Clay’s Relapsed Refractory Multiple Myeloma Story
Clay shares his multiple myeloma story and undergoing extensive treatment, with three different chemo regimens, radiation therapy, and both autologous and allogeneic stem cell transplants.
Explore his story below, where Clay also highlights managing through graft versus host disease (GVHD), dealing with the emotions of not being able to go back to work, caring for his caregiver and parenting through cancer.
- Name: Clay D.
- Diagnosis: Multiple myeloma
- Staging: N/A
- 1st Symptoms:
- Persistent kidney issues
- Nausea
- Treatment:
- Chemotherapy
- CyBorD: cyclophosphamide (Cytoxan), bortezomib (Velcade) and dexamethasone
- KRd: (Kyprolis), lenalidomide (Revlimid), and dexamethasone
- VDPace: bortezomib, dexamethasone, cisplatin, doxorubicin, cyclophosphamide, etoposide
- Radiation therapy
- Transplant
- Autologous stem cell transplant
- Allogeneic stem cell transplant
- Targeted therapy: daratumumab (Darzalex)
- Orchiectomy: surgical removal of left testicle after myeloma spread
- Radiation to right testicle
- 25 sessions
- Immunotherapy: elotuzimab (Empliciti)
- Chemotherapy
- Multiple Myeloma Diagnosis
- Chemotherapy Regimens
- Radiation
- Autologous & Allogeneic Transplants
- Multiple Myeloma Reflections
- Transitioning to not being able to work
- How has cancer changed your perspective on life?
- How has your wife handled everything?
- What helped you both with the mental and emotional recovery?
- How were people able to show their support?
- What’s it like being a parent with cancer
- How do you cope with the anxiety of living with cancer?
- What advice do you have for someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Multiple Myeloma Diagnosis
What were your first symptoms of multiple myeloma?
Leading up to going to the doctor, I had had about 18 kidney stones. I had so many surgeries in 2014 for that. I had been going to a nephrologist. We were adjusting my food and medications. It wasn’t getting any better. The kidney stones were still happening.
I went to my primary care doctor because it seemed like the only thing that would help would be to get an IV bag and flush my system.
Days before I was admitted to the hospital, he gave me the IV and did some blood tests. He didn’t really tell me what he was doing. He just said, “You know what, while we’re at it, I’m gonna do some blood tests.”
That happened, and then a couple of days later, I was so nauseous. I looked at my wife and said, “This isn’t a kidney stone. I don’t know what’s happening. We have to go to the hospital.”
How did you get the multiple myeloma diagnosis?
We went to the ER. They didn’t know what to do with me, but they decided to admit me because it was clear that I couldn’t keep fluids down.
I was in the hospital for maybe a day when my primary care doctor called my wife and said, “You need to talk to whoever the oncology specialist is on call. He’s got a protein level that’s high, and I think he might have multiple myeloma.”
It was brutal. I was so out of it that I had no idea what was happening. I can’t even remember it.
It wasn’t the typical experience you think of where you’re sitting across the desk from the doctor.
My wife bore the brunt of it, and it was so hard on her. I think it was surreal for her.
Bone marrow biopsy
At that point, they decided we needed to do a bone marrow biopsy. They wheeled me down to a CT because they needed to do it as a CT-guided biopsy. A priest had somehow found me to come bless me beforehand.
They did the biopsy, and that confirmed that I did in fact have multiple myeloma. They found that 99% of my bone marrow was cancer.
They gave me a mild sedative. It’s like they take a drill and go into your lower back region. You can hear the drill, so that’s crazy. I don’t remember going back to my room after that, so they must’ve given me something to take the edge off.
Processing the multiple myeloma diagnosis
I was in the hospital for about 5 days. Once I got out of the hospital and really realized I had cancer, I was focused on options. I was focused on what options I had and moving forward with those options. I’ve carried that attitude pretty much the whole time.
I met my oncologist pretty quickly. At that point, things are just flying at you. I had a few extra people in the room with me to help ask questions and remember things for me. We all just took that approach.
»MORE: Processing a cancer diagnosis
Chemotherapy Regimens
What was your first-line treatment for the multiple myeloma?
