Ray’s Multiple Myeloma Story
Ray was diagnosed with multiple myeloma. He shares his story and how he found out he had cancer starting with a routine CBC blood test. He stresses the importance of going to your doctor for routine checks, his experience with stem cell transplant, and learning how to accept help from family and friends.

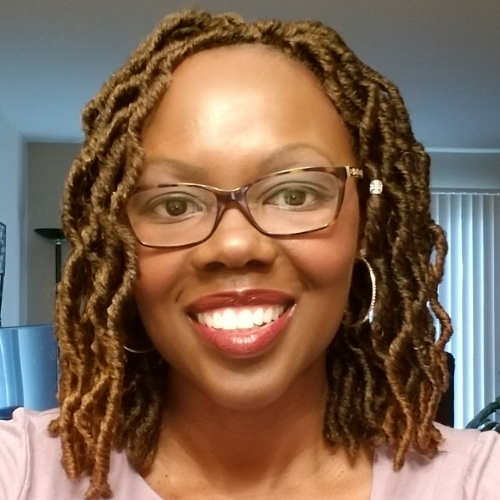
- Name: Ray H.
- Diagnosis:
- Multiple myeloma
- Initial Signs: Hemorrhoids, low red blood cell count (a bit anemic)
- Treatment:
- Immunotherapy: Revlimid, Velcade, Dexamethasone
- Chemotherapy: Cytoxan (Cyclophosphamide), BCNU (Carmustine), Melphalan
- Stem cell transplant
- Maintenance Regimen:
- Revlimid
- Velcade
My cancer diagnosis is a big part of me now… Cancer hasn’t taken away my life and parts of my life. It’s enriched my life
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Pre-Diagnosis
Tell us about yourself
My cancer diagnosis is a big part of me now. I’m a marketing writer. I’m also a musician. I live in the Bay Area, been married for a really long time, 27 years or so. Have two children — [a] 25-year-old daughter and our 23-year-old son — and [I] was diagnosed with multiple myeloma [in March 2019].
Looking back
Sometimes, time goes by pretty quickly. Part of that may be going through the pandemic and all the disruptions that we’ve had in our professional, personal, and social lives; that seemed like a long time. When you start hitting anniversaries, all that seemed kind of a fast year.
When it relates to my cancer diagnosis, looking back on some of the treatments like during stem cell transplant, time seemed to move pretty slowly.
Now, I’m 20 months out [from] having my stem cells reintroduced to my body, that seems pretty quick, a year and a half’s gone by.
Routine CBC came back. They said, “It’s a low red blood cell count. Let’s confirm it. Something weird could go on.”
First signs
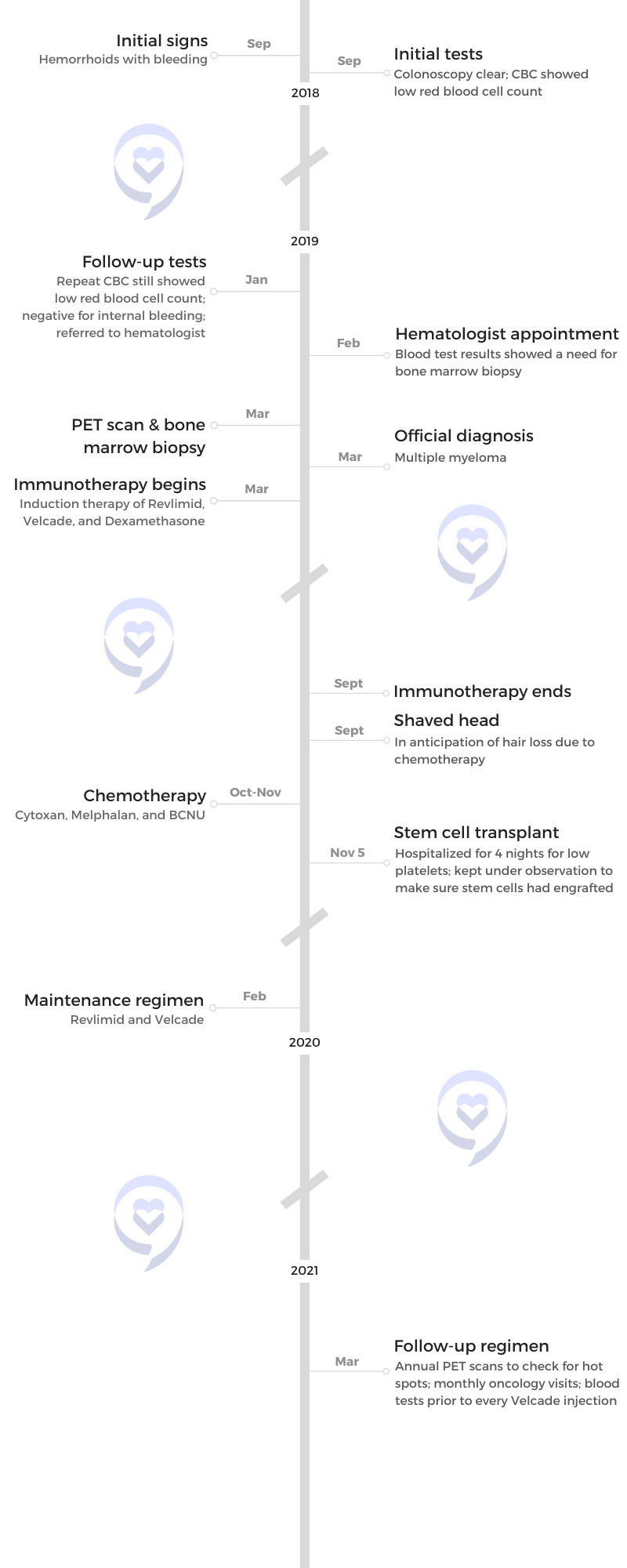
I, for years and years and years, have been a cyclist to keep me in shape and allow me to eat whatever I want to eat and drink whatever I wanted to drink. I, like most cyclists, would keep performance metrics. In 2018, my metrics as a 54-year-old were every bit as good as they were in my late 40s. I was a beast on the bicycle doing fine.
