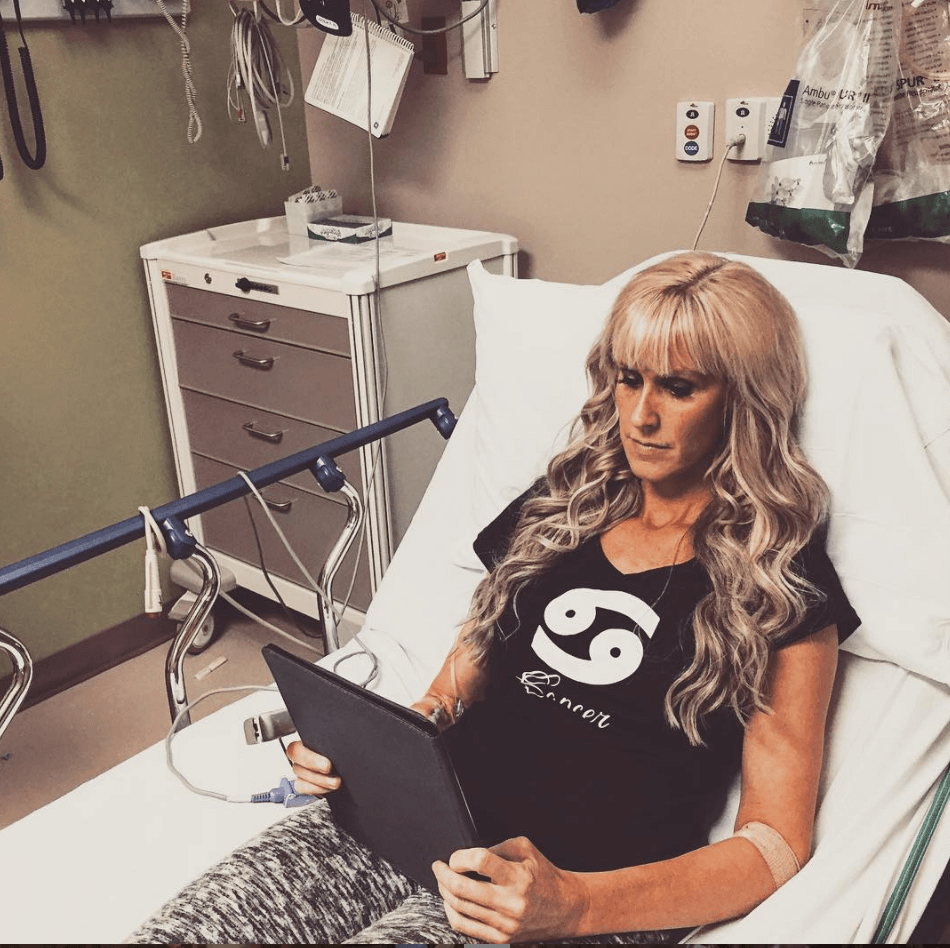
Melissa’s Stage 3 Multiple Myeloma Story
Melissa shares her stage 3 active myeloma story, along with undergoing in vitro fertilization (IVF) before her treatment. She details going through the RVD regimen, with Revlimid, Velcade and dexamethasone for 7 rounds.
In her story, Melissa also highlights navigating quality-of-life issues, from dealing with cancer’s impact on her marriage, how to be a parent, the importance of self-advocacy, and the most unexpected hardship of all: financial toxicity in trying to pay for cancer treatment.

- Name: Melissa V.
- Diagnosis:
- Multiple myeloma (active)
- »MORE: What is Multiple Myeloma and How is it Treated?
- Staging: 3
- 1st Symptoms: Infections
- Treatment:
- IVF treatment
- Retrieved one egg that turned into an embryo
- Regimen: RVD
- Immunotherapy: Lenalidomide (Revlimid)
- Targeted therapy: Bortezomib (Velcade)
- Steroid: Dexamethasone
- 7 rounds; infusions twice a week for three weeks, one week off
- Stem cell collection (for potential future transplant)
- IVF treatment
The one thing that I tell people is that it will be okay. You will be okay. Don’t be overwhelmed even though that’s hard to do.
