Beth’s Relapsed Refractory Multiple Myeloma Story

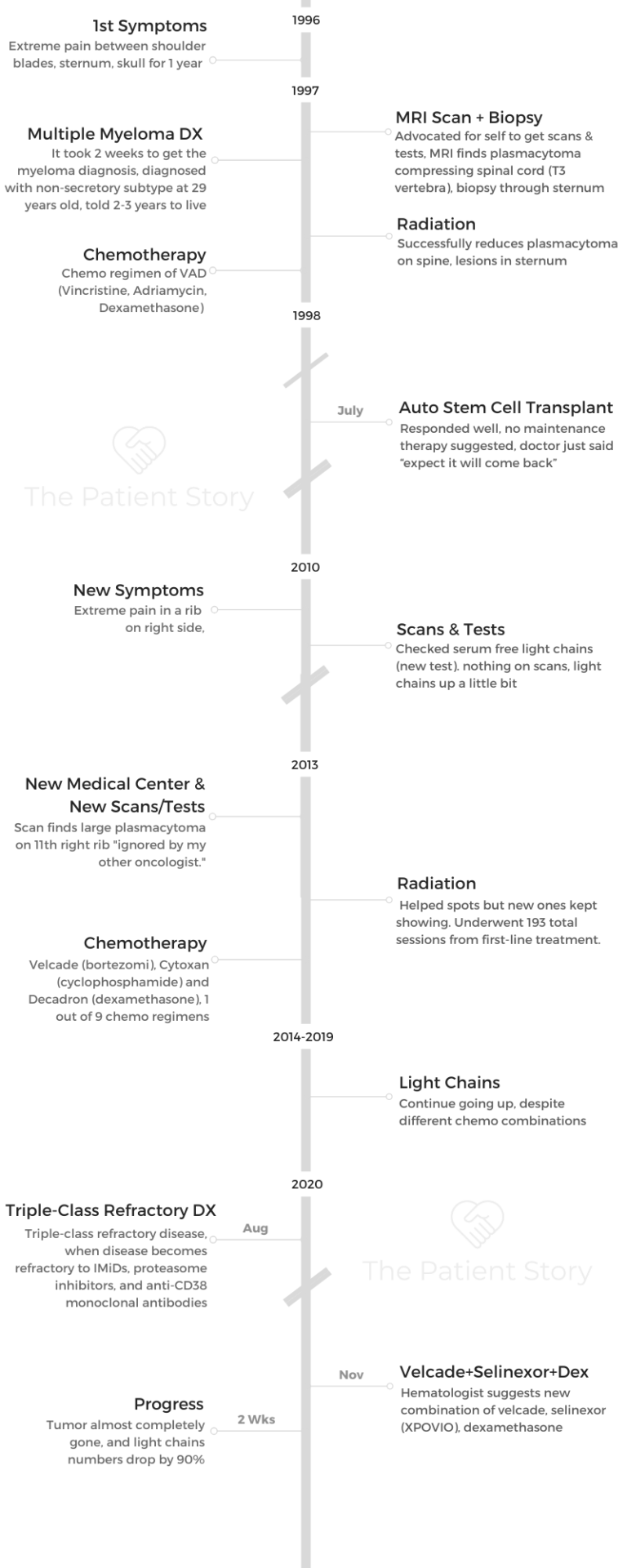
Beth was just 29 years old and the mother of 2 young kids when she was diagnosed with multiple myeloma. She describes how she got through first-line treatment of radiation, chemotherapy and a successful stem cell transplant.
For 12 years, Beth lived her life with no sign of myeloma. When her pain returned, she didn’t think much of it after a doctor concluded it was unrelated to the myeloma. But just a couple years later, an oncologist said the myeloma was back — the cancer had relapsed.
Beth dives into her over-2-decades-long myeloma experience, including how the myeloma became triple-refractory (it didn’t respond anymore to the usual drugs), the new drugs that worked and didn’t work, and how she has managed to live her fullest life with the disease.
Explore her incredible 5-part story series below. Thank you so much for sharing, Beth!
- Name: Beth Ayen
- Diagnosis (DX)
- Multiple myeloma
- Relapsed/refractory multiple myeloma
- 1st Diagnosis:
- Age: 29 years old
- Symptoms: Extreme pain between shoulder blades, sternum, head for 1 year
- Burning sensation that radiated out
- Tests for DX:
- MRI found a plasmacytoma compressing spinal cord
- Treatment
- Radiation therapy
- Chemotherapy
- VAD (Vincristine, Adriamycin, dexamethasone)
- Autologous stem cell transplant (SCT)
- Relapse:
- Age: 45 years old
- Symptoms:
- Extreme pain in ribs and head
- Light chain #s up
- Treatment:
- Radiation (193 sessions total over 7 years)
- Chemotherapy (9 regimens since beginning), mainly:
- Velcade (bortezomib), Cytoxan (cyclophosphamide) and Decadron (dexamethasone)
- Different drug combinations
- Elotuzumab (Empliciti)
- Belantamab mafodotin (Blenrep)
- Selinexor (Xpovio)+ bortezomib (Velcade) + dexamethasone
- VIDEO: Early Symptoms of Multiple Myeloma
- 1st Symptoms of Multiple Myeloma
- The Multiple Myeloma Diagnosis
- Processing the Diagnosis
- Getting your prognosis
- Dealing with the possibility of a “terminal” diagnosis
- How did you break the news of the myeloma diagnosis?
- What support was most helpful from other people during this time?
- How did you handle the cancer diagnosis with young children?
- A silver lining to the shifting household roles
- "Let people help you"
- VIDEO: Finding Treatment in a Small Town
- VIDEO: Multiple Myeloma Relapse
- VIDEO: Relapsed Refractory Multiple Myeloma Treatment
- CAR T-Cell Therapy
- Belantamab mafodotin (Blenrep)
- Selinexor (Xpovio) + Bortezomib (Velcade)+ Dexamethasone Combination (SVd)
- How did you learn of this treatment option?
- What was the status of your myeloma?
- Describe the selinexor + Velcade + dexamethasone (SVd) regimen
- Describe the selinexor, bortezomib and dexamethasone combination side effects
- What has helped you manage the side effects?
- What’s the real impact of finding a new treatment that finally works for you?
- VIDEO: Living Life with Multiple Myeloma
- Multiple Myeloma Stories
Thank you to Karyopharm for its support of our educational program. The Patient Story has full editorial control of our content. The interview has been edited only for clarity.
This is not medical advice. Please consult with your healthcare provider for treatment decisions.
VIDEO: Early Symptoms of Multiple Myeloma

1st Symptoms of Multiple Myeloma
Introduction: Tell us about yourself
I live in Casper, Wyoming, and my husband is an engineer. He works for the highway department. I have 2 children. My daughter, Becca, lives in Colorado Springs, and she has 2 kids. I have 2 grandkids, and their names are Isaac and Piper.
They’re really fun, and I’m really excited that I got to see grandchildren in my life. It’s so exciting. I have a son and daughter-in-law, who live in Houghton, Michigan. They are pregnant. They’re going to have a baby in September, so that’s really exciting!
They’re far away. Hopefully, we’ll get to know our little baby pretty well. I’m a retired third-grade teacher. I worked as a teacher for about 8 years.
Then just with health issues and the myeloma, I’ve just decided that I needed to retire and take some time off and focus on my health.
Other than that, we love to travel Wyoming and visit all the incredible places that there are here. I love to crochet, and I love to read. I’ve been having trouble with my vision. When I can, I love to read. We love to go see movies and those kinds of things, so that’s what we do.