Oddly enough, though, I was having problems with hemorrhoids; not so much with pain, but with just blood. I went to my gastroenterologist [and] had a colonoscopy [in early] 2018. He mentioned, “You have hemorrhoids,” and just went on to [talk] about the results from my colonoscopy. I [wanted to know] more about these hemorrhoids. [He said,] “Don’t worry too much about the hemorrhoids. It’s not going to turn into cancer or anything like that.” But I [wanted to] know [if] it’s [going to be] a problem for more advanced treatments. [When he asked] what the symptoms [were, I said] I have blood. Then [my doctor said,] “Why don’t we just do a quick little blood test? Routine CBC.”
That routine CBC came back. I was a bit anemic. My red blood cell count was 11-something. They said, “It’s a low red blood cell count. Let’s confirm it. Something weird could go on.”
I can be diving into a deeper pool than I want to be diving into.
Testing
Before I could get it confirmed, I got into a bicycle accident and broke my eye socket so it took me a little while. I had a lot of things on my mind, other things I was getting prepared for, the holidays… Just natural procrastination.
[In] January 2019, I went back for my follow-up blood test and it also was anemic. In fact, a little bit more anemic. He said, “You are definitely anemic. Let’s see why. Let’s run another blood test [that’s] a little bit more sophisticated to see. Perhaps [there are] some indications that there might be internal bleeding.” That came back still anemic but negative to those indicators that might have internal bleeding.

At that point, he’s like, “We’ve gone as far as we can go from a gastroenterologist type of perspective. Time for you to go to a hematologist.” He referred me to one and that’s when I found out that, looking her up online to make an appointment, hematologists are oncologists. That’s the first time it came to my head. There might be something a little bit more to this.
Around February 2019, [I] have an appointment with my hematologist-oncologist. That was probably a four-week, five-week process as we began to work down what was causing my anemic condition. After a couple of weeks and a couple of tests, we knew it was probably something. Then after that, a bone marrow biopsy was the one that confirmed her suspicions of multiple myeloma.
‘Time to go to a hematologist.’ It came to my head. There might be something a little bit more to this.
Seeing a hematologist-oncologist
I had worked for a drug company a long time ago. I knew hematology was [the] study of blood, but I have a sneaking suspicion that most hematologists are also oncologists.
Looking up my doctor and seeing the oncology next to her was a big shock. I don’t think I’d even been thinking about it as a possibility. I don’t know what could have been the cause of my red blood cells being low but cancer wasn’t high on the list. I can be diving into a deeper pool than I want to be diving into, and that was the first kind of hint that that was going to be the case.
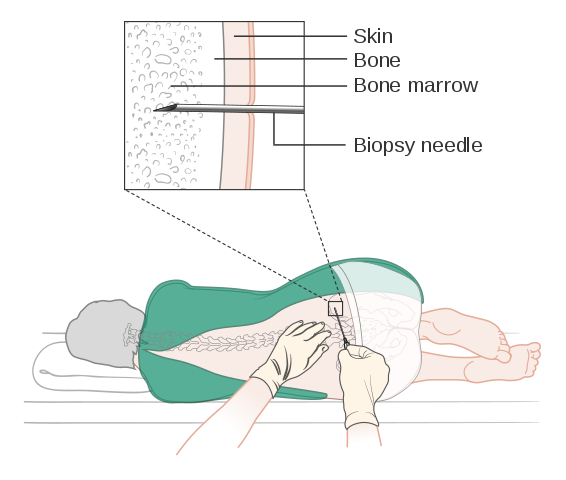
Discussing the bone marrow biopsy
My wife and I are sitting in a doctor’s office. She goes, “Next step, we’re going to do a bone marrow biopsy.” I give it a resigned chuckle and a roll of my eyes. She’s like, “What’s that about?” And I’m like, “Come on, doc. The bone marrow biopsy test comes with a reputation, right? There’s some baggage that comes along with it.”
What I tell people that ask me about my bone marrow biopsy experience is you don’t want to consider it recreationally. It’s a painful thing. You just got to suck it up and get through it. Thankfully, it doesn’t last long because [it’s] uncomfortable.
A bone marrow biopsy was the one that confirmed her suspicions of multiple myeloma.
Getting through the bone marrow biopsy
I’ve had two different bone marrow biopsies and two different approaches to it. The one that I had in my doctor’s office was straight old pushing the needle. I had another one at the Cancer Center at Stanford University. They used a drill. Scary sounding, but it didn’t hurt as much. It was also my second one, so I kind of knew what was going in.
My advice is [to] try to breathe [and] focus. Some people take themselves to their happy place. Find a spot in the wall that you stare at, but it’s critical that you be still. There’ll be probably a second person, an attendee at the biopsy, to hold your ankles down and keep you from rotating. It’s important to stay still and get through it.
[In] my initial bone marrow biopsy, they discovered that 90% of my bone marrow was cancerous.
The worst part of the pain is not just the injection, but it’s also the, for lack of a better word, dissections and taking the bone marrow out. I think that may have helped the second time around. I had less cancer in my bone marrow. It was a little easier to draw out so maybe that contributes to [feeling] less pain.
[In] my initial bone marrow biopsy, they discovered that 90% of my bone marrow was cancerous. All this came from a simple CBC test, something that you should be getting once a year when you see your doctor. If you do not go to your doctor, you’re doing yourself a disservice. I was performing exceptionally well on my bicycle. I was feeling great, yet I had 90% of my bone marrow cancerous and I was anemic.
Even if you’re just a patient caregiver, take care of yourself. Go to the doctor. It’s rule number one. Go get your CBC. For me, that’s the only reason I was diagnosed and I was diagnosed way before multiple myeloma could become much more problematic.
A lot of multiple myeloma patients get diagnosed with bone fractures; frequently, compression fractures of the vertebrae. There’s a patient in my support group who woke up one morning [and got] compression fractures in three of his vertebrae, lost about two and a half inches of height in his first two steps out of bed. The bone marrow is so cancerous [that] it had gone into the bone, weakened the bone, and then had that fracture risk.
Blood test results
From my first anemic test, it was a little worse [going into] the second one. The third follow-up was close to the second, so it was about the same.
Within starting treatment, my first or second blood test after [showed] I wasn’t anemic anymore, so I did see immediate results.