Don’t ever give up hope. There’s always hope. Never give up the fight. It’s tough because myeloma is a tough fight, and I’ve been there, but never give up. Always fight.
Melissa V.
- Diagnosis
- Fertility
- Treatment Plan
- Remission
- Prep for Stem Cell Transplant (SCT)
- Support and Family
- What was the lowest point for you mentally and emotionally?
- What helped you in your lowest moments?
- How important was it for your to have caregivers?
- How did the cancer affect your relationship with your husband?
- Do you have advice for other couples going through cancer?
- Parenting with cancer
- Did you have to hire outside help for your son?
- Any advice for parents who are going through cancer
- Reflections on Cancer Treatment
- Advocating for yourself as a patient
- Advice about being your own advocate
- How did you deal with the hair loss?
- Did you work through treatment?
- Financial toxicity: paying for cancer treatment
- What do you wish you had known at the beginning?
- What is your “new normal” after cancer?
- What’s your advice for someone who has just been diagnosed with multiple myeloma?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
I got sick a lot. It started out with pneumonia. A few months later, I got sick again. It turned into pneumonia again. I had a really hard time recovering from it.
It was really strange to me because I’d always been really healthy. Within 6 months, I was diagnosed with pneumonia three times. That was really unusual for me. I got strep throat, bronchitis and ear infections. I was getting infection after infection, and I knew something was wrong.
That’s the first time I set up an appointment with a doctor to get a physical. I thought it was strange that I was getting sick so much. That was the biggest red flag.
I even felt like I maybe had leukemia, but it wasn’t showing up in my blood work, so I suspected multiple myeloma before I was diagnosed.
What do you remember about going to the doctor the first time?
Initially, when I went to my primary care, she kind of dismissed it. My son was 12 months old at the time. He’d been in daycare for 6 months before this, but she blamed it on the daycare.
I started having other symptoms around the time I went to see her. I had a fever of 102 the day of the physical, so she couldn’t complete the physical. My symptoms were advancing, so she started sending me to a bunch of different specialists.
Finally, it was a hematology oncologist who ultimately diagnosed me with multiple myeloma. Typically, multiple myeloma is diagnosed within the geriatric population.
She had never dealt with a case like mine, so I took it upon myself to switch to a myeloma specialist at one of the major hospitals in Dallas.

Were there any misdiagnoses?
They were thinking Lyme disease. I had fevers, so they were thinking infectious disease at first. They were trying to rule that out.
All my doctors were basically saying, ‘This is above my pay grade,’ and didn’t know what was going on. I kind of had a feeling, though, so I was the one who pushed for a hematologist.
I’m an occupational therapist, and I’ve been in the healthcare field for 15 years. I’ve worked with multiple myeloma before. I knew the only two cancers that cause frequent infections were leukemia and multiple myeloma.
Leukemia wasn’t showing in my blood work. Myeloma is a difficult cancer to diagnose because it won’t necessarily show up in your blood work, and I knew that.
I had a gut feeling. I even told my parents I thought I had multiple myeloma. I dismissed it, but I had a feeling.
What was the appointment with the myeloma specialist like?
They already knew I had multiple myeloma because I had already been diagnosed by the hematologist. She “prescribed” me with a bone marrow biopsy.
She didn’t know how to treat me. She wasn’t up to date with all the new treatments for myeloma. That’s why, even though I loved her, I switched to a specialist. They re-did all my tests, including the bone marrow biopsy.
What is a bone marrow biopsy like?
The first one I had, they put me out. When I switched hospitals to the myeloma specialist, that’s something they do all day long.
You go in, they numb it, take a big drill to your hip while you’re lying on your stomach, and it was quite a different experience. They can give you some Ativan if you need it.
I’ve had 5 bone marrow biopsies total. They just take a sample from the back of your hip. It’s definitely not super fun, but it’s not horrible.
Usually, I was down for a couple of days repairing from that. There’s some pain associated with it. I just had to rest and take it easy for a few days.
How did you process the cancer diagnosis?
I still remember when she came in that day. She just put her hand lightly on my shoulder. She said, “You have multiple myeloma.” I responded by saying, “Yeah, I know. I’m not too surprised by that.”