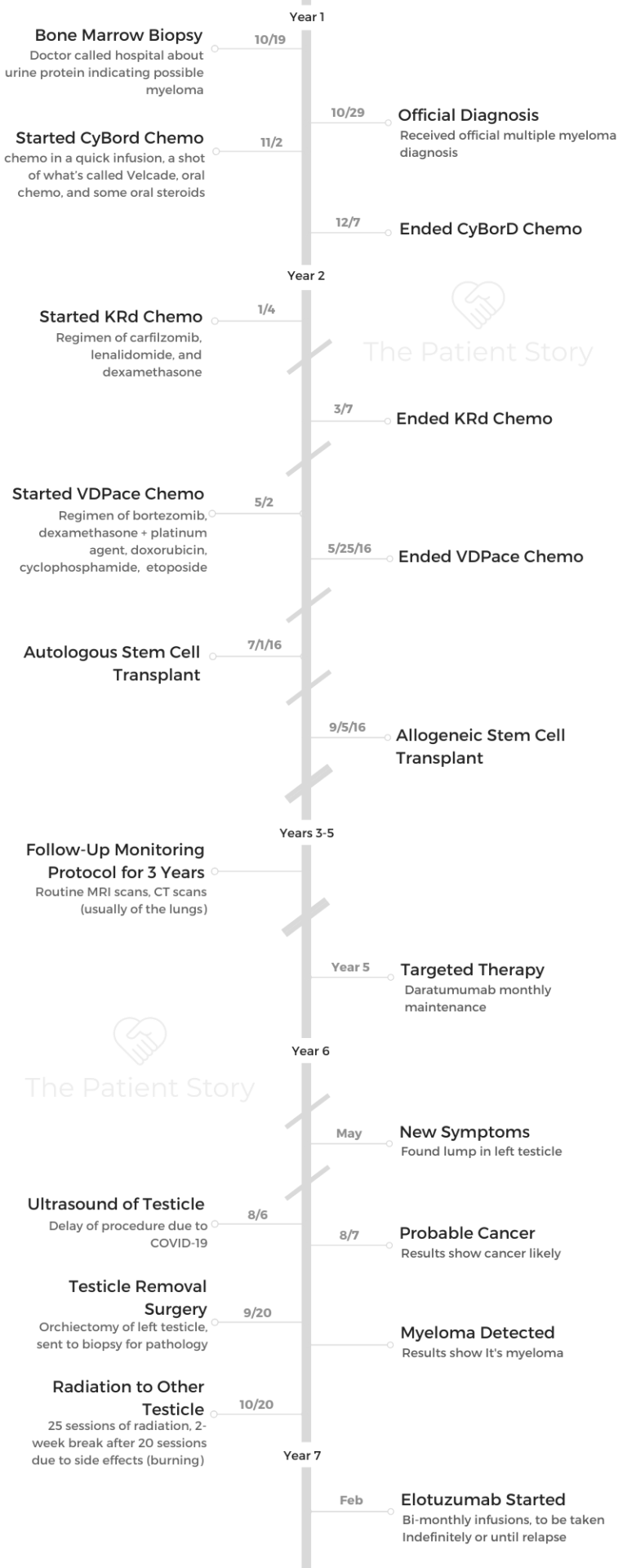
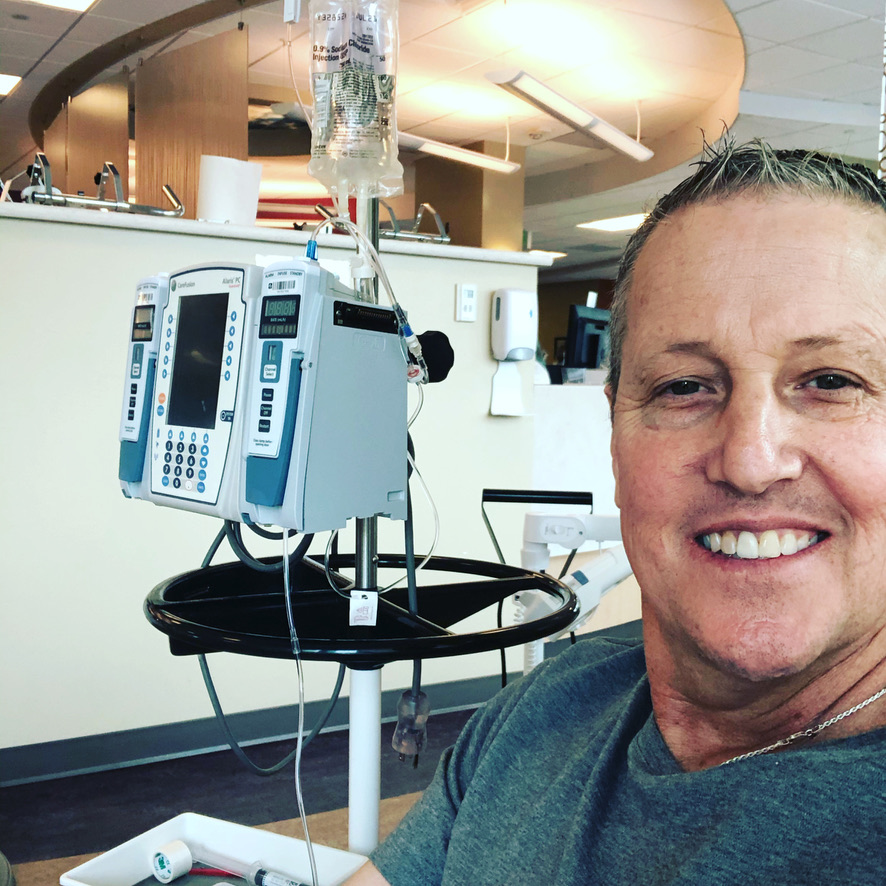
The first step in my treatment was CyBorD. That was some chemo in a quick infusion, a shot of what’s called Velcade, oral chemo and some oral steroids.
They weren’t sure how aggressive my cancer was, so they just had to address it with what was the standard regimen to see how I responded.
I took oral chemo every 21 days with a week off at the end. The same was true for the steroids. I was going in twice a week for the infusions and the shot. The infusions were quick though. They were only about ten minutes.
I was still working at that time. I was in banking. I would have to go home sometimes because I was so tired. I did that chemo for just over a month.
It wasn’t long before they did another blood test and biopsy and determined this wasn’t working.
What was the next treatment you tried?
We switched to KRD. I finished out the course of chemo on KRD. It was pretty similar. It was quick in the infusion lab like the first one. My schedule didn’t change much on the KRD versus the CyBorD.
What were the side effects from KRD?
By the end of KRD, I didn’t feel like going to the gym or anything like that. I think the side effects built up over time for me.
I was fatigued a bit on the CyBorD, but by the end of the KRD, I was really, really nauseous and tired.
Radiation
Describe the radiation