Dealing with scanxiety
I never had scanxiety before because I was always expecting them to be normal. But then once they started becoming abnormal, there’s the anxiety even heading up to get it. What are the numbers going to be? Are my cancer markers back? Are they higher?
I’ve had a closed MRI before and an open MRI for athletic injuries. Closed MRIs [give me] much more anxiety because it’s extremely claustrophobic. The open one’s different. The PET scan, [even if it was] still exploration, [you] wonder what it’s going to come back at, [if] there literally [will be] holes in my bones that require an escalated treatment.
I went to a group very early. I got diagnosed [on] March 11th. My first group was the very next week. I learned about anxiety because people say, “I’ve got this test coming up,” and now everyone’s worried about what’s the number going to be. Everyone’s got a number in something and they want this number to be within range or lower or what have you. There’s a lot of anxiety that comes with that. It’s helpful to talk about it and find out that you’re not the only one who feels that way.

It’s helpful to talk about it and find out that you’re not the only one who feels that way.
Diagnosis
Getting the official diagnosis
It came a bit more of a shock to my wife. She had been in all my appointments ahead of time. But in the research that she was doing, I think she was hopeful. She was thinking [it] was like a smoldering case of multiple myeloma.
I was not going to Google because I know what head game that could be. I knew that it wasn’t going to change anything. All that work I would do in between my bone marrow biopsy and my doctor’s consultation afterward, nothing I could do within that is going to change what my approach would be from that very moment of my diagnosis forward.
All this other stuff didn’t really matter. I wanted to compartmentalize and work with what I knew and what I could do. I didn’t want to think about all the various possibilities. It’s just [how] I’m wired.
My wife Lori is a little bit different. I came in and because of the conversations that we [have] had, it was probably going to be lymphoma or multiple myeloma.
Nothing I could do within that is going to change what my approach would be from that very moment of my diagnosis forward.
I, at that time, was tired of being picked on. I was getting poked and prodded. I don’t particularly like needles to begin with. I had given a lot of blood [and] had the bone marrow biopsy. I sat across [from] my doctor and said, “Doc, I feel as though I’m like a fighter in a ring and I’ve been taking a whole bunch of punches. Tell me what it is and let’s start swinging and punching back.” She looked at me and said, “All right. You’ve got multiple myeloma.”
Going into that ahead of time, if you’re thinking it’s lymphoma or multiple myeloma, there’s one that is incurable, there’s another one treatable, and there’s another one that is curable. Treatable, curable, but also potentially [with] the mortality rate higher. What do you even hope for? Which way do you want that coin to land?
I feel as though I’m like a fighter in a ring and I’ve been taking a whole bunch of punches. Tell me what it is and let’s start swinging and punching back.
She told me it was multiple myeloma. [It] came as quite a shock. My wife was very strong in the office but when she got back [to] the car, she immediately started crying. We’d been warmed up to the process that it was going to be something, so it wasn’t just out of the blue.
Both of us, in some way, knew that something was coming. It turned out to be more significant than my wife was anticipating for me. I didn’t have an idea about levels. It was more binary, yes or no. We already knew it was going to be yes, so now it’s just which yes is it.
Multiple myeloma as a chronic illness
Even before the official diagnosis, she let me know — chronic disease, incurable yet treatable. I still remember that. It was known even before I was officially diagnosed.
Both of us, in some way, knew that something was coming. It turned out to be more significant than my wife was anticipating for me.
Breaking the news to your family and friends
Nobody knew that we were going to these tests. Why get people worried about something that they might not need to be worried about? Nobody at my work knew, none of our friends, certainly none of our family.
It was no warm conversation. This is as cold a cold call as it gets. We [couldn’t do] a synchronous Zoom call where I could talk to everybody at the same time so I thought I’m just going to work my way through time zones.
Nobody at my work knew, none of our friends, certainly none of our family.
My daughter is at law school [in] Vanderbilt, Nashville. I call her up and I hadn’t rehearsed anything in my head. There’s no user manual to talk about this with your loved ones. My daughter, when she gets a call from her old man, that’s something she needs to answer. I yanked her out of a seminar. It’s in the evening, her time. She answered the phone, “What’s wrong?” And that gets me crying before I even start talking. Then she hears me crying and I’m her dad [so] she starts crying.
Nobody in my family had ever heard of multiple myeloma before so telling her was probably the most difficult conversation I’ve ever had with anybody. It was just one person in my family and I still had a ways to go. It gets better with practice, but the first one was extraordinarily heavy.
I wish I’d just hadn’t jumped on the phone. I wish I had thought about it, maybe rehearsed [it] in my head, had some messages that I wanted to clear up. Maybe there’s a way that I could have softly approached it with a text first and warmed into a phone call. I wish I’d rehearsed it. Certainly very emotional, very tough to get by.
It’s like becoming a new parent to a newborn. You don’t get a user’s manual when you become a parent and there’s no user manual on how do I tell my loved ones. It does get easier.
Nobody in my family had ever heard of multiple myeloma before so telling her was probably the most difficult conversation I’ve ever had with anybody.
Difficulty of breaking the news
You don’t want your loved ones to have anxiety. You don’t want them to be worried.
There might be an internal perspective of where it’s the final building block that this is real for me and maybe I hadn’t thought about that. Maybe there’s still a part of you that has not complete acceptance of it because you haven’t told anybody and if you haven’t told anybody, maybe it’s not real. There’s probably a component of that as well and the realization is, “Wow, man, I have cancer and now my family knows about it.”
Any advice I have is [to] rehearse it a little bit. Think about what you want to communicate and how you want to communicate it.
The realization is, “Wow, I have cancer and now my family knows about it.”
Treatment plan
I actually got a binder [with] a bunch of resources in it and what treatment was going to be.
There’s a standard induction treatment for multiple myeloma. Part of my diagnosis involves genetic testing. The type of multiple myeloma is different for everybody.
Mine’s an aggressive form so knowing that and knowing the standard induction treatment that goes into it [leading] up to a stem cell transplant, all that was kind of laid out for me. [The] medications, regimen for a period of three to six months or so, stem cell transplant, then after, some sort of maintenance regimen to continue on.Mine’s an aggressive form so knowing that and knowing the standard treatment that goes into it [leading] up to a stem cell transplant, all that was laid out for me.