My attitude was mostly, ‘What’s next?’ I wanted to know the next steps and how to treat it. I’ve heard a lot of people say they’re shocked when they hear their diagnosis.
I think it was no different for me. Even though I thought I knew, it’s different when you actually hear it from the doctor. I went numb and into fight mode.
»MORE: Processing a cancer diagnosis
How did your loved ones handle the diagnosis?
I had already told my parents I thought I had myeloma. When I told them, they were very upset. They broke down and were very scared. When you Google myeloma, it can be a very scary cancer to have.
My husband was shocked that I had to begin treatment right away. Everyone was in shock really.
»MORE: Breaking the news of a diagnosis to loved ones

Fertility
Preserving fertility before treatment
I always wanted another baby. Jackson is my kid. I never wanted kids before him, but he was a pleasant surprise.
Ironically, we had planned on having another kid around the time I was diagnosed. My first reaction was, ‘Am I going to be able to have another kid once I started treatment?’
My oncologist and the fertility specialist said most likely I wouldn’t.
I went through IVF right after my diagnosis. That took about a month. It was an intense process. I got one egg and one embryo. I did get one embryo. I started treatment immediately after that.
Can you talk about the IVF process?
That was probably one of the hardest parts. It was such a rushed process. We didn’t have to research and look anything up. We just knew we wanted to have another baby, so we went to a fertility specialist. He just told us the steps. I remember feeling pretty numb and thinking, “Okay, I have to give myself some shots.”
It was a super emotional experience because the doctor said he thought we would at least get 11 eggs. We thought we’d have an easy time with it.
They do a sonogram every other day, and the news was the same every time: “You don’t have any eggs yet.” That was an emotional rollercoaster. By the end of it, he gave me a less than 7% chance of that turning into an embryo.
»MORE: Read a patient’s detailed IVF journal
Paying for IVF
It was a $15,000 expense, so we didn’t know what to do. We cried in the parking lot and decided to go with it because we didn’t want to wonder.
We put our deposit down, and my husband lost his job. We had less than a 7% chance of having an embryo, my husband lost his job, I was about to start treatment, and we didn’t have any health insurance. It was a trying time.
We waited for a week, which felt like forever. He called and said, ‘It worked. You got your miracle embryo.’

Treatment Plan
Describe the treatment plan
They gave me a high dose of steroids, an immunotherapy drug and chemotherapy. We did them simultaneously for 7 rounds. The goal was to do them for 4 months, and then I would go through a stem cell transplant.
However, my myeloma specialist knew that I wanted to have a baby, so he said we could do treatment for a longer period of time and instead of doing a stem cell transplant, I could try to have my baby and then do the transplant.
Immunotherapy (Revlimid)
The immunotherapy drug is called Revlimid. It’s a common drug in the myeloma community. It was kind of mainstream at the time. I’m not sure which side effects it caused because I was on two other drugs, but I know that typically, it can cause some GI issues, as well as fatigue and neuropathy.
I did experience all of those, but I don’t know if that was from just the Revlimid or the other drugs, too.
The steroid is just a pill. It’s dexamethasone. Velcade is the targeted therapy chemo, and it’s an infusion. I didn’t need a port or PICC line.
I was on a high dose of Velcade, so I would go in twice a week to get infusions. I would take Revlimid every day, and I would take the steroid the day of the infusion and the day after. I did that for 3 weeks, and then I would have a full week off from treatment. I was in the hospital for about 5 hours every time I went in.
Can you talk about the side effects you experienced?
All the drugs I was on except the steroid can cause neuropathy. That was a huge thing for me. It’s tough when you’re going through any kind of treatment because fatigue and nausea are huge side effects you have to battle. I had a lot of GI issues.
Exercise was something that I’ve always done, thank goodness. Going into treatment, it wasn’t as hard for me to do it. I would just walk a lot.
Dexamethasone is called “roid rage” in the myeloma community because you’re taking so much of it. I sometimes felt like the steroid caused the worst side effects because it’s just such a big dose in a week. I would get really anxious and be up all night long. I sweat a lot.
I even remember telling my husband, ‘It’s not personal. I’m gonna go up to the room and shut the door because you’re irritating me.’ It was definitely not personal. I could tell I felt different because of the steroids.