What finally got you to go to the doctor’s office?
It was just becoming so consistent. It had started between my shoulder blades, and then the same kind of pain was happening in my sternum and in my skull.
It was like a burning pain. It started out as a pinpoint, and then it would radiate farther out, farther out, and then into the other bones. I just thought, “This is not right. This is not muscular pain.”
I saw several doctors in my little town that we were living in, Rock Springs, Wyoming. They would just say, “Oh, everybody has pain. Just do these exercises. Everybody has back pain.”
I finally just was talking to a lot of people and just sharing with them how I was in all this pain and someone said, “There’s an orthopedic surgeon in Salt Lake City who will see people without a referral.”
We decided to go ahead and go see him. He was able to do an MRI on my spine without a referral. That was really great. He was the one who found the issues that were happening in there.

How did you advocate for yourself as a patient?
I think part of it is you really have to remember that you know your body when other doctors are telling you these things, and you just know that it’s just not right.
My first bachelor’s degree is in exercise and sports science. I just knew that these exercises that they were giving me were not the right things to do. They were causing more pain.
I just thought this is not right. I’ve got to go somewhere where someone will actually take me seriously. Really, I’m one that never goes to the doctor for pain.
My doctors now are like, “You need to tell us when you are in pain.” I’m always way far along in the process because I wait so long. I knew that because of that personality trait, that there was something serious and that I was really feeling like I needed to see a doctor who could help me.
We just pushed and pushed and pushed and researched and looked and asked people.
I think that was an important thing for us to do, because I don’t know how long I would’ve gone. I would’ve had a lot more issues, I think, if we hadn’t gone then.
»MORE: How to be a self-advocate as a patient
When did you first think of cancer?
Beth went to a Salt Lake City doctor, who finally gave an MRI and found a plasmacytoma that was compressing her spinal cord where her T3 vertebra used to be.
What the doctor told me was, “We’re going to do a biopsy.” They decided to do a biopsy through my sternum because they didn’t want to do it through my spine. It was too dangerous. They did a biopsy through my sternum. This was the week before Thanksgiving in 1997. He told me, “Just wait. We’ll call you with the results of the biopsy.”

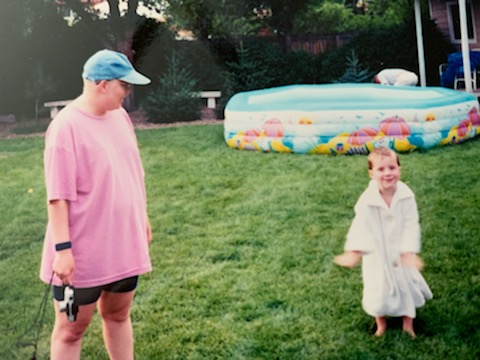
Of course, when you hear the word ‘biopsy,’ you think ‘cancer’ for sure. That was really difficult. I had 2 kids. I had a 5-year-old and a 3-year-old at the time, which made it really, really hard to think about the cancer diagnosis.
We lived 3 hours away from Salt Lake City. That’s how far Rock Springs is from Salt Lake. It just all made it very difficult. I went home, and I sat by the phone. I was cleaning my house. I was getting ready for Thanksgiving.
The Multiple Myeloma Diagnosis
Getting “The Call”
I was doing all the things that you do for that and just working and feeling pretty normal, except for the pain in those places. I got a call on Wednesday, the day before Thanksgiving, and it was the orthopedic surgeon.
He said, “I’m going to hang up this phone in about 2 minutes, and the phone’s going to ring. It’s going to be an oncologist, and she’s going to tell you what she needs you to do.”
I put the phone down. Literally, when I put the phone down, it rang. This was back when we had phones that hung up. Anyway, I picked up the phone, and it was this oncologist. She said, “Beth, you need to get to Salt Lake right now.”
I said, ‘Do you realize it’s 3 hours away? I have 2 small children that I need to figure out what to do with.’
She said, “I don’t care. You need to get here immediately. They’re going to hold the admissions office open for you because they’re waiting for you.”
I was like, “Okay, well, we’ll get there as soon as we can.”
We threw stuff in a suitcase. We dropped our kids off. We had lived in Evanston, Wyoming, for a while, so that’s on the way to Salt Lake. We dropped our kids off there with some friends, and then we drove the longest drive that we ever drove from Salt Lake City. It’s about an 80-mile drive. We just sat there and just did not talk.
We knew that now we’re seeing an oncologist. We knew this was cancer now, but we had no idea what this meant.

We showed up at the hospital. Of course, as soon as I walked into the admissions office, they’re like, “Are you Mrs. Ayen? Are you Mrs. Ayen?”
“Yes, I’m Mrs. Ayen.”
“Okay, we’re going to take you up to the oncology floor.” They took us up there. The nurse at the desk said, “Your room isn’t quite ready, so can you just sit in the waiting room for a minute?”
I said, “Sure.”
Then this doctor walked in a few minutes later, and she said to the nurse, “Well, where’s Mrs. Ayen?”
The nurse said, “Well, she’s right there.”
The doctor said, “No, that can’t be her.”
The nurse was like, “What do you mean?”
She’s like, “Because she shouldn’t be able to walk. She shouldn’t be moving.” She came over to me and she goes, “Can you walk?”
I said, “Oh yes, I’ve been cleaning my house. I’ve been making beds. I’ve been cooking turkeys.”
I said, “Yes, I’m doing fine,” and she said, “Oh, my goodness. Please don’t move an inch. We’re going to take you to your room. I want you to lay in bed, and you’re only allowed to get up to use the restroom.”
At that point, another oncologist came in and they told me that they suspected that I had multiple myeloma. They saw myeloma cells in my biopsy, and I had a plasmacytoma where my T3 vertebra used to be. It had eaten completely away, and it had completely compressed my spinal cord.
They were worried that any movement could cause complete paralysis. They wanted to do 10 days of radiation to get that tumor down so that my spinal cord would come back, and I wouldn’t be in such danger of severing that spinal cord with that plasmacytoma.

It took longer to diagnosis because I didn’t fit the “myeloma profile”
They were just really surprised, and they couldn’t believe it could be multiple myeloma, so it took a while for them to diagnose it because
I was only 29, I was a White female, and this is just very not typical of myeloma, especially in 1997.
They weren’t seeing that very often, and they actually had never seen it — at this hospital and several hospitals that I had been at — that young.
They took a while to diagnose it to make sure that they were correct, but they took it to the tumor board at University of Utah. The other thing about it was I didn’t show the M protein, which is very indicative then of myeloma, and so I didn’t show that. I was considered non-secretory, so that is a more rare side of the multiple myeloma, and it was more difficult to diagnose because of that.
How long were you in the hospital?
I was in the hospital for about 10 days. Actually, it was only about a week, and they did radiation every single day, trying to get that tumor down until it was safe for me to move around.
My parents live in Denver and were coming up to visit us for Thanksgiving, and so they just bypassed Rock Springs, picked up our kids in Evanston, and then came to us in Salt Lake City.
They stayed in a hotel for a little while while I stayed in the hospital, and then I had to stay in the hotel. My husband and I ended up staying in the hotel with them for a few days after because they let me go from the hospital, but I was still doing radiation for a few days. I had other appointments that they wanted to look at. They wanted to see what the ramifications of the tumor were going to be on my spine.
Processing the Diagnosis
Getting your prognosis
There’s just a quick story about the neurologist that I saw. He said, “Oh, there’s some things that we could do, but you’re not going to survive long enough to make it worth it.”
I know. It’s just crazy. I was like, “Oh, okay, well, I guess.”
The oncologist gave us a prognosis of 2 to 3 years at the time, and then this neurologist told us that. At that point, we were just feeling like, “This is a short-term thing, or I’m going to die from this. We got to figure out what to do with our life, with our kids. How’s Mark going to raise these kids by himself?”