I had cancer in my bone marrow, but I also got three soft tissue tumors in my upper back. I had terrible pain from that. They did a CT scan and decided on a course of radiation therapy.
I did that once every weekday for two months. They were worried about them because the tumors were close to my spine.
Fortunately, the radiation went well.
I responded really quickly to that, and it wasn’t that hard on me. I couldn’t tell how much it was adding to things. Later, I had more tumors in my lower back and one in my calf.
Autologous & Allogeneic Transplants
Chemo infusions (VDPace) before transplant
I did a bone marrow biopsy again after radiation, and everything was indicating that the cancer was still there. At this point, we’d already been planning a stem cell transplant. I needed more chemo before that, though.
I had to go inpatient for VDPace chemo. That was the intensive chemo before transplant. It caused all kinds of problems.
Because I’d had radiation, I had something called radiation recall. This chemo set off a recall of the radiated areas. Because it was in my upper spine, I was getting esophageal problems. I couldn’t swallow or eat. They had to give me a tube.
I spent about a month total in the hospital. Finally, that subsided. Then they started feeling good about how I was responding to those drugs.
Describe the autologous stem cell transplant
On July 1st, I went in to do the actual transplant. Before that, I had more chemo and radiation. They wanted to kill everything bad and start with a clean slate. It was a process to take them out.