Left unsaid in the multiple myeloma world [is] we look at things in three-year periods. Get you through three years and hopefully, there would be more advanced therapies that come out within those three years. Then look at something else for another three-year cycle. While you’re going through proven best practices treatment, the scientists are in the lab looking for new things like CAR T therapies, for example, in the multiple myeloma world. It was laid out to me. A lot of documentation.
In the multiple myeloma world, we look at things in three-year periods.
In a way, I’m pretty blessed. I’m here in the Bay Area. Stanford is right across the water. Across the bay is a world-renowned hematology department and cancer center. My oncologist is associated with Stanford University. A lot of materials ready to help educate me as a patient of the road to come.
First-line treatment
Induction therapy
The highlights were a weekly visit to the infusion center to receive an injection of a drug called Velcade. Not much fluid in that shot and not a very long induction or infusion process.
For multiple myeloma and the Velcade injection, it’s a process that is a slow plunge on the injection so that takes about 10 seconds. I can get in and out of the infusion center in an hour with my vitals checked [and] blood tested.
Built around that was a pill regimen, Dexamethasone, a steroid, and a big dose of it, too. It was a once-a-week dose and that was timed for the same time as my Velcade injection. I would take 40 mg of Dexamethasone and later that day would get my Velcade injection.
If I had a less aggressive form or if I didn’t have 90% of my bone marrow being cancerous, I could get to this MRD (minimum residual disease) level where it was such a minute amount of cancer in my bone marrow where [they can put] you on a maintenance dose, keep you steady.
Side effects of induction therapy
The idea explained to me is [that] sometimes taking a heavy dose of steroids can get you hyped up a little bit. I have difficulty sleeping as a side effect, but one of the side effects of the Velcade injection might be fatigue. When you put those together, there might be something that counteracts and you can go to sleep.
The third and final part of my induction therapy was Revlimid. [It] was a daily pill, 25 mg, which is a heavy dose, much higher than I’d take now in maintenance therapy. That was once a day and I believe that was 28 days on, seven days off in a cycle. I didn’t notice [many] side effects as it relates to Dexamethasone.

Revlimid, particularly at the start, a lot of skin rashes would present [themselves] in my thorax and up my neck and my scalp. I used to get a lot of those.
[With] the Velcade, I didn’t really notice many of the side effects but it’s an injection given in the belly and the injection site would bruise and suffer a big rash as well. You just keep looking for a fresh spot to put the injection.
Digestive problems to Revlimid and Velcade, not exactly sure which one [caused] which, but there’s both constipation and diarrhea. I know some people might be thinking, “How is that possible?” Some cancer patients under treatment can tell you it’s possible. They can both present at the same time.
Then there was fatigue. Thinking back, I don’t know how much of the fatigue is [a] side effect of therapies to also just the side effect of a diagnosis. Just the mental gymnastics that you play in your head so many times, particularly early in a cancer diagnosis, can be exhausting.
Mental gymnastics
From my cancer diagnosis and my initial regimen, which took place for six months, everything I’ve always done has always had some milestone and keynote. Whether it’s athletically, I had an event, or if at work, it was a presentation. If it was as a musician, it was a gig, a performance.
Everything would kind of build towards something and I took that same approach as my cancer diagnosis. I got to exercise. I got to eat. I take my medication because I was building toward fight night to game day performance. It was a realization.
The mental gymnastics that you play in your head so many times, particularly early in a cancer diagnosis, can be exhausting.
Two weeks in, I went to go have dinner with my wife [and] my son. I’m just sitting in a restaurant [and] I was exhausted. I was beat. It took a while to [realize] that when you have a cancer diagnosis, you have a chronic illness. Every night is fight night. Every day is game day. It’s not this training thing that you build up and you hit something. It is every single day. Cancer doesn’t take a day off. You can’t take a day off either. You’ve got to judge your efforts to get that through.
A big part of that for me that can be mental. When I was first diagnosed, I thought about cancer pretty much as soon as I woke up and the last thought that went through my head at night was cancer. A lot of times in between, it was cancer. That’s not the case anymore.
With time comes a different type of acceptance and you do things differently. I think that’s important to tell people early on in their journey. You’re tired; give yourself some credit for being tired. It’s okay to be tired. You’ve got a lot going on.
Just know that every day is fight night and game day performance day. Be able to adjust what you need to adjust to go on for a long marathon because you’re fighting this forever. You’re a warrior and you know you’re coming through the other side. [There are] going to be times you don’t feel great but that’s okay. Don’t beat yourself up on it. Just adjust and get back up. Get back up to speed.

Cancer doesn’t take a day off. You can’t take a day off either. With time comes a different type of acceptance.
Not looking sick
One of the things new to me is people caring about their hair and losing their hair. I have friends that adjust their treatments and do not take certain treatments because they don’t want to lose their hair. For me, what’s the big deal? I did lose my hair through my treatment but when a man loses his hair, it’s not because he’s sick. It could be because of fashion, genetics, or it could be a whole bunch of different things in our North American society. If you’re a woman and you’re bald, pretty much [the] first thing people jump to is, “Oh, is she going through some health problems?”
A mental approach for a lot of patients to come across when you’re going through treatment: Cancer’s not so tough. It’s the treatments that are tough and you’re going through treatment. Sometimes you don’t look so great. You’ll be pale and all these other [varieties] of things. I don’t think people want to look like they’re not feeling well and that’s a big mental thing to overcome. There has to be a certain time and a certain degree of acceptance that you have to give that. That’s the way I am.
You have to find a way to push through it. Don’t let that be all-consuming to you. If you’re not feeling well, it’s really easy to sit on the couch [and] lay in bed for a little while [but] it’s not making you feel any better. It’s making you feel even worse. You’re losing your power and losing your energy. “I just don’t feel like going to the store. I don’t feel like cooking. Maybe I’ll just get some fast food.” Then you’re not eating very well, and that’s certainly not going to make you feel any better. You feel even more tired, then you’re feeling kind of depressed because you’re feeling so tired or eating fast food, and doing this and that. It’s okay for all of us to do that at some point in time.
Cancer’s not so tough. It’s the treatments that are tough and you’re going through treatment.