Dealing with the possibility of a “terminal” diagnosis
It was really difficult, and it was difficult for me to have the kids there in some ways while we were in the hospital. I loved having them there for sure.
I felt like we were all together as part of a family, but I also was dealing with so many emotions that I didn’t want to burden them with my dealing with that I have cancer and it’s terminal. I’m probably not going to live very long with it.
That was really difficult. I think my daughter still struggles with some of that because she was five. She remembers some of it. My son doesn’t have any recollection of any of that happening, but I can remember them coming in, sitting on my bed, playing with the up and down buttons on the bed, different things like that, but there were some difficult parts of that.
I was glad to have them there because a mom wants their kids by her side. At the same time, it was hard on them, and I wish they didn’t have to go through it.
How did you break the news of the myeloma diagnosis?
I remember sitting in the hospital and Mark, my husband, calling a lot of people and telling them what was going on. We’re churchgoers, and we have a lot of close church family. In Evanston and in Rock Springs, we had that.
»MORE: Breaking the news of a diagnosis to loved ones
What support was most helpful from other people during this time?
There were a lot of people who wanted to support us. They came and visited. When we got home, they brought meals and cleaned our house. They did so many things for us, which was just amazing.
They took care of our kids. They would take them on trips. If they were going to the store, they’d come and pick them up. If they were going to McDonald’s, they’d come and get them or whatever. That was really helpful.

How did you handle the cancer diagnosis with young children?
I think the way that we just dealt with the kids was just that, “Mommy is sick, and she’s going to have to do some medication.” They were too young to really understand.
We use the word “cancer,” but they didn’t understand what that meant and the ramifications of that until later on in their life. They just basically have lived with it their whole lives pretty much.
I can remember when I lost my hair the first time, my daughter did not want to see me with a bald head. I always wore a hat or a scarf or something. I didn’t wear wigs too much.
I just didn’t have access to good wigs at that time, with where we lived and the cost of them. They have such better resources now.
Anyway, my son loved it. He would take my hat off. He would rub my head. He just thought it was so cool that I was bald. That was a difficult thing to manage because I didn’t want to upset my daughter.
At the same time, I couldn’t stop my 3-year-old from that. We just lived that life. I was homeschooling my daughter in kindergarten at the time, which is crazy.
I was doing the first line of treatment, the VAD, which was vincristine, Adriamycin, and dexamethasone. They would hook me up in Salt Lake with a pump with this fluorescent pink medication in it that had “biohazard” written all over it, and I’m thinking they’re pumping this right into my veins.
They would hook me up in Salt Lake. I would go home for 4 days, and then a home healthcare nurse would come into the house and take care of it.
My kids were around this all the time, and I had very difficult veins. The poor nurses would just struggle and struggle. My kids would be walking around while they’re doing all of this.
Sometimes, I think maybe I would try to expose them less to less of that if I had to do it over again, but I didn’t know what I was doing. This was all new to us. I was just trying to survive the day and do what they told me to do.
It was a difficult treatment. It was very hard on the body, and it was really the only treatment at that time — that was widespread, anyway. Luckily, my husband worked really close to the house and had a very flexible job. If he needed to come home while I was feeling sick or whatever, he was able to do that and take care of the kids.
A silver lining to the shifting household roles
One thing, I guess, is that it developed a really close relationship between their dad and them because he was their caregiver in a lot of situations where, normally, I would have been.
My mom would come for about a week during that time when I was doing the VAD treatment. Then the next time, the next month, my mother-in-law would come, and they would just switch back and forth and help with the kids.

“Let people help you”
I think the thing that I would tell other people is to accept help. Let people help you, and ask for help if you need to. I know it’s so hard. I want to do everything on my own and just do it.
Sometimes if you need help, it’s okay to ask.
VIDEO: Finding Treatment in a Small Town
Rural Cancer Care Experience
Beth underwent radiation therapy to decrease the lesions and the plasmacytoma on her spine. She then had the chemo, the VAD, which did not reduce the lesions. The following year, Beth went through an autologous stem cell transplant and responded well.
How did you manage getting treatment in such a rural area?
Because we lived in such a small town of Wyoming — and really in Wyoming, they don’t do stem cell transplants anywhere — we had to go to Denver, which is where my parents lived. That worked out really well.
They wanted us to go to Salt Lake City because that’s where my original oncologist was, but it worked out better in Denver because my parents were there. They could watch the kids.
The need for more support
We knew it was going to be most of the summer of 1998. My husband had just gotten a job. We had just moved recently from Evanston to Rock Springs. He was new to his position.
They made it so nice for him. They donated sick leave. All over the state, they donated sick leaves. He was able to come and be with me during the entire transplant, which was 30 days in the hospital.
Autologous Stem Cell Transplant

Describe going through the stem cell transplant process
We went to the University of Colorado, and that’s where I had my stem cell transplant. They had no problem getting enough cells for that.
It was a really, really hard time. Basically, they kill your bone marrow until it’s basically nothing so that they can restart it.
I was very, very sick. Thank goodness they give you medications so that the patient doesn’t remember a lot of the things.
My husband had to watch the whole thing, and he remembers all of it, but I don’t remember a lot of it.
What was the day-to-day like in the hospital?
It was really cool. I was in a study, and there were 3 things that you could randomly be picked for. One was a friendly visitor, music therapy or a massage. I got a massage! That was really cool that I got to do that, but I remember I had to journal in this book for that massage study. The first few days were really coherent. I could read my writing, and I was saying things that were happening.
Then as it went through, it just became just this scribbling and you could not read a word of it. The lady’s like, “Well, it’s pretty typical, because you’re just so sick and you’re just barely hanging on in some ways.”
It was a difficult time. It was all in the hospital, where if anybody came to visit, you had to gown up and be germ-free as much as possible.
We had a lot of visitors. We had different people coming in to show their support, which was really great, but it was a difficult time.
How was the recovery from the SCT?
I had to be there a month before the transplant to get the cells and then a month after for just making sure I’m okay to go home. We spent the whole summer of ’98 in Denver in my mom’s house or at the hospital.
It was a big deal, but boy, I came out of it great. It took about a year where I wasn’t feeling sick all the time and building my strength back.
How was dealing with all the travel for transplant follow-up?
When we lived in Rock Springs, I was going back every 3 months, and it was difficult because they were doing just extensive testing every time. I would have to take the kids out of school. My daughter was in school. We homeschooled her for kindergarten, and then we put her in school for second grade. We took her out of school for 2 weeks each time.
Every 3 months, we go to Denver for 2 weeks. They do a bunch of testing, a day’s worth, we stay there, and then we have to go back for the results and different things like that. That was a hard time just getting through that and going up every 3 months.
Then, once they realized that I was doing great and that the stem cell transplant seemed to have worked, I went every 6 months.