The night of my infusions, I would be really sick and nauseous. I would take some Zofran to help with that. There was really just no helping it, though. Nausea was a big problem.
Unfortunately for me, I’ve never eaten a lot of sugar, but I would crave sugar. One of the side effects of the steroid is an appetite. I craved so much sugar. Interestingly enough, I had lost a lot of weight prior to my diagnosis. Through treatment, I didn’t gain a lot of weight because I was very careful with what I ate, but I had so many cravings.
A lot of people in the myeloma community say they gain a lot of weight during treatment. It was kind of a balance of being nauseous and craving things. When I was nauseous, there wasn’t really much to help it except maybe bananas. I ate a lot of bananas.
»More: Read other patients’ experiences with side effects
In and out of the hospital
I’ve been in and out of the hospital. It’s been more for my neuromuscular issues and trouble breathing, which they thought was caused by my myeloma initially. For the myeloma specifically, I’ve only been hospitalized once. I have been hospitalized a few times throughout the process. It’s not been easy.
Everything revolves around my son. I just wanted to make it easier on him. It was hard for me to leave my life and stay there. Journaling always helped, but it was really hard to be away from my son.
When he would come see me every day, we made it a very fun time. We ordered lemonade and chocolate cake. Now, he actually likes it when I go to the hospital because he can get lemonade and chocolate cake. That lifts my spirits for sure.

When did you get blood work and scans?
Each month, before the next round, I would get blood work done. They test for a monoclonal protein. That measures the amount of cancer in your blood. They performed the scans and did the bone marrow biopsy at the end.
Remission
Do you remember the moment you were told you were in remission?
They put me in a small room with a table. I had to wait there for my doctor to walk in, and I knew he had the results. It was excruciating.
I played a mean trick on my husband. He went to pick up one of my best friends, who was going to meet us at the hospital.
My specialist came in, and my husband hadn’t made it back yet. Of course, he told me I was in remission. I was very overwhelmed.
My husband came in toward the end of the appointment, and I decided to play a trick on him. I had my specialist tell him that things didn’t look good and there was a turn for the worst. Of course, I was just kidding, and that was a great day and moment.
What happened after your treatment ended?
The interesting thing about my story is that I actually achieved remission at the end of my treatment. That’s not typical. In fact, my myeloma specialist didn’t think I would achieve full remission.
He just wanted to get me as close as he could. Not everybody achieves full remission even after a stem cell transplant, but it’s more likely that you will after a transplant. Multiple myeloma is not a curable cancer, so a transplant will just get you more time as far as remission.
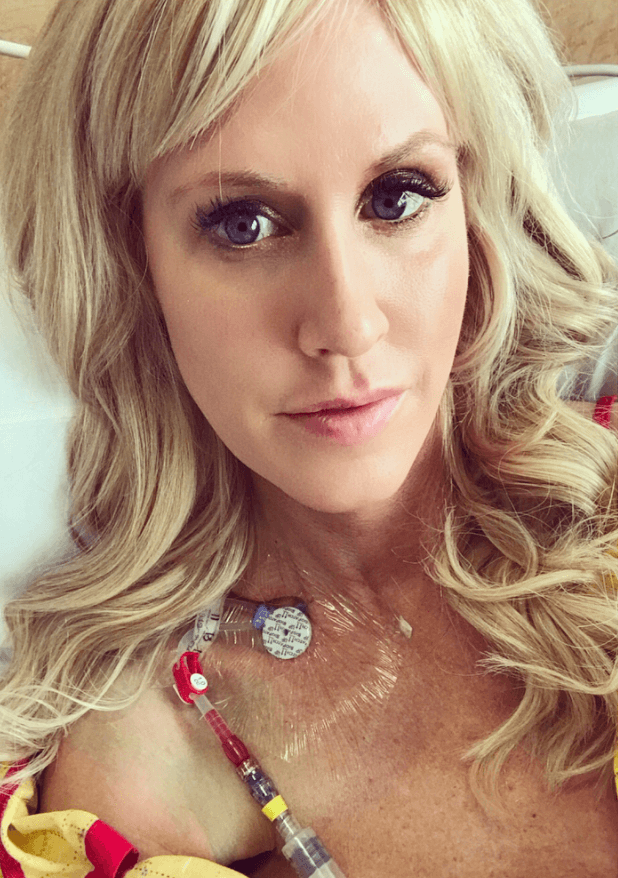
Prep for Stem Cell Transplant (SCT)
Stem cell collection
In my case, it was really unusual that I achieved full remission. I was really excited. The plan was to have a baby after that, but I did stem cell collection first.