We’re all humans. Give ourselves a break. Important for everybody — cancer patients, maybe even more so — [to] be able to identify that. Pick yourself up. Today starts the first step. Let’s get out. Let’s get a little exercise. Let’s get a little strength, a little power. [A] different frame of mind. Let’s go forward.
Managing the side effects
I don’t believe going through immunotherapy did anything about diarrhea. For constipation, MiraLAX — odorless, tasteless powder mixed in water. Take that daily. I still take that daily through my ongoing treatment with the rashes.
I did get some prescription drugs and creams to combat the rashes but I didn’t use them much. I was already taking a whole bunch of pills and felt I can live through the rash. As my body adjusted to Revlimid, I felt those needs went away.
For the injection sites, just a regular over-the-counter lotion. For the Revlimid and the rash, even some over-the-counter anti-allergens, like Claritin. I still take Xyzal once a day just to help combat potential skin problems.
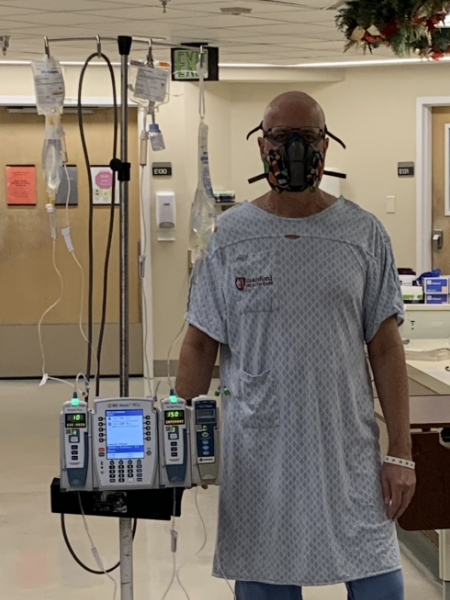
Stem cell transplant
Losing my hair
I knew that if I was going to get a stem cell transplant, I was going to go through chemotherapy, and going through chemotherapy, almost for sure I was going to lose my hair.
In induction therapy, I thought, “If I’m going to lose my hair, I’m not going to shave and I’m not going to cut my hair, and then I’ll do it my way just before I go through therapy. We’ll have a big party and we’ll shave my head and we’ll cut off my beard.” I started getting this mountain man look as I was going through my induction therapy because I wasn’t cutting my hair and I wasn’t shaving and I was just preparing for the time when I was going to shave it down before chemotherapy took it for me.

When I started my induction therapy, they were telling me, “Three to six months, you’ll take maybe a stem cell transplant… We’ll see how you progress.” And me wanting to be an overachiever, “Let’s do it sooner!”
I went to go see a specialist just a couple of months into it. She gave me some great advice. “What are you in a hurry for? You’re responding well to your induction therapy. Let’s keep going at it for a little bit. There’s no need to rush.” Coming from my perspective, if it’s three to six months wouldn’t three months be better? Not necessarily.
I wasn’t learning anything about stem cells and stem cell therapies because I was focused on induction therapy and what could I do. What could I do to help present a garden of my body to help grow healthy cells as opposed to cancer? I was concentrating on clean eating, drinking, and exercise, in my mind at least helping the medicines do what they’re intended to do. It was maybe May when I got this whole idea [that] maybe [I] don’t need to rush into a stem cell transplant.
I continue to make progress, but that second bone marrow biopsy probably would have been in early September. It’s gone from 90% to 10% but the markers are there. Not at an MRD level through induction therapy. Now’s the time to probably think about a stem cell transplant.
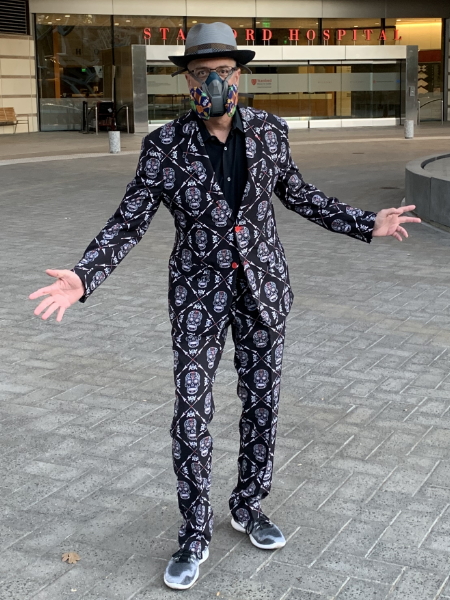
Stem cell transplant, you start it off with chemotherapy. It’s not day one, it’s day two, and that chemotherapy is going to be chemotherapy that probably results in losing your hair. I had a party that was a fundraiser for the Multiple Myeloma Research Foundation. It’s $20 a swipe with the clippers. We raised $250 that night that we matched. I was going to go bald sooner or later anyway so I went bald my way.

Preparing for chemotherapy
The first day is surgery for catheter placement. Chemotherapy can be extraordinarily harsh going through your veins so I had a catheter placement. I was also going through daily blood tests. It’s a Hickman catheter put in my chest; [a] very quick procedure. It’s conscious sedation, in and out. The second day, [I had] my first chemotherapy dose.
I [went through] 3 different types of chemo during my process. I think [Melphalan] was my last dose, either [the] second or third dose. BCNU (Carmustine) would be another one. The first one I think… Cytoxan. [A] nice big heavy dose of Cytoxan.
Side effects of chemotherapy
I do want to share about Cytoxan and chemotherapy-induced nausea. I thought I knew what nausea was and I thought I was going to be okay with it. I learned through my very first chemo that’s not the case.
We had to be in very close proximity to the cancer center. We relocated to Menlo Park, California, to be close to it. That first stop by, you need to be within an hour of the cancer center in the Bay Area. That means that could be three miles away. We were staying in a hotel and I knew I was going to be there for five meals. My wife and I go to the store. Easy, right?
[On] day number two, [the] day after my surgery for the catheter, I spent all day with Cytoxan. It gets synthesized through your body, through urine, and through your bladder so it’s a lot of fluids [getting] pumped into you. You need to drink a lot. It was all day sitting in the infusion center and getting it.