Moving to a bigger town
Then we moved to Cheyenne, Wyoming, which was a lot closer to Denver, which was nice. I was going about every 6 months, and then they released me to just a local oncologist in Cheyenne, where they have oncologists, which was nice. I did a 6-month checkup then with that oncologist there in Cheyenne for many years, and I worked.
I lived a normal life. I felt great. I was exercising. I was doing everything that a mom does for her kids growing up.
They were getting older and in junior high and high school by then. It was just like, “Hey maybe I’m in remission forever.”
They had told me, “Give us 10 years, and we’ll maybe have a cure by then.” That didn’t really happen, but I had a long time where I could just live my life, so it was nice.
How did you manage the stress of a having a possible relapse?
It was difficult, because every time we go to the doctor, it was like, “Okay, is it back?” Even though they said give us 10 years, they also said 99% it will come back.
Each time we’d go, we have this dark cloud over our heads thinking, ‘Is this the time when it’s going to come back?’
It was hard because I was always feeling pains. What is this pain? What is this pain?
It was just always a mind thing where I was just dealing with that all the time. I guess, for us, we just have a tremendous faith in God, and that’s the biggest thing that helped us was just to have trust in Him and know that He has the best plan for me.
We just went that way along the whole journey, and I’m just so thankful for that because I don’t know how I would have done it without that in my life.
VIDEO: Multiple Myeloma Relapse

1st Symptoms of Relapse
What were the symptoms you experienced for the relapse?
It was really strange because it came on suddenly. Now that you look back on it, and you think, “Well, maybe there was pain there, and I just ignored it.” It just really came on suddenly.
We were out of town, and I was sitting on some steps. I think it was a sneeze, and it just popped in there. I just had so much pain.
That’s when we went to an emergency room. I couldn’t breathe, I couldn’t sit, and I couldn’t lie without being in excruciating pain.
Of course, then I start thinking, “Myeloma.” We really hadn’t seen it for 12 years. They couldn’t see anything on the X-rays at the emergency room.
The oncologist didn’t see anything
I went back to the oncologist. He didn’t see anything. The light chains test was pretty new back then. He didn’t have a history of my light chains, so it was difficult for him to say, “Oh, well, there’s a trend. It’s going up.”
I felt like we needed to do something because those light chains were going up. He just felt really confident that there was nothing going on.
Mentally, it was just really hard because I was like, “I think there’s something going on.” I just put it to the back of my mind.
The Relapse Diagnosis
How did the relapse get diagnosed?
We moved all over Wyoming, but when we moved to Casper, we saw the doctor here. He found a big plasmacytoma on those ribs. I’d been telling him about other pains. I was having pain in my skull at that time and in my femur and my hips.
He did some scans, and he’s like, “Well, are you having pain in your ribs on the right side?”
I was like, “Yes, for about 2 years at this point. I just don’t tell anybody about it anymore because I thought it was nothing.”
He’s like, “Well, you have a large plasmacytoma on those ribs, and it’s obviously been growing for a long time.”
Another example of importance of speaking up
I don’t know what happened with those scans and why you couldn’t see [the plasmacytoma] in those. It was just very strange.
Once again, it was one of those things where I wanted to fight for myself and say, “Hey, you need to listen to me. I am having these issues, and no one’s listening to me. You’re just blowing it off.”

I’ve had that experience so many times, and I’ve learned over 23 years now how to say, ‘Wait a minute. I know something is going on. We need to keep investigating this until we figure it out.’
For me, I’m not a pusher-backer. I want to trust my doctor, I want to do what he says, and I want to follow all of his recommendations. I’m not one to push back. It takes me a long time. It’s really hard. I cry, and I get really emotional about it.
How have you learned how to speak up with your doctor?
I’ve just learned how to have a conversation with the doctor. It’s taken a long time to be able to do this in a way where I’m just saying, “Hey, there’s something wrong here, and I need you to help me with it. Is there anything else we can do?”
My doctor and I have really come to that place where we’re able to have those conversations really easily.
It is hard because you want to trust them, and you want to put your faith in what they have to say. At the same time, you have to advocate for yourself.
»MORE: How to be a self-advocate as a patient
2nd-Line Treatment
Describe the radiation therapy
Beth had 193 radiation sessions starting from her first-line treatment, mostly focused on the sternum area.
Fortunately, with multiple myeloma, they can use low dosages. It’s really, really effective. Every time I’ve had those 193 treatments have all been effective for me. It immediately started reducing the pain from the lesions.

I’ve had several tumors. I’ve had a tumor behind my eye, I’ve had tumors in my ribs, and on my sternum, different places in my skull. They just reduce them quickly. I only have to have 12 treatments, and then that’s all they would do.
What were the radiation side effects?
- tiredness, fatigue
- redness
- some hair loss
Thank goodness, the side effects were very minimal. There’s definitely tiredness and fatigue, even redness. I didn’t even have burns or anything.
I lost some hair when I had to have some done up here, then part of an eyebrow. That causes hair loss a little bit.
Mostly, I didn’t have nausea. I didn’t have anything like that. I think I’m really fortunate because of my age and being young and going through all of that. I’m still young for being treated for multiple myeloma.
I think that’s an advantage for me, in that my body handles it pretty well. It’s getting harder and harder, I think, as it builds up in your system and you have so many [tumors]. Even this last one that I had a year ago, it was on my ankle, and I didn’t have any real side effects except for maybe a little bit of fatigue.
Then, that’s very different for myeloma patients. I’m in the oncology center with all different kinds of cancers.
Some people have a really hard time with radiation. They have to deal with the side effects that I didn’t have to deal with.
Describe the chemotherapy, side effects & what helped you lessen them
Beth says she underwent 9 different chemotherapy regimens, starting with first-line treatment.
Bortezomib (Velcade) + Cytoxan + dexamethasone
- fatigue (biggest)
- some nausea
I think that there’s some nausea that happens with it, definitely fatigue. I think, for me, that the biggest side effect of all of the chemotherapies that I’ve done is fatigue. Also some nausea, but they’re so good now with medications, where they have a 3-medication regimen.
You start with one, and if that doesn’t help, you go to 2. Then if that doesn’t help, you go to 3. Usually, by the second one, I’m feeling pretty good. I’m feeling a lot better. That has been really helpful for me as those 3 medications for nausea.
They also will give you something to help with that. If you’re doing an IV treatment that day of chemotherapy, they’ll start with something that will help with nausea.