Basically, what you’re doing is driving your body to its lowest immune point. You’re driving all your numbers to zero to get ready for your new cells. Then you get the cells. You’re in the hospital and super susceptible to everything. You can’t be around anyone who isn’t wearing a gown and gloves.
You feel crappy for several days, then your cells take hold, and you start to feel a little better.
Describe the allogeneic stem cell transplant
I had the autologous transplant, went home for about a month, and then went back in to get my donor cells. I had the second transplant with donor cells.
My donor was a young girl in Germany. Someone had to physically fly the cells over and hand deliver them.
It’s really the same process, but I’m getting her cells instead of mine. I got sick, didn’t feel good, and then I started feeling better.
I got out of the hospital about a month later, and I had to be within 30 minutes of the hospital for 90 days, so I had an apartment.
Graft versus host disease (GVHD)
I was taking a lot of medications to combat any GVHD issues. I had influenza B, and that was awful. I was probably sick for a month. Even when I was out of the hospital, I was having to go in every day for the first week or two.
I had some GVHD in my mouth. Everything was raw in my mouth. About a year after the transplant, I got what they thought was graft vs. host in my left lung. For the most part, I managed through all that pretty well.
»MORE: Explore more on GVHD and what to expect from a medical expert
Follow-up protocol
I’m still taking chemo three days a week. I take a drug called Revlimid. I take a low dose of Prednisone every day.
I go in for a monthly infusion of Darzalex, which is a newer immunotherapy. It’s becoming more and more popular with myeloma because it does a good job of keeping the cancer at bay. I also get IV immunoglobulin, which just helps boost my immune system.
For the last year and a half, my numbers have been good. I’ve felt great. I walk three miles a day. I don’t know that you ever get back to normal, but I’m doing well. I’ll just be doing this indefinitely unless it stops working.
Are there any side effects with the Revlimid or Darzalex?
The Revlimid gives me some fatigue, but I tolerate the Darzalex pretty well. It’s expensive treatment, but I’ve been so fortunate.
I’m involved with some patient finance programs. I have some co-pay assistance. Since the first inpatient treatment, I haven’t been able to work.
»MORE: Read more about benefits available
Multiple Myeloma Reflections
Transitioning to not being able to work
That’s probably been the worst part for me. I thought I was who I was because of what I did. I’m a banker. I go help people, lend them money, and do all these things. Then all of a sudden, I was just sick and trying to figure out who I was.
Mentally, that’s interesting. Where I am today, oddly, is grateful. I’m thankful for all these things I’ve been through. They’ve made me a different and better person. Not totally different, but I’m a different version of myself.
I got to decide who I wanted to be post treatment. This person is a little bit different than I was before.
»MORE: Read more on how others dealt with work after a cancer diagnosis
How has cancer changed your perspective on life?
I’ve realized that somehow things just have a way of working out. I’m not sure how all the time. I have a pretty good idea, but I don’t know.
I’m not sure that all the planning and worrying I did about my health and finances was worth it.
I just say what I have to say now. I was very much a people pleaser before cancer. Now, I just don’t hold back. I wouldn’t say I’m unfiltered now.
If I love you, I’m going to tell you I love you. If that makes you uncomfortable, I don’t really care. I need to say it.
How has your wife handled everything?
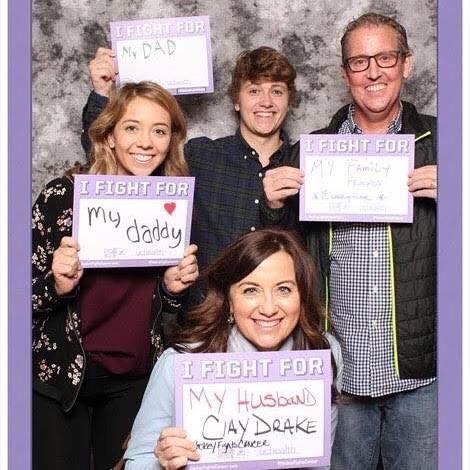
I don’t even know where to start with her. She got the diagnosis first. That was hard on her. At that point, I think she just decided to stiffen up and not let her emotions get to her. That’s what she did.