I had lunch feeling pretty good. I watched Thursday night football that night; feeling pretty good. It’s about 11:30 at night [and as] my wife [is] getting in bed to go to sleep, I’m like, “Lori, I need you to go to the store to get something.” [The] stuff that we had picked out [earlier at the store], just the thought of it, was making me nauseous.
I was on all these anti-nausea medications but this was sweeping over me. All I could think of was maybe some crackers, ginger ale, or something like that.
You got to stay on top of your meds. That’s just a given. If they say take this every 4 hours, take it every 3 hours, 59 minutes, and 59 seconds. Don’t miss it at all. Stack them. Keep it up.
Always keep a little something in your stomach and have a lot of choices because whatever gets presented right in front of you is something that you’re not going to like. That was a recurring theme for the next six weeks. My wife would ask me, “Hey, Ray, do you want…?” Just her saying words were like making me sick to my stomach. I’m like, “I know you’re doing this out of love and asking me if I want something. Let me come up with the words because just even the words can make you nauseous.”
I thought I knew what nausea was. I didn’t know what nasty was. I do now and it can be crippling. It can be debilitating. Through chemotherapy, that first time around, I did not have episodes of vomiting. The second [and] third time around, I did for a couple of days. No one likes doing that. It’s probably not nausea that you’ve experienced previously in your life before you go through chemo.

[There are] times when you double up [the anti-nausea medication] and definitely do that. For me, there’s a very, very fine line between hunger and nausea. Don’t think about your favorite food. What’s kind of common advice is don’t even think about eating your favorite food going through treatment because it’s not going to be your favorite food ever again. Save that and do something else but have some choices for you. Wet and cold were best for me, way over something dry.
One of my chemotherapies created mouth sores and going in ahead of that was cryotherapy, chewing on ice for 15 [to] 30 minutes. I did have one in the back of my throat. You have to take some pretty big pills and pills can start me getting gagging. The last thing you want to start doing is [to] start gagging when you’re nauseous. You’re sitting down there and fighting the urge to vomit. You’re just trying to get yourself together, to muscle down a horse pill that you’re trying to get down.
Another handy thing: [a] pill crusher or something to cut pills. [There are] some pretty big ones for the possible infections that you might get, antibiotics [and] antivirals that you need to take. Cutting those in half, maybe even crushing them, [putting] on a little bit of ice cream, and working it down.
Beware of things that can kick-start your nausea. You’ve been doing everything right but the next thing you know, you start gagging on a big pill because of a sore in your mouth, and then it gets you right back to step one again.
Give yourself a whole bunch of options. For example, when it comes to food, if you need five meals, have 20 ready. Also, redefine what you think a meal might be. It’s not going to be 2,500 calories of a whole bunch of stuff, a big platter of food. Just a bite or two, here or there. It gives you sustenance, gives you strength, gives you power, and something that you can stomach.
Recovering from stem cell transplant
The transplant was the long haul. The stem cell transplant [is] where they’re using your own stem cells to reintroduce [into] your body. All in all, it’s six [to] seven weeks. It starts with the catheter placement, a massive dose of Cytoxan, and then you’re free to go in 24 hours. It kills myeloma cells that also kick-starts your immune system. Be prepared for wackiness.
When your nurse is giving you chemotherapy, they go to extraordinary pains and measures to make sure none of that touches the outside of their body or their clothes. They are in complete hazmat [suit] and they’re injecting it straight into your heart to the catheter. That is a weird thing to kind of get over.
Cytoxan kick-starts your body’s immune system [and] starts ramping up the production of stem cells. Then you go through, for me, about 11 days of Neupogen injections that my wife would give me three shots a day to spur all these stem cells to get coaxed out of the bone marrow [and] into [the] bloodstream. Once they enter the bloodstream, that’s a lot easier to get taken out of as opposed to 200 bone marrow biopsies to get your stem cells out. For me, that was about 11 days of that until I finally got a blood count that was high enough to go through apheresis.

Apheresis is a dialysis type of treatment where [the] blood comes out, gets centrifuged around by volume, the stem cells are kept, [and] the rest of it gets put back into you. [Sessions] can take over three days. For me, I did it one day, about 4 hours. Once you start, you can’t stop. That was the end of the first step and that was great because after that, you get a couple of weeks where you kind of rest up and get your body ready. All said and done, it was like one big chemo day.
Side effects of stem cell transplant
I didn’t feel great that night and the very next day, but after 24 hours, I was feeling better. The shots were a mental thing to get over and then I had a two-week break. Then the rubber meets the road.
The harder part is the second half. That’s two massive doses of chemotherapy in a three-day period. It’s not a very long infusion. It’s maybe 15 [to] 30 minutes afterward. Those two big massive doses of chemotherapy [are] designed to completely wipe out your bone marrow.
You start to feel those effects because your bone marrow is what makes your blood cells and red blood cells, for example, carry oxygen. You will not have any more red blood cells except [for] what’s in your body. Over time and quickly, those kinds of break up and dissolve. They’re going around, they’re getting banged up through their journey through the vascular system. They disintegrate. Your blood cell count starts going down and you have nothing in your bone marrow to get that back. They give you your stem cells back a couple of days later, after that second dose of chemotherapy. Then it’s a waiting game until it engrafts.
Waiting for stem cell engraftment
Those are long 11 days. During that time, I had nausea after those chemotherapy treatments. Getting the stem cells back as they package it up and DMSO. Everyone’s going to have a weird side effect and that’s going to be body odor. It depends on your body on what type of body odor you get. Mine was tomato soup. Your stem cells come back in and the next thing you know, the room smells like tomato soup.
After my stem cells have been introduced, my blood counts just kind of went to zero. I needed a couple of red blood cell transfusions. I started popping a bit of a fever. I have low blood pressure, to begin with, but with a fever and low blood pressure, that could be anything.
All these prophylactic doses of very strong antibiotics got to the point where I needed to be hospitalized. Moved out of the hotel in Menlo Park and into Stanford Hospital for four nights. I probably could have left after two [because] my fever was gone but they wanted to wait [to] see some platelets and [to] know that it’s engrafted. Then it was home for the recovery. Those 11 days until I engrafted… very long days, very tiring. It’s a tough road.