Dexamethasone (steroids)
- blood clots, even a pulmonary embolism
- pulmonary hypertension (fluid in lungs)
- insomnia, difficulty sleeping
- weight gain
- anxiety
- mood swings
- cataracts
- shortness of breath
I’ve had some other side effects, like with the dexamethasone. I’ve been on that so long. It’s a steroid, and so it caused the blood clots. I had a pulmonary embolism, actually 2 clots in my lung from being on that long-term. They thought it was in my ankle, and they did an ultrasound. They couldn’t find it, and then 3 days later, it was in my lungs. That was definitely a scary side effect of the dexamethasone.
The dexamethasone is a hard medication. It causes me to not be able to sleep, so I still do it twice a week. I take it orally, and it causes me not to be able to sleep. It causes me to gain weight. It causes me to have what they call “moon face.”
It causes anxiety. Every time I’ve done treatment, it had been dexamethasone, and it’s been at different dosages. Because of some of the things that I’ve been through, they went back up to a higher dose. It’s like the maximum dose that they’ll give someone in a week.
Anyway, when we started this, I was so angry all the time. Anything my husband said, I would just lose my mind, and that’s just not me. That’s just not my personality. I would just get angry, and I would yell, and I would be so mad.
Then we adjusted it for a little while, and then went back up on it. Now I’m doing a lot better. I’m able to see it coming a lot better so that I can take the steps of walking away from the situation or just closing my door for a minute and taking a breath.
The not-sleeping part is really difficult, so 2 nights of the week, I don’t sleep much. The weight gain is really difficult as well. Every time I started, I gained anywhere from 10 to 30 pounds. That’s been really difficult. It’s really hard then to lose that weight.
My radiation oncologist is always saying, ‘Don’t worry about it. You know, there’s nothing you can do. It’s chemically changing your body. Just do the best you can, eat as healthy as you can, try to stay away from sugars, those kinds of things, as much as you can. That’s all you can really do with that dexamethasone.’
But there’s a lot.
It also causes other things, like cataracts, and there are other drugs that I’ve been on that caused cataracts. There are just a lot of different things with dexamethasone.
I just was diagnosed about a year ago with pulmonary hypertension, and they’re pretty sure that that’s basically where I get a lot of fluid on my lungs. I struggle with shortness of breath and having to use oxygen and that kind of thing.
It put me in the hospital with pneumonia several times, and they think that some of the drugs that I’ve been on have caused that to happen. Just the long-term effects of some of these medications can be pretty harsh.
You just have to find ways of dealing with it. Right now, I’m on a lot of diuretics to help with the fluid in my lungs and then on my body. That helps with the pulmonary hypertension. Anyway, there are so many things.
How did you manage the steroid side effects?
We [lowered the dosage] temporarily. Then, when we went back up again, it was fine. I was able to deal with it. Right now, I’m handling it really well at the maximum dose. I just think I’ve just learned. Unfortunately, I had to take it for so long. I’ve learned how to deal with it.
Living Life with Myeloma

Being vigilant with myeloma symptoms
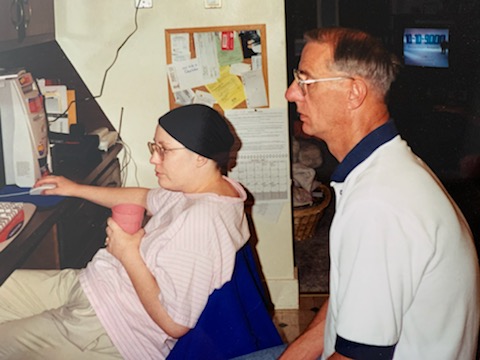
With the tumor in my orbital bone, you can see in that picture that my eye was starting to droop. My left eye, which is the one closest to my son, Zach, was starting to droop down.
It was starting to close and moved down my face, in a way. If you saw the MRI scans, you would see that there was a tumor on my orbital bone. It was pushing into my brain a little bit, and it was pushing my eyeball down my face.
In this picture, I had no idea that this was happening to me. I just kept looking at myself in the mirror going, “That eye looks really droopy.” I would ask people sometimes, like my husband. I’m like, “Does that eye look droopy?”
He’s like, “Oh, I don’t know, maybe.”
I just thought maybe it’s just something that was happening to me as I got older. I was not sure. Then, one day, I was at oncology, and I asked one of the nurses. I said, “Look at my face, and tell me if you think my eye is drooping.”
One of the nurses is like, “Yes, I can totally see it.”
I went in and then saw our PA (physician assistant) there, and she’s like, “We need to go get an MRI right now.” That’s when they found that tumor there, but this is very typical of how my life goes.
Pain and M protein
I’m sure I had some bone pain there for a while. I have bone pain in my ribs, and I think to myself, “Is it old? Is it new? What is happening in these places? Is it nothing? Is it muscular? Is it bone pain?”
A lot of it, too, is because I don’t show the M protein. The only way that they really see the progression of my disease is through pain. It’s through the light chain test.
If my light chains just barely go up… People live in the hundreds in their light chains. If I go up to 7, I know I’m going to start getting lesions somewhere.
That helps a little bit because then I can look at that and go, “Oh, if I’m at 10, then I know that this pain could be a lesion somewhere in my shoulder and my arm and my leg.” It’s just a constant everyday thing where I’m guessing about how I’m feeling. It’s hurting.
I went for a long time thinking my ankle was just twisted or hurt, and I was hobbling around and limping. Finally, my doctors are like, “We need to do something about this. We need to look and take a scan of it.”
Sure enough, there’s a tumor in my ankle. I had to end up wearing a boot for a while, and they did radiation on it. It’s just how my life goes all the time. It’s just those kinds of things.
What helps motivate you to keep pushing forward?
That’s probably one of my biggest struggles — how to live your life like that, because I’m sick a lot. The last year has been really hard. When I go to oncology, they push me around in a wheelchair. I was walking around my house with oxygen on because I wasn’t able to breathe, or hobbling around in a boot because my ankle had a tumor in it, all these things. How do I beat that? It’s really hard.
I guess the biggest thing for me is if I’m going to go through this, I want to help others who have to go through it.
At the oncology center, we have a couple of myeloma patients there. There’s not a lot, but it doesn’t matter. There’s other people with cancer that I can talk with and let them share their story with me.
Being “Beth with Myeloma”
Being “Beth with Myeloma” isn’t so bad all the time because I want to help other people and be a part of their journey and just be there to listen to them. I don’t know. It’s a really, really difficult thing to manage. I just live with it. I guess I just live in it, being “Beth with Myeloma.”
When I was working as a teacher, there at the end, it was just really hard because I was needing accommodations. I needed people to help me get my kids to other classes, I needed my oxygen in my classroom, and I needed all these things.
I just became “Beth with Cancer.” It’s okay. I don’t mind it too much. If people want to talk about it, I’m always willing to talk about it and share my story and see if I can encourage anyone. That’s where I’m at after 23 years.
VIDEO: Relapsed Refractory Multiple Myeloma Treatment