She sold the house, and we moved. She was still working, and she was traveling to Denver to see me, trying to take care of our daughter who still lived at home, and so much more.

A couple of years ago, I looked at her and said ‘I’m okay. You need to refill your tank now. You can’t make it one more second.’
What helped you both with the mental and emotional recovery?
She’s good now. We started meditating, daily walking and things like that to refill our tanks. She’s wonderful. I tried to shoo her away a few times and tell her this wasn’t what she signed up for, and she just told me I was an idiot.
If I didn’t love her before, I sure do now. I love her more than I did on the day we got married. We’ve been married for almost 28 years. I can’t say enough about her.
This whole experience was way harder on her than it was on me. As the patient, I was just doing what I was told to do. For the caregivers and family members, they’re having to watch, and there’s nothing they can do.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
How were people able to show their support?
The thing that we hated was when people would say, ‘Let me know what you need.’
To be honest, we didn’t know what we needed. If I have to spend the time to figure it out and tell you what I need, I might as well do it myself. Most people don’t know what to do.
One of the big things for us was the food. I bet we had at least one meal a week for an entire year. That was amazing. The other thing was that our closest friends came to the doctor with us.
You have to know your friends pretty well and know if they’re comfortable with it or not, but ours were and came as extra sets of ears for us.
My wife will go down the rabbit hole of research, and I begged her not to. Our friends would do research for us. They would go to appointments with us and be there to listen and ask questions. That’s clearly a level of friendship you have to know you have in order to do that, but if you do, that’s so helpful.
My friends would come and hang out with me at my house once I was back home. They would come hang out for a couple of hours. That was awesome.
At the end of the day, I think the reason I got better was because I was fighting so hard for all the people out there supporting me.
»MORE: What kind of support cancer patients say helped the most
What’s it like being a parent with cancer
My son had just gone to college. He was home on a break when I got diagnosed. We had to send him back to school after he found out his dad has cancer.
I told him, “You don’t want to be here and watch this. You’re better off being at school.” Sometimes, I’ve thought that maybe we should’ve had him come home. I don’t know, though. He’s probably struggled in ways I don’t understand.
My daughter was home with us and had other things going on in her life. I think she got tired of hearing about it. All she would hear is, “How’s your dad?”
She was just trying to do normal teenage girl things while living with someone who’s more or less a stranger. I can’t imagine it was great for her either.
When I started to feel better, it was really important for me to solidify my relationship with my kids.
I tried to be available and present. I wanted to be able to help them process things and get back to normal.
»MORE: Parents describe how they handled cancer with their kids
How do you cope with the anxiety of living with cancer?
There’s a lot of different ways I manage things. One is with Prozac. I went for a long time without taking anything. I was crying so much. You could say, “It’s such a nice day. We should go for a walk,” and I would start crying. I can’t explain how much that happened.
I finally went to my doctor and said, “I don’t know what’s happening, but all I do is cry.” They put me on a low dose of Prozac to see if that would help, and it did. I’ve been on that a few years.
Any time I travel, I have some claustrophobia. When I fly, I get anxiety. I can’t get an MRI without having to be sedated. I didn’t experience that before.
Another thing that’s helping me daily is CBD oil. I get the purest strain I can find with no THC. I take a spoonful of that a day, and that helps.
I also have started a daily meditation right when I wake up. I’d tried meditation in the past, but it wasn’t until the last few months that it’s really started to click for me.
I did an 8-week mindfulness class, and that was interesting. It keeps you aware of the moment instead of getting out into the future.
There’s no getting away from the anxiety, though. It builds and comes faster than you can even think. You have to find ways to cope.
»MORE: Read other patient experiences on yoga and meditation

What advice do you have for someone who has just been diagnosed?
Don’t be afraid to ask for help. I can’t stress that enough. I held everything in at first, and it made things worse. I should’ve just asked for help. I now volunteer and mentor another guy who has myeloma.
It’s healing to reach out and get help in a variety of ways. Whether you seek out someone who has cancer or not, it’s helpful. I try not to be the “cancer guy,” but that’s part of my story, so I don’t shy away from it.