They collect your stem cells so that in the future, they can use your own stem cells for the transplant. If you use someone else’s, it can cause a lot more complications.
Describe the stem cell retrieval
Typically, it’s so easy for people to do. For me, the process was a little more excruciating because I’d been in treatment for 7 months. My bone marrow was pretty damaged.
When I did the collection, it was very painful. They give you Neupogen shots, which increases the white blood cell count in your bone marrow.
If you can imagine everywhere you have a bone, that’s where I had pain. They had to give me multiple shots because I wasn’t producing enough.
The first day, it was7 hours of trying. My blood counts went down, and I didn’t do very well. It was just not a fun process for me. I ended up staying in the hospital for 5 days. My goal was to get 9 million, but I only got 6. I did get enough for two future transplants, though.
What is like living with a chronic illness?
I never thought I would be in this position. I always was so healthy and prided myself on that.
It is sort of surreal to find myself living with a chronic illness that will eventually turn terminal. There is no cure, so it’s manageable until it’s not manageable anymore.
I’ve seen some of my friends who I’ve connected with not get to live as long as I have. I focus on that, but I’ve learned to not focus on that as well.
I’m grateful for my life and every day that I have, but at the same time, I don’t live my life as though I’m thinking about my illness all the time. I don’t want it to consume my life or my thoughts.
You almost have to learn how to live with it and without it. You don’t want it to always be in the forefront. You’re not going to enjoy your life if your illness is all you think about, so you manage it.
It’s like the cancer itself. You learn to manage it. It evolves. Everyone is different in how they cope, but for me, it’s really helped to focus on my son and husband and even helping other people.
I live my best self. What would be my best self even with sickness?
I’ve always loved exercise. I’ve never stopped that. I’ve never given up on my dreams. I still want to have another baby. I’ve not stopped living my life. I’ve been able to work still even if I’ve had to cut back. I’m still living my life to the best of my ability.
Support and Family
What was the lowest point for you mentally and emotionally?
It was month 4. My numbers weren’t budging at that point. I remember thinking I wasn’t going to even get close to remission.
I was going through everything, and the anxiety of getting those blood counts back just exacerbated the feelings. For a few months, the numbers weren’t moving at all. I got a little frustrated.
What helped you in your lowest moments?
It was a combination of everything. The biggest thing I’ve learned is it’s okay to be sad or frustrated. You have to let yourself feel those things, because it’s impossible to always feel great.
Know that it’s not good to stay in that place for too long. Everyone copes differently, but for me, having emotional support and reaching out was helpful.
Also, helping others. Sometimes, if you take yourself out of the equation, it can really help change your focus and your mindset. It can help you be more hopeful and not so discouraged.

How important was it for your to have caregivers?
I realize I’m super lucky. I realize that so many people don’t have the support of a spouse. Even through this difficult journey, sometimes people lose their spouses.
My husband and I had only been married for 3 years. Having his support meant everything. I’m not physically close to my family. They’re kind of all spread out.
Having the support of my community was great. Neighbors even stepped up. My family has always been willing to come out if I needed them.
Myeloma isn’t really a common cancer for someone my age. It’s tough for people to relate sometimes, so I belong to a couple of support groups. One is specifically 50 and under. There’s a small group of us, but that has really helped with resources and support because it’s a rare cancer.