CAR T-Cell Therapy
How did your oncologist describe the CAR T-cell therapy option?
Find this video clip at 00:56
He described it like a bone marrow transplant in a lot of ways, but a lot less harsh on the body and less extensive as far as time in the hospital.
He said I’d have to go somewhere with a big hospital, where I’d receive treatment. I’d have to stay there for a few months to get the treatment throughout the whole thing. That was a difficult proposition to do.
My mom lives in Denver still. She’s currently living here, so it’s going to be even harder if I decide to do that eventually. I’d have to live with my mom and travel back and forth to the hospital, so that was something to consider. Also, I had been on Blenrep. It did not work for me.
The doctor and I just had a conversation about 2 weeks ago about it, and I asked him about CAR T. I said, “If this treatment that I’m on right now, the selinexor, if it stops working, what’s the next step? What do we have left?”
We’ve gone through so many things. The list is getting shorter. Although there are so many things that come out on the market constantly, so it starts to add down at the end, it is getting shorter for me. CAR T is one of the things I could possibly look at.
Belantamab mafodotin (Blenrep)
How was your experience with belantamab mafodotin (Blenrep)?
Find this video clip at 4:03
Now, I can even hardly remember. I think it was oral. I only did it for months because I wasn’t seeing a good result from it.
What were the side effects?
- Eye-related problems (keratopathy):
- dry eye
- itchy
- cataracts worsening (started from previous treatment)
- double vision (no driving, reading)
When I was on it, I’ll tell you, the dry eye was just terrible. You just had to constantly be putting gels and creams and drops in your eye just to try to not go crazy because it was just so painful, and it was itchy and hard to deal with.
Also, I had cataracts forming from when I was on Revlimid, and the dexamethasone also causes it. It wasn’t bad enough to do surgery, but when I went on the Blenrep, I was having all these problems. I couldn’t see; I was having double vision. It’s crazy. A nice lady from our church would come to my house, and she would read to me.
She was a former school librarian. She would bring books that she loved to read to her students, and she’d come and she’d read to me because I could not read.
It was so nice. What a kind thing that she did.
Anyway, it was that bad where I’m still struggling. I had cataract surgery. It caused the cataracts to become so bad that they had to do surgery on both eyes. They just did some laser treatments on it to try to finish some of the cataract stuff up.
I still can’t read. I have to use glasses on top of glasses in order to read right now. They’re still working on that, but it’s all since the Blenrep.
It’s hard because it didn’t work for me, but I still had to go through all this. I really haven’t seen normally, I bet in at least a year and a half, pretty close to 2 years. For a long time, I couldn’t drive.
My husband had to drive me to all my appointments, and friends had to drive me. I finally can drive now, which is great, and I appreciate that. That makes me really happy, I can get out of my house.
What helped with the Blenrep side effects?
Find this video clip at 7:41
- Eye drops
- Resting
The eye drops and things like that. I think rest was really important. I laid with my eyes closed a lot. That seemed to help keep them lubricated a little bit more.
I think just trying to have a good attitude and saying, ‘This is going to pass. We’re just going to get through this.’
I saw an eye doctor every week before [treatment], and they’d have to check to see if it was too bad. If the keratopathy was really bad that week, they would not treat. They would skip a week, and go and treat the next week if the eye doctor gave her approval.
That was helpful, as far as them monitoring me all the time. I appreciated that. The eye doctor and the oncologist kept in constant communication.
What was the Risk Evaluation and Mitigation Strategy (REMS) program for the eye problems?
Editor’s note: The REMs program is part of the Blenrep regimen.
Find this video clip at 8:39
Every time I went, they would do all the little pre-tests. They would do a normal eye exam. Then she would come in, and she could look at the cornea to see if there was too much inflammation. She could totally tell the extent of the dryness of my eye.
She would just look manually with her tools that she had. That’s really what it was. It took maybe 10, 15 minutes each time, and she was really great.
It was interesting to her. She’d never had this happen to anyone before, so she was really interested in it and did some research. It was great as far as that goes.

Selinexor (Xpovio) + Bortezomib (Velcade)+ Dexamethasone Combination (SVd)
How did you learn of this treatment option?
Find this video clip at 11:02
My oncologist had said, “There’s this new combination coming out. The selinexor (Xpovio) is pretty new, and then with Velcade (bortezomib), let’s just see if this works.” It wasn’t even out on the market yet.
He was able to get the insurance company to approve it each separately, which was really great because I was able to start, and I was in a desperate situation.
What was the status of your myeloma?
Find this video clip at 12:05
- 4 in x 3 in x 3 in tumor on sternum
- light chains, normally around 0 to 1, up to 70
- weakness
- shortness of breath
I had a tumor on my sternum that was 4 inches by 3 inches by 3 inches. We’re talking inches here. We’re not talking centimeters; we’re talking inches. It was clear across my chest and visible, and it was just growing like crazy.
It was just out of control. My light chains, I’m normally around zero or one, and then I was up at 70. I’d never been at 70 before, and that was really scary, and I was feeling terrible.
Most of the symptoms of myeloma that I’ve had are just mostly pain and maybe some fatigue as far as the symptoms of the actual cancer. But at this point, I was weak. I was short of breath.
I was having to be pushed around in wheelchairs, those kinds of things. Just not doing well at all, and actually, we did an interview with the doctor. He would never say this to me face-to-face, but he later said, “I wasn’t sure what we were going to do. I didn’t know what our next steps were going to be.”
He’s always been so up and positive with me, and he said, “We have a lot of tools in our toolbox,” all these things. That’s the first time I’d ever heard him say something like that, so he was really excited about this new combination because the Velcade had worked for me before, and we didn’t stop it because it stopped working.
We stopped it because of the neuropathy, so they didn’t want to continue and see if the neuropathy would reverse itself and all of that, which it did a little bit.
We knew that the Velcade was a good fit for me, and then with the selinexor on top of it, he was just really super excited about it.
Describe the selinexor + Velcade + dexamethasone (SVd) regimen
Find this video clip at 14:08
When I first started, I started on 100 milligrams, which is the highest dose, but you can adjust that dose to a lot of different things. I started on the 100, and then 40 milligrams of dexamethasone a week, so 20 on one day, 20 on another day, and one shot of Velcade a week. I would just go in, get the shot for Velcade, and then go home and take the dexamethasone and the selinexor.
Describe the selinexor, bortezomib and dexamethasone combination side effects
Find this video clip at 14:51
- food tastes different
- some fatigue (Beth thinks it’s caused by the dexamethasone)
- some nausea
The side effects are pretty minimal for me.

The biggest thing that I experienced is that my taste is different, so food doesn’t taste the same. It’s funny because it’s not listed as a side effect. I went on a support group of selinexor patients one day, and there was a special speaker. She said that it’s not listed, but she hears it from several patients. They may have to start listing it.
Anyway, that’s one bad thing, because nothing tastes good to me at this point, even chocolate. It’s not as bad as when I did VAD. When I did VAD, I couldn’t even stand the taste of chocolate. I could kind of eat it, but it just doesn’t taste the same anymore. That’s the biggest thing.
I do experience some fatigue. I think that’s a lot of the dexamethasone. I’m on it for 2 days, and I’m on this high, and I’m not sleeping and I’m full of energy. Then it drops way down, and then I’m feeling so tired, and maybe the effects of the selinexor kick in more, or I feel them more. A little bit of nausea where I’ve had to do the 1, 2, 3 medications, but really not that much.
It really has made me feel so much better. I’m like a different person than I was 6 or 8 months ago. I’ll just say that the first week that I took it, the tumor on my sternum just went down by half, and then my light chains dropped from 70 to 25.
Then the second week, you couldn’t even tell I had a tumor. It was completely gone. My light chains were down to zero. Well, 0.1 or something like that.
It’s just made a huge difference for me, and we’re just hoping that it continues.
What has helped you manage the side effects?
Find this video clip at 16:51
Adjusting the dose
We’ve had to adjust the dose because of my platelets. It really affects my platelets, especially because I’ve just had a crazy few months where I’ve had 2 cataract surgeries. I had to have my port replaced. When you do surgeries, you got to make sure your platelets aren’t too low, so you don’t bleed too much.
I’ve had to skip some treatments because of those things. They’ve gone down to 60 milligrams right now because my platelets are so low all the time, they won’t recover like they’d want them to. Some of my other numbers are pretty low, but they’re kind of borderline. Sometimes I’ll do 80, and sometimes I’ll do 60. I haven’t been up to 100 for a while.
My light chains have gone up a little bit from zero to 3, but they’re staying steady at 3, which is great and I’ll take it. I think if those start to go up again, they’ll probably increase the dose and try it at 100 again.