Living with myeloma
Maintenance therapy
My second birthday, the day that my stem cells were given back to me, was November 5th. I know I engrafted around November 16th or so. I’d probably started maintenance meds in February again and I was kind of bummed out because my maintenance regimen was Revlimid and Velcade. I just went through a little garden walk through hell just a couple of months ago, and I’m back to the same thing, minus the Dexamethasone? My specialist [said], “You did the right thing. You beat the thing down. That’s the whole idea. Beat your myeloma down to the lowest possible level that you can and then do the maintenance therapy.”
My Velcade is now half of what it used to be so instead of weekly injections, it’s biweekly injections. My Revlimid dosage is now 10 mg. Currently, I’m at three weeks on [and] two weeks off. It’s been a juggle now trying to figure out what’s right. It’s been over a year. It was 28 days, seven off and it’s ranged from that to now three weeks on, two weeks off, trying to figure it out.
I still suffer from a low white blood cell count. I’ve only had to miss one treatment though; once, my neutrophils were too low to do [the] treatment so we passed on the Velcade injection. We’re into the new normal for me. I think I’ll always have a low white blood cell count but trying to get the right meds for the new normal.
Adjusting to the new normal
It’s a bit of a leash. At this point, I’m chained to an oncology center. I have to be there every two weeks. I’m trying to come to terms with that because my kids are out of the house now and I want to know: where do we want to live? Change is always difficult. Change when it comes to your healthcare and [the] professionals that you deal with, that’s a huge complication. If I move out of the area, then I no longer have my doctors, my specialists, and things like that. Mentally, it’s this idea that I’m tied to.
I need an infusion every two months or every two weeks. Can I go to northern Italy for a month and hang out? I can, but I’ll be missing a treatment and so is that the best thing to do? I quickly overcame my disappointment. You get kind of used to it. It’s a way of life and that’s what you do.

I got my strength back pretty quickly. Rebounded physically pretty well. A friend of mine, as a New Year’s resolution, was going to walk 1,000 miles. I thought that’s something I could get behind. I could do that because I’d already been walking a little bit. So I did!
Physical exercise is important. It’s always been important to me but I think it’s important here. It makes me feel better and when I feel better, it also helps me.
As a cancer patient, take advantage of the days that you’re feeling good. Go out there and do something. It’s human nature for us to sit around. But keep in mind, it’s very tough when you’re perfectly healthy to break your New Year’s resolutions. You’re not injured. You just don’t feel like it. Being a cancer patient, you don’t want to work out. You just don’t feel like it. But you need to prepare your body for your medications. You need to have that type of power and strength and energy to be able to shop for yourself, prepare healthy meals, go to the doctor, [and] take your medicines. It’s overcoming that mental aspect of it.
I like to view myself [as] a system of subcomponents. There’s a physical component and mental component, emotional and spiritual, and they all are interrelated and all play amongst themselves. I need to be alert on when one of those might be down [and] help push that back up. Do something else. Maybe a change in the frame of mind to get me to take care of myself as a whole person.
Complementary therapies
Going through my induction therapies, I was aware of a local organization. My doctor said, “Try these things out and get grants for these complementary therapies.” This organization [offers] acupuncture, acupressure, visual imaging, [and] a couple of other modalities.
The idea is [to] try some of these complementary therapies. They’re not going to cure your cancer, but maybe they can help you feel better. For me, it was trying acupuncture and also acupressure for skin and fatigue
One I did not mention earlier [was] insomnia. I can tell you that [with] acupuncture, I used to fall asleep during the treatments so that must have helped a little bit with insomnia. It was good to try those out. It’s something I would not have tried on my own, something that insurance doesn’t cover.
[In] this particular organization, I got a grant to try these things out. They want you to try these different modalities and see what might work for you. If acupressure doesn’t work for you, maybe you might find that acupuncture does. Then if it does, what’s it hurt to give it a little bit of a go and see if it helps alleviate some of these symptoms? Sometimes it’s the treatments that are more problematic in the way that you feel than cancer itself.
Getting help is important. These are people right next to me, arm in arm with me, and that strength in numbers means everything to me.
Getting support from family and friends
When I first was diagnosed, [people asked] “How can I help you?” I kept on saying, “I’m feeling good. I don’t think I need any help.”
[It] took somebody at a group to share with me that people want to help you but it’s not just to help you. It’s also to help themselves. They care for you and they love you. They feel better if they know they can do something for you so consider that. I don’t need someone to drive me to my doctor’s appointment. But if [a friend needs] to drive me to my doctor’s appointment, then [I’ll have them] drive me.
Accepting help initially was kind of difficult. I needed somebody from my support group to set me straight on it. It is about you, but it’s also about them. Getting help is important.
My wife went through this entire process with me. If you know anybody out there going through any type of significant health issue, reach out to them and help. It is daunting. She continues to be my rock. There is just so much that goes on with a serious health issue and our complicated health care system. There’s a ton of correspondence. You need somebody next to you. I can’t imagine going through it alone.

What’s meaningful to me is this great network of folks that my wife and I have and these friends. It means the world to me that it’s not people standing behind me as I go into this fight. These are people right next to me, arm in arm with me, and that strength in numbers means everything to me.
I’m so grateful for the people that have [been] there for me. They care about me. I don’t feel like they’re behind me. I feel as though they’re next to me and there’s a difference. I’m thankful for that. Everyone needs that.
I feel as though it’s my role, my responsibility to the patient community and the caregiver community. When I was first diagnosed, they were asking me, “What can I do for you?” My answer was nothing. It finally got to the point where I was speaking in front of so many groups sharing my story that I came up with a list. [There are] four precise things that you can do.
Go to your doctor
I would have been in a much worse situation if I hadn’t gone to my doctor and I went to [the] doctor for a specific thing. It was not general maintenance. [It had] been about a year and a half since [I’d] had a blood test. Go to your doctor [and] get a blood test. Do it for yourself.
Mitigate your risks
We all have toos in our life. I call them the toos — T-O-O — and you don’t need a doctor. You don’t need me to tell you what those toos are, but mitigate your risks. They’re all associated with toos: drink too much, smoke too much, eat too little vegetables, eat too much red meat… We all know what those are. Mitigate your risks.
Reach out
If you know somebody who’s going through a health issue — particularly if they’re going through it alone — reach out to them. I can’t imagine going through this without my primary caregiver, Lori, but just my support community.