I love sports, so my medical team has had me drop the puck at a hockey game. They’ve had me go to a college basketball game where the team captain wore my name on his jersey.
I just embrace it. It is what it is, and I’ve just accepted the support. I encourage everyone to try to do the same.

Inspired by Clay's story?
Share your story, too!
Multiple Myeloma Stories
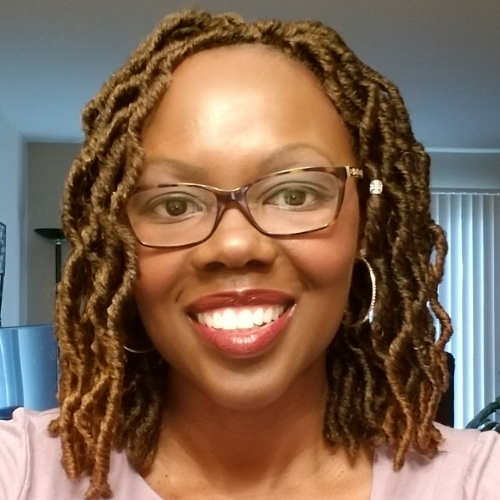
Clay D.
Diagnosis: Multiple myeloma
1st Symptoms: Persistent kidney issues, nausea
Treatment: chemo, radiation, stem cell transplant
...
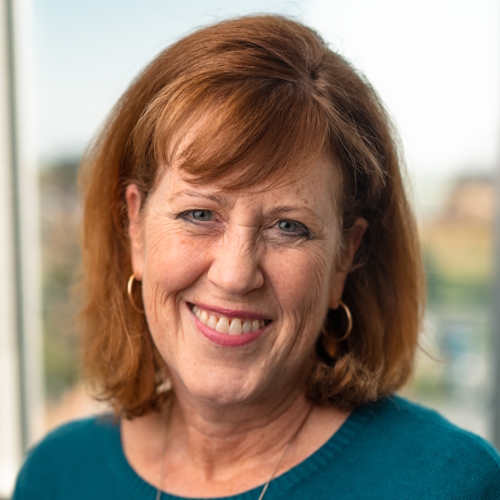
Melissa V.
Diagnosis: Multiple myeloma, stage 3
1st Symptoms: Frequent infections
Treatment: IVF treatment & Chemotherapy (RVD) for 7 rounds
...
Elise D.
Diagnosis: Multiple myeloma, refractory
1st Symptoms: Lower back pain, fractured sacrum
Treatment: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P.
Diagnosis: Multiple myeloma, stage 3
1st Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatment: Chemotherapy (Bortezomib/Velcade), Daratumumab/ Darzalex, Lenalidomide, Revlimid) and stem cell transplant
...
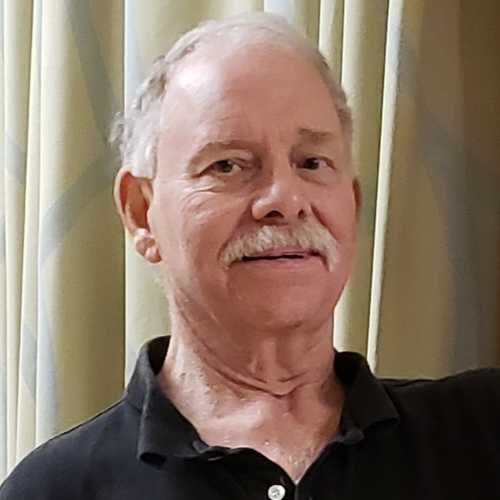
Ray H.
1st signs: Hemorrhoids, low red blood cell count
Treatment: Immunotherapy, Chemotherapy, Stem Cell Transplant
...
Valarie T.
Symptoms: Nose bleeds, fatigue, back pain
Treatment: Chemotherapy, stem cell transplant
...
Julie C.
Symptoms: Queasiness, food aversions, lack of appetite, fatigue
Treatment: Stem cell transplant, chemotherapy (D+PD), bispecific antibodies (talquetamab & cevostamab)
...
Laura E.
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
...