The “1-2-3” anti-nausea medication plan
Video time code: 18:19
- Ondansetron (Zofran)
- Prochlorperazine (Compazine)
- Lorazepam (Ativan)
The first drug is Zofran, and I’ll tell you what, when I was first diagnosed, Zofran was like $20 a pill. It was so expensive, and now it’s not expensive at all. That’s the first line of treatment for nausea. You take that.
If you’re not feeling any better from that — and that usually does the trick for most people — then you take Compazine, which is prochlorperazine, but that one does it for me every time.
I just love that drug because it does it for me every time. If the Zofran doesn’t help, if I take Compazine, then I’m feeling so much better.
Then the last one is Ativan, or lorazepam. That one is for anxiety mostly, but it does help with nausea, and it helps calm you down. That’s the third line. If you’re really still feeling sick and nauseous, the last one is Ativan, which a lot of cancer patients are on and take anyway for anxiety and different things. It helps counteract some of the dexamethasone side effects as well.
Anyway, that’s the 1-2-3, and it’s wonderful.

What’s the real impact of finding a new treatment that finally works for you?
Find this video clip at 20:35
When I was going through it, right before the selinexor and things weren’t working, we were trying all kinds of things, and the doctor was feeling he wasn’t sure what we were going to do next. I was feeling so bad physically.
It was also really hard emotionally because I kept thinking, “We’re down to the bottom of the list. There’s nothing else left.”
I’m going to have to do CAR T, which was fine, but it wasn’t really what I wanted to do at that point. All these things.
I would cry a lot. Everything would make me cry, and that just wasn’t my personality.
They were giving me medications to help me with some depression issues, so I wouldn’t cry about every single thing. That helped while I was going through that.
When we started the selinexor, it was like a new beginning to my life in a lot of ways.
I’d been really suffering for over a year, not really knowing what was going to happen. I’m a pretty upbeat person. I don’t get caught up in the hard stuff too much, but this was one of those times where I really did.
I read the stories about the people with myeloma and people my age who are dying because they’re just not responding to treatment. That’s where my mindset was really going. “This is going to be the end.”
I also had a friend with breast cancer who was dying at the same time, and so we were kind of going through it together. It was really hard, and she actually passed away during all of that. That just made it hard, too, because I thought this is where I’m at. I’m going to follow this same path.
It’s been kind of surprising the way that the selinexor has worked. I wasn’t expecting it, so it’s been great. I feel great, and I’m hoping that it just keeps going.

VIDEO: Living Life with Multiple Myeloma

Quality of Life Impact
The decision to retire from work
It’s been hard in a lot of ways. I had to retire from teaching. I think that was one of the hardest things because I just felt like I can do this. I was working 50 to 60 hours a week as a teacher.
It took me so much longer to do anything because I was tired, I was weak, and I was experiencing different side effects throughout different therapies.
It was really difficult to make that decision to say, “You know what? I can’t work anymore. We’re going to have to figure this out financially,” because cancer is so expensive.
I’ve just been thinking a lot about how many cancer patients feel like they have to work because they have to keep their insurance. They have to have money to pay for treatments. It just amazes me to think what people have to do to even get treated.
Thank goodness I have good insurance and we were able to get on long-term disability through my school district, so I was able to stop working. That was probably one of the hardest decisions that we had to make because I loved teaching, and it made me feel like I was normal, like I was doing something like every person does.
I felt like I was contributing to the family for so long. Even during my remission time after my transplant, I did some work. It was tutoring and substitute teaching, those kinds of things.
I just didn’t feel like I was really contributing to the family, but once I got my own classroom and I was teaching, I just really felt like I helped. It just felt like for so long I was pulling resources away from our family because of cancer. We were traveling so much.
You just make different decisions financially than you would if you didn’t have cancer. We spent money where we shouldn’t have. We made a lot of bad decisions too, but anyway, I just think those are the things that just have been the hardest for us, traveling through this journey. I guess that’s what I have to say about that.
»MORE: Patients talk about working during cancer treatment
Guidance to others on getting support paying for treatment
I think the biggest thing is to be in communication with your supervisors and administrators. For so long, I just tried to do it on my own, do it on my own, do it on my own. I tried to act like there was nothing going on with me.
Finally, I just had to because I was taking time away from work. I was leaving for treatment 15 minutes early. I had to run to my car before the bell rings so that I could get out of the parking lot before the parents started moving, and people had to cover my class.
There were times where I was doing 6- to 8-hour treatments. I’d have to take the day off, find a substitute, write sub plans, all of these things that were so hard to do while I was doing treatment, but I just did them anyway.
I would ask for the time off or ask for help finding coverage, but I didn’t really share what I was really going through. I think once I started doing that — and it doesn’t happen in every situation, but in my case — my administrator was really helpful and worked it out so I wouldn’t necessarily have to take all my sick leave all the time when I was leaving just 15 minutes early or whatever. She would work it out so that I could come in earlier, do this or that, so that I could cover that.
She helped me get some accommodations to the district. I was allowed to sit while teaching because that was a rule in our district that you need to stand while you teach, and I just couldn’t all the time.
I found an accommodation where I could sit while I was teaching, I could have my oxygen in my classroom, and I could have people help me take my kids [around]. I didn’t have to walk across the building all the time on days if I wasn’t feeling well.
If I hadn’t been in communication, I wouldn’t have been able to get that kind of help through her.
When I was thinking about retiring and quitting, they were really helpful with what are the best things to do:
- Is it best to just quit?
- Is it best to retire?
- How do you apply for long-term disability?
- Is that an option for me?
- What are the steps?
She put me with the right people.
»MORE: Find more resources on finances during cancer treatment
Finding resources to help navigate these life with cancer questions
I think communication is the biggest thing. Also, I talked about it before, but it’s helpful to just ask, “What are the things, what are the resources that I have to help me go through this?”
Most people are so kind and willing to help.
I am on some myeloma pages on Facebook, and a few people have talked about how it’s been really difficult in their job situations, dealing with their administrators and things like that.
It’s just a hard decision. Do you leave your workplace? Do you go and try to find something that you could do at home or something less physical?
There are just so many options. I know that people need to still work and still have insurance, but there are options out there. You’ve just got to research and ask. You have got to follow up on things. It’s hard to because I feel like that’s a full-time job.
For a while, it was a full-time job just scheduling appointments, trying to find coverage for my position at work, and all of those things. Then there was calling all these places asking about whether I could do long-term disability, all those things, and it’s just like having a whole other job. It’s hard. It’s really hard.
Support and Acceptance
How important is it to have a caregiver through treatment?
I’ll tell you, I have the best caregiver on the planet. My husband does everything for me.