»MORE: What kind of support cancer patients say helped the most
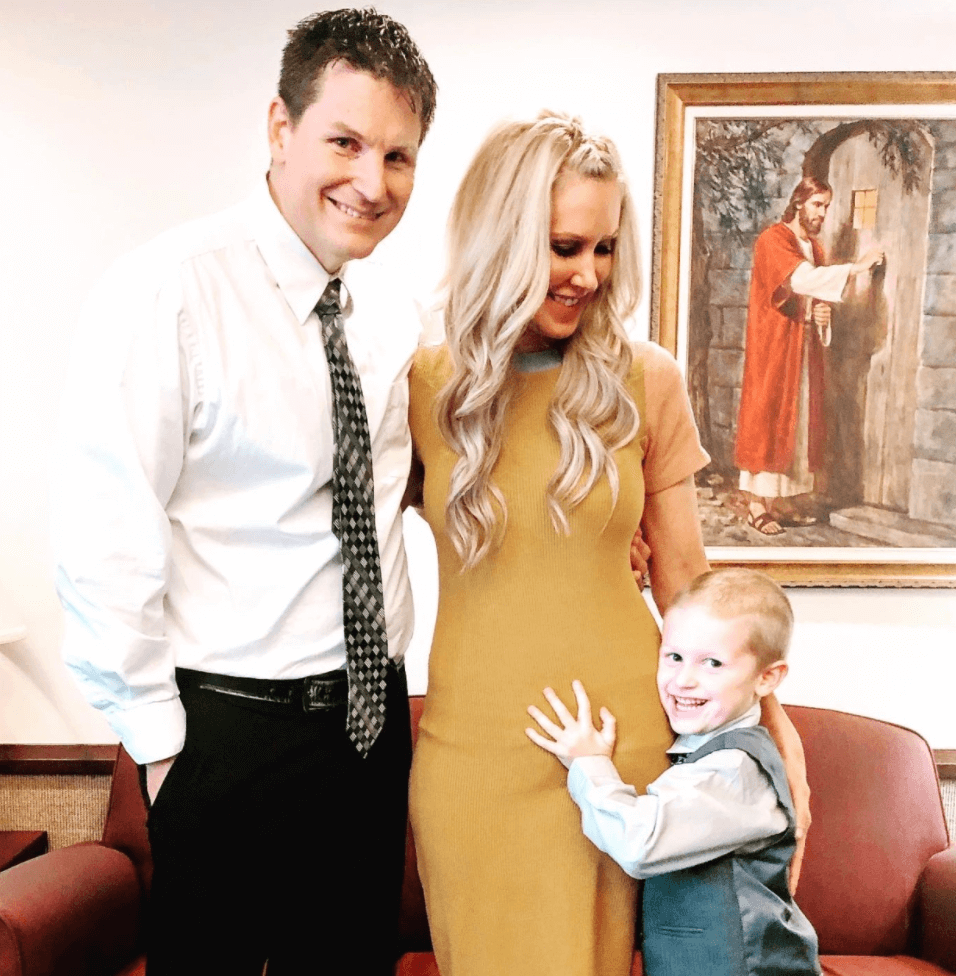
How did the cancer affect your relationship with your husband?
It affected us both. It put a lot of stress and strain on our relationship because the relationship we once had was now forced to change.
Unfortunately, he became more of a caregiver while I became a patient. I didn’t like that position. I think it brought out a lot of insecurities in me, especially being in a newer marriage.
It also has made us stronger throughout the process because we’ve had to get through us. We’ve been able to turn to each other and rely on each other. I trust him more. It’s made our connection more solid.
Do you have advice for other couples going through cancer?
Something I’m a huge fan of is counseling. A diagnosis is uncharted territory. There’s just as much stress on the caregiver as there is for the patient.
We chose to go to counseling so he could help us navigate the best ways to communicate.
We wanted to grow with the experience rather than let it tear us down. It was a great move for our family. I would recommend it to others for sure.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
Parenting with cancer
My son wasn’t even a year old when I was diagnosed. It’s been a lot harder on me than it has been on him.
I’m very aware that I can’t be the mom that I want to be or that I know I could be. That is my own personal struggle. He’s too young, and all he knows is me being sick actually. That’s all he remembers and knows. He’s just starting to form memories.
He knows Mommy is sick, and he actually helps me if I’m having a bad day. If I’m on the couch, he’ll go get me some water or something. He’s so cute.
I was in and out of the hospital, and that was affecting him even at 3 years old. He began experiencing some anxiety that he wasn’t before. He had been sleeping through the night, but then when I went to the hospital, he started having some anxiety. It would show itself at night, and he’d be asking, “Where’s Mommy? Where’s Mommy?”