I’ve been there and ashamedly, I didn’t reach out to people in the past because I didn’t know what to say. Start with what you do know and that is you don’t know what to say. Start that conversation off with, “I don’t know what to say, but I love you and I care for you. And I’m hoping that we can get through this difficult conversation because I want to be here and support you.” Reach out to those people.
As a cancer patient, I never feel [stronger] than I do when I’m around my people and I know they’re with me.
Contribute
Find something that you’re passionate about and give your time, give your money, give both. Health is difficult.
I was unaware before I started my cancer journey that 33% of the people in the United States, one out of three, are going to be diagnosed with cancer sometime in their lifetime. If you read another study, you’ll see four out of ten will be diagnosed. It affects either you or affects somebody very close to you, in your professional [or] personal network. But even if it’s not cancer, it’s some other health issue. Find it. Find out what you’re passionate [about] and look for ways to contribute. We’re all in this together. As a cancer patient, I never feel [stronger] than I do when I’m around my people and I know they’re with me.
Reading through different books upon diagnosis, you hear some of these anecdotes from people. “The best day of my life was the day I was diagnosed.” I’m not quite there yet. I’m not quite ready to say that. But cancer hasn’t taken away my life and parts of my life. It’s enriched my life.
It’s my job to help the person behind me, reach back and pull them up to me, and show them how to live, too. Cancer is giving me that.
New role as a cancer patient
Prior to my diagnosis, I had a lot of different roles in my life: father, husband, son, brother, worker, boss, teammate, bandmate, and all these roles. With each one of these roles came purpose. Cancer didn’t take any of those roles away. It just added more. It enriched my life. Now, I am a patient and I am part of a larger patient community that is all inspiring. People who have been there and done that, and are showing others the way; that is just inspiring and it’s motivating.

Being a member of this patient community, I can go to the Multiple Myeloma Research Foundation’s Walk in San Francisco. I went three weeks after I was diagnosed and I’m looking at my heroes — these healthy, vibrant cancer patients wearing a different colored shirt than everybody else, participating in this thing. They’re showing me how to live with myeloma. It’s my job to help the person behind me, reach back and pull them up to me, and show them how to live, too. Cancer is giving me that.
Cancer is giving me a role as a patient advocate, as an advocate for the caregiver community, going through stem cell transplant. It’s tough. It’s very easy for me to get caught up in my journey but I know what I can do. I know what I can take and what I can handle. Even [during] the tough days of stem cell transplant, your loved ones, the patient community, the caregivers, they don’t know. There’s a lot that they carry with them. Those men and women are so brave.
Everybody’s different. If you are thinking that cancer is taking things away from you, also look at it the other way around. One go so far it’s called a gift. That does add things to your life. Those things can be very enriching and very rewarding. Don’t lose sight of that.
I love talking to new patients about multiple myeloma and what I’ve done and what they might be able to [do]. I started a blog, MeMyselfAndMyMultipleMyeloma.com, that I infrequently update and chronicled a little bit of my journey. Some people view cancer as a journey. I don’t view it as a fight. It’s a little bit different. We all have our own things. When they’re diagnosed, there’s a lot left to live for, a lot left to do, [and] a lot of purpose. Anything I can do to help any individual out, I hope I’m aware of it because I want to jump at the opportunity.


Inspired by Ray's story?
Share your story, too!
Multiple Myeloma Stories
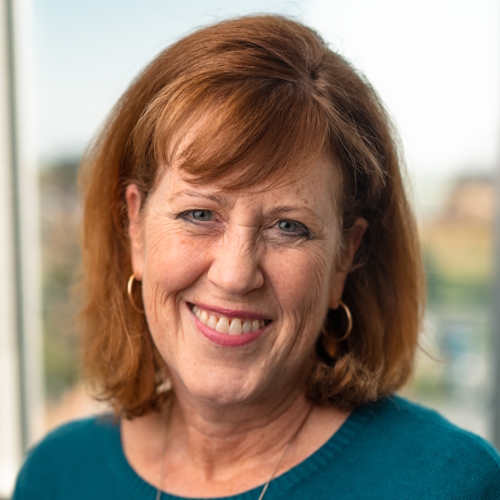
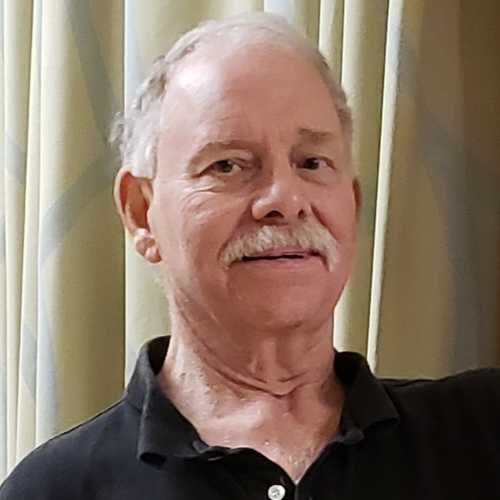
Clay D.
Diagnosis: Multiple myeloma
1st Symptoms: Persistent kidney issues, nausea
Treatment: chemo, radiation, stem cell transplant
...
Melissa V.
Diagnosis: Multiple myeloma, stage 3
1st Symptoms: Frequent infections
Treatment: IVF treatment & Chemotherapy (RVD) for 7 rounds
...
Elise D.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: Lower back pain, fractured sacrum
Treatment: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P.
Diagnosis: Multiple myeloma, stage 3
1st Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatment: Chemotherapy (Bortezomib/Velcade), Daratumumab/ Darzalex, Lenalidomide, Revlimid) and stem cell transplant
...
Ray H.
1st signs: Hemorrhoids, low red blood cell count
Treatment: Immunotherapy, Chemotherapy, Stem Cell Transplant
...
Valarie T.
Symptoms: Nose bleeds, fatigue, back pain
Treatment: Chemotherapy, stem cell transplant
...
Julie C.
Symptoms: Queasiness, food aversions, lack of appetite, fatigue
Treatment: Stem cell transplant, chemotherapy (D+PD), bispecific antibodies (talquetamab & cevostamab)
...
Laura E.
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
...