Sometimes stairs are really difficult for me to navigate because of some dizziness and some just weakness, so he does all the laundry, he cleans the house, he does the cooking, and he just takes care of me.
Especially when I was teaching, he just had decided, “She has to go through this and treatment and work these 50 to 60 hours a week, so I’m going to do everything else, plus my 40-hour week job to take care of her, and all she has to concentrate is getting well.”
He was working at that time, and even though I’m not working, he still does pretty much everything for me.
I’m really blessed with that, and I know that’s not everybody else’s experience all the time.
Sometimes that has caused us to not accept help outside of our little 2-person family, now that our kids are gone. I think we could do better at that.
Accepting support from others
There are people at our church and at school who wanted to help more and bring meals sometimes. We had some people help us when we were moving, give us extra help in cleaning the house that normally I would have done that I couldn’t do.
It’s so hard to accept someone’s help, but they really want to find some way to help you. Giving them that opportunity is really a blessing to them.
We’ve really realized the value in giving other people the opportunity to help. We don’t have family here. It’s just us, and now my mom is here, but she’s 83.
It’s an interesting thing. She helps me. It’s funny. The other day we went to the grocery store, and she’s holding onto my arm because I’m probably going to get dizzy.
She’s this 83-year-old woman, all these people are probably thinking, “Oh, that’s so nice that her daughter is helping her along the parking lot,” but it’s really her helping me. That kind of support and some emotional support are important.

Different styles of support from family members
My daughter really struggles with it. She still doesn’t like to talk about it a lot. She likes to hear what is happening as far as tell her just the nuts and bolts, but we don’t really want to talk about it too much. She was really affected when she was 5 with that whole thing, and then on and on and on for her whole life.
We’re still working on some of that with her, but I think we’re at an okay place where I feel like if I really needed to talk to her about something, I could.
My son is all over it. He loves to talk about it. He’ll ask me lots of questions, those kinds of things.
It’s hard sometimes to just accept help and support, but we try.
Clinical Trials
Would you ever participate in a clinical trial for myeloma drug research?
I don’t know a ton about it because I’ve never done one, but when I’m on those pages with all those myeloma people on Facebook, they talk about it a lot. They talk about, “Please do the clinical trials if you can.”
I think it’s really important. I would love to be able to do them when we come to that place where I really don’t have a lot more options, but I did hear from someone that being non-secretory could make it difficult. That might exclude me from a lot of different clinical trials. We really have to look into it and see what the exclusions are and see what happens with that, but yes.
I’m all for it. I think if patients can do it, they should do it.
Dealing with the logistics of participating in a trial
I know that it can be expensive. For me, it would be really expensive because we live in a small town in Wyoming, and we’d have to travel somewhere to do it most likely.
That’s a real problem for us. Right now we could probably do it better than we could 10 years ago, but there are a lot of considerations like that that patients have to walk through.
There’s a lot of testing. There’s a lot of that kind of thing. It’s not an easy decision to make, but I think that it’s so important if we can get these things out on the market for patients, for the wide audience that needs it.

Living with Multiple Myeloma
Finding purpose in helping other myeloma patients and caregivers
It’s been just a crazy year. All these opportunities to share my story have come up. I’m just so grateful for that because I think sharing your story, for me at least, helps me to process what I’ve been through.
It helps me remember, because I think it’s important to remember what we’ve been through. It helps you make decisions in the future, and it just helps you to give yourself some grace.
I don’t give myself grace very often, as far as when I feel bad or tired or anything. I think, “Ugh, I’ve got to feel better. I gotta get up and do stuff. I got to push through this.”
Then if I tell my story, I think, “You know what? You’ve been through a lot. This is okay to feel this way this day.”
Reconciling being a cancer patient and not “looking sick”
I think we just are hard on ourselves, and we don’t let ourselves be sick, especially myeloma patients because we don’t look sick. We don’t often show that we’re sick.
I look like I’m not sick. It’s really hard to balance that with “I am sick” and “I need to be able to take care of myself, and I need to not push it too much, and I have to give myself some grace.”
I think that’s one of the biggest things. Just be in good communication with your doctors, and like we talked before, just be an advocate for yourself and not be a pushy, annoying patient.
Sometimes you have to be, but just do what you have to do and be in communication and conversation about it and ask a lot of questions. Do research, but be careful where you’re doing your research. Make sure that you’re looking in good places that have real information.
This is another thing that I think has been one of our biggest things we’ve dealt with. There’s so many people that want to help, and they have good intentions. I’ve been told I need to take this supplement or read this book or do this thing. We were told to do coffee enemas. We were told to take curcumin, which is proven actually to help some people with myeloma. We had someone tell us, “Don’t talk about it. Don’t put anything negative out into the universe, and your cancer will be healed.” Those kinds of things.

We’ve had difficult situations like that, and I think that’s a hard thing to wade through because you want these miracle cures to work. People are always saying, “They’re going to work. They’re going to work.” Often they don’t work.
You have to wade through that, and you have to decide, are you going to change your diet? Are you going to take supplements, whatever it is? It may help you; it may not help you. That’s a difficult thing that we’ve had to wade through.
We’ve had some difficult relationship issues with that where people are upset because we won’t do what they want us to do. “Oh, you’re going to be healed if you do this.” We’ve chosen to do the traditional medicine type thing mostly. I do some things natural, like for side effects and things like that.
As far as treatment for myeloma, we’re doing all traditional medicine, but other people have other choices. It’s a big thing that people have to wade through. I think it’s tiring and I think it’s hard.

Inspired by Beth's story?
Share your story, too!
Multiple Myeloma Stories
Theresa T.
Diagnosis: Multiple myeloma, relapsed/refractory
Subtype: IgG kappa Light Chain
Initial Symptom: Extreme pain in right hip
Treatment: Chemotherapy, CAR T-cell therapy, stem cell transplant, radiation
Laura E.
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
Donna K.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: None, found by blood tests
Treatment: Total Therapy Four, carfilzomib + pomalidomide, daratumumab + lenalidomide, CAR T, selinexor-carfilzomib
Connie H.
Diagnosis: Multiple myeloma, relapsed refractory
1st Symptoms: Chronic bone pain
Treatment: IV Chemotherapy, CAR T cell therapy
Elise D.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: Lower back pain, fractured sacrum
Treatment: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
Beth A.
Diagnosis: Multiple myeloma, relapsed/refractory
Subtype: Non-secretory (1-5% of myelomas)
1st Symptoms: Extreme pain between shoulder blades, sternum, head, burning sensation
1st Line Treatment: VAD chemo, radiation, stem cell transplant
RR Treatment: 8 chemo regimens, successful combo→selinexor+bortezomib+dexamethasone
Scott C.
Diagnosis: Multiple myeloma, relapsed/refractorySubtype: IgG lambda (majorityof myelomas)
1st Symptoms: Pain in hips and ribs, night sweats, weight loss, nausea
Treatment: Clinical trial, chemo, kyphoplasty, stem cell transplant







One reply on “Beth’s Relapsed Refractory Multiple Myeloma Story”
Congratulations on your journey I pray that all continues to go well you are in my prayers