We have a little book. My husband’s best friend is a children’s book author and created this book for us. What we’ve done is said, “If you want to talk about Mommy going to the hospital, let’s read this book together.”
He actually has done that a few times now. We read about it and talk about how he’s feeling. He’s so little, so he can only understand concrete feelings. I ask, “Are you happy? Are you sad?” He can verbalize how he’s feeling a little bit in a child -appropriate way with that book.
Did you have to hire outside help for your son?
Luckily, we’ve had him at school. He’s been taken care of at daycare during the day. My husband has a flexible enough job that he’s able to take off early if he has to.
We are really blessed that way. We have our church, and they’ve been a whole community on their own always willing to help us. We’ve had people we trust who were able to watch him, so we haven’t had to hire any outside help.

Any advice for parents who are going through cancer
Kids are really resilient. They understand more than you realize they do.
It’s really important to realize where you can be child appropriate with them and help them understand what’s going on.
Give them a lot of reassurance. Counseling has actually been helping us with that as well. It’s helped us navigate ways to talk to him about it. Everyone’s situation is so unique.
Having the support of family, friends, community and church has really helped us. It just depends on your child’s needs and their age.
Find what works best for your family. It can take some trial and error to do that, and that’s okay.
»MORE: Parenting during cancer treatment
Reflections on Cancer Treatment
Advocating for yourself as a patient
I had to advocate the whole time. I’ve always been on the other side. I’ve always been a healthcare professional. I’ve seen other patients have to fight for themselves and have difficulty getting a diagnosis.
I never in a million years thought I’d find myself there. I was fighting to get a diagnosis. I remember telling my primary care physician that I needed a referral to an oncologist. She was very hesitant. She didn’t put in an urgent referral, but I felt the urgency.
It takes a lot of strength from a patient perspective to push and advocate for yourself, especially when you know there’s something wrong with your body after you’ve been healthy your whole life. Even if a doctor dismisses you, you have to keep going even if that means finding a different doctor.

Advice about being your own advocate
Sometimes it helps to bring someone who might be a little stronger than you who might be a good advocate. Sometimes I hear patients say, “Maybe I’m going crazy. Maybe it’s just me.”
If you bring someone you know and trust, maybe they can advocate for you and they’re in a better place to fight for you.
There’s nothing wrong with switching doctors. Doctors are fallible and human just like we are. They make mistakes. Sometimes it takes another doctor to find what’s going on.
It’s a grueling process for a patient because it’s hard to know who’s going to be a good doctor. I don’t like going to doctor’s appointments, but if it means feeling better and getting a correct diagnosis, then it’s important to push forward and keep going.
How did you deal with the hair loss?
It was annoying. I didn’t like it. I wasn’t going to shave my hair. I was grateful that I didn’t have to since I didn’t lose all my hair.
Even if I did, though, wigs are great these days. I probably would be okay with it, but I don’t know.
I probably will have to deal with it at some point because a stem cell transplant is looming in my future. I’m grateful that it’s pretty easy to wear wigs these days.
»MORE: Dealing with hair loss during cancer treatment
I tell my husband, ‘You get two women with me.’ He has the one that has a full head of hair, and then I can take the extensions out and he has a whole other woman.
Did you work through treatment?
I was a manager, so luckily I was able to work from home a lot. With the type of cancer I have, I realized it’s just too hard for me to maintain a full-time job. I quit my job more than a year ago now.
Now, I work with a company that lets me come in if I feel good that day. I’m PRN, which is basically “as needed.” I had to scale back what I did because I have a very physical job.
»MORE: Read more on how others dealt with work after a cancer diagnosis
Financial toxicity: paying for cancer treatment
That’s actually been the most unexpected trial we’ve experienced.
Financially, we were doing really well. My husband lost his job and our health insurance the day we decided to do IVF. That’s actually turned out to be a blessing in disguise. Prior to that, we had found out that there was a cap on his insurance for stem cell transplants, so I wouldn’t have been able to do that.
To change insurance, we needed a major life event. We were even thinking of divorcing for a minute so we could change. Then he lost his job, so that ended up being good because he found another one with better insurance.
The expense from cancer isn’t really talked about enough. Realizing that we went through our life savings and not having a lot of time to recover from that has been hard. It can be a huge burden.
Since my husband lost his job, I was able to go through the Leukemia & Lymphoma Society, and they sponsored my treatment for 6 months. The day I found that out, he found out he got his new job, so that was huge.
I’ve done a couple of fundraisers. I did one recently to be able to go to Mayo.
There are payment plans for every hospital. They want their money, so they’re usually open to working with you. It is a huge burden, though, so it’s good to know your options and what your resources are.

What do you wish you had known at the beginning?
I wish I had understood my cancer and what exactly the treatment would entail.
I knew what multiple myeloma was, but I didn’t really know treatments and options that I had that I know now. It took some time and research. Connecting with people who have already gone through this experience is what helped me the most.
When I was first diagnosed, it was a very overwhelming experience. I wish I hadn’t worried so much about it. You don’t need to know everything all at once.
You come to know things as you need to. I wish I had known not to worry so much about everything. I wish I could’ve just let things evolve and have faith in that.
I wanted to change my diet and my whole life because I had this cancer that’s incurable. It was just a lot.
What is your “new normal” after cancer?
I don’t know if I would have been different without the experience. It’s like I almost forgot who I was and have become a new person because of it. Sometimes I wonder if I’m completely new or if I’m just a better version.
With my son, I embrace every single moment with him. At night, we have “talk time.” We talk about our day, and he really looks forward to it. He always says, “Mommy, can we do talk time now?”
I really make a conscious decision to enjoy moments. Every memory that I make, I’m very aware of it. How I treat other people has changed. When I walk down a hallway, I want every person to feel good about themselves — especially when they’re in my presence.
A lot of people wouldn’t know just by looking at me that I have cancer. The truth is, we can look at someone and not know what they’re going through or that they’re going through anything at all.
I treat people like they are going through something, though, because we all go through things. I try to treat people like they’re the most important person in the world. It has definitely changed my perspective and how I think about those kinds of things.
What’s your advice for someone who has just been diagnosed with multiple myeloma?
The one thing that I tell people is that it will be okay. You will be okay.
Don’t be overwhelmed, even though that’s hard to do. Don’t ever give up hope. There’s always hope. Never give up the fight.
It’s tough because myeloma is a tough fight, and I’ve been there, but never give up. Always fight.

Inspired by Melissa's story?
Share your story, too!
Multiple Myeloma Stories
Clay D.
Diagnosis: Multiple myeloma
1st Symptoms: Persistent kidney issues, nausea
Treatment: chemo, radiation, stem cell transplant
...
Melissa V.
Diagnosis: Multiple myeloma, stage 3
1st Symptoms: Frequent infections
Treatment: IVF treatment & Chemotherapy (RVD) for 7 rounds
...
Elise D.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: Lower back pain, fractured sacrum
Treatment: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P.
Diagnosis: Multiple myeloma, stage 3
1st Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatment: Chemotherapy (Bortezomib/Velcade), Daratumumab/ Darzalex, Lenalidomide, Revlimid) and stem cell transplant
...
Ray H.
1st signs: Hemorrhoids, low red blood cell count
Treatment: Immunotherapy, Chemotherapy, Stem Cell Transplant
...
Valarie T.
Symptoms: Nose bleeds, fatigue, back pain
Treatment: Chemotherapy, stem cell transplant
...
Julie C.
Symptoms: Queasiness, food aversions, lack of appetite, fatigue
Treatment: Stem cell transplant, chemotherapy (D+PD), bispecific antibodies (talquetamab & cevostamab)
...
Laura E.
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
...








One reply on “Melissa’s Stage 3 Multiple Myeloma Story”
Hi, Glad for your outcome and hope it holds! I was diagnosed in 2008 with smoldering MM. Went active in 2011 as high risk MM. Tandem stemcell transplate and 3 years of maintenance. I achieved stringent complete remission immediately after the transplant. Been there ever since. According to the doctors at UAMS with high risk and no relapse within 5 years I probably won’t see MM again. The said this is 10 years with low risk as it’s less aggressive. Go figure. The point is hang in there, keep a positive outlook and know that it’s possible you may never see MM again. Regards