Dr. Michael Gieske:
The Doctor Fighting for Early Lung Cancer Screening
Story 2 of The White Ribbon Project Stories
As an avid hiker and backpacker, Mount Everest Base Camp was always on the bucket list for Dr. Michael Gieske.
“It was a nine-day trek, 9,000 feet climbing elevation and and that was really remarkable.”
The primary care physician admits there were many moments he thought about turning back.
But he wasn’t making this trek just for himself. He was making it for the many people he’s met who’ve struggled with lung cancer. Those who’ve made it and those who haven’t.
“It’s one of the things that kept me going. It was a pretty, pretty tough hike,” says Dr. Gieske.



The message Dr. Gieske wanted to shout from the mountaintops was simple:
There is so much more we can all do to save people from dying of lung cancer.
It’s a personal mission for him. He’s worked for decades down the street from where he grew up in Kentucky. His goal is to save the lives of his neighbors and community members, specifically from lung cancer, a devastating diagnosis for the thousands who get it each year.
“It was absolutely the frustration and the realization that there was a profound level of hope that lung cancer screening presented and that not only could you catch it early, but if you caught it even in the later stages, that with the new treatments we have, you can make a big difference.”
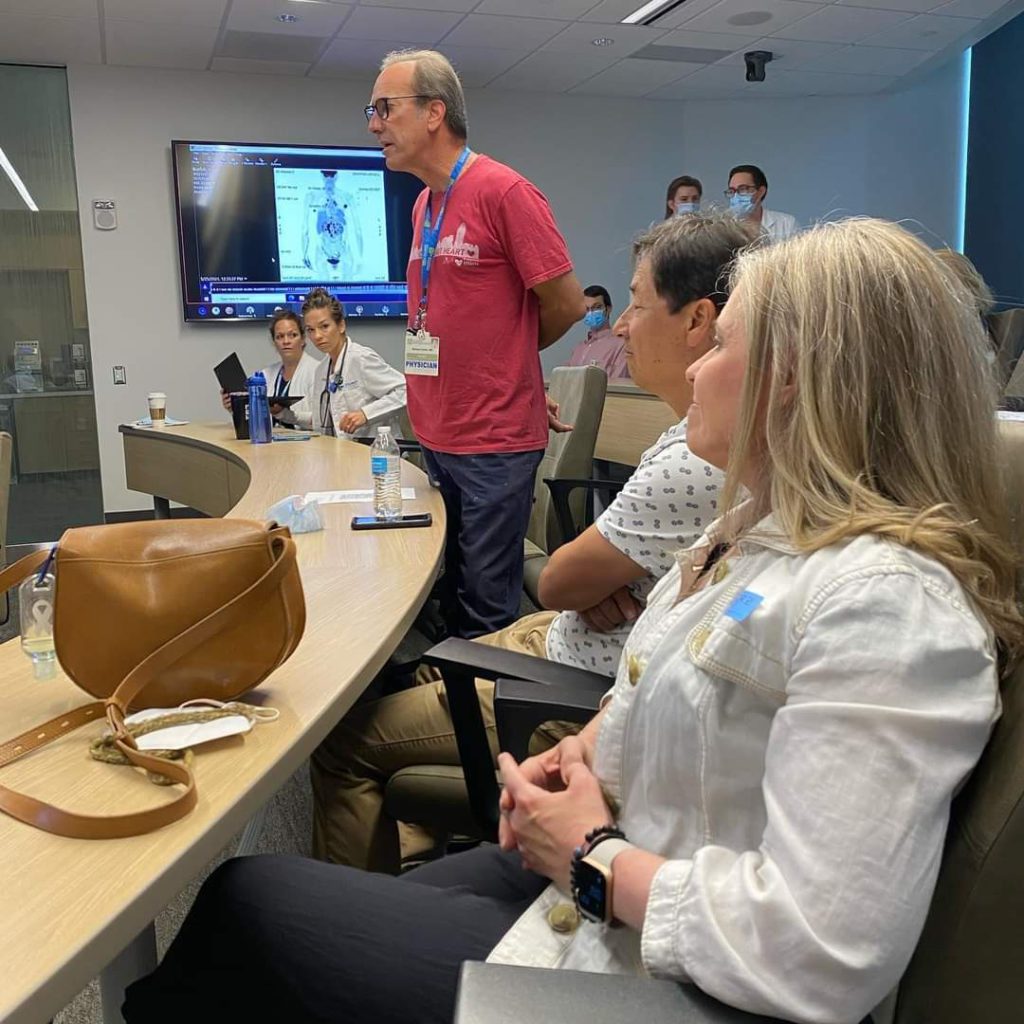
That big difference shows up at his program at St. Elizabeth’s where they’ve done 20,000 lung cancer screenings:
- 55% of lung cancer cases found are in stage 1
- 68% of lung cancer cases found are in stages 1 and 2
Dr. Gieske says the stage makes a big difference in prognosis.
“If you catch a patient stage one, you can have a greater than 90% chance of curing that patient from lung cancer. So that’s what it’s all about.”

The screenings use low-dose CT scans. According to Dr. Gieske, it’s a very low dose of radiation.
“That’s why it’s called low dose CT lung cancer screening. It’s 1.3 millisieverts, which to kind of put in perspective: natural background radiation, if you walk around over the course of a year, you absorb about 5 millisieverts. So it’s about a fifth of what you absorb just through natural background radiation. So it’s a low dose and you get very good resolution.”
He also says the procedure is a one-breath hold and is the “easiest test” they’ll undergo.
“It takes three minutes. They don’t have to have anything put it in them, up and down them, through them. You know, there’s no dye. It’s very quick and painless. They leave their clothes on. So it’s an extremely easy test to do, and it’s has an extremely impactful outcome.
“We’re finding one lung cancer for every 63 scans that we do, so 1.7 percent of the scans we do find a lung cancer, that’s a very high yield. And again, you know, when you’re finding these patients with lung cancer, the majority of them are in the early stages.”
What will hopefully help catch more early-stage cases of lung cancer are the updated screening recommendations in the U.S. this year. The U.S. Preventive Services Task Force (USPSTF) altered two guidelines:
- Expanded age criteria: 55 to 80 years old → 50 to 80 years old
- Lowered number of pack years: 30 to 20
Dr. Gieske says the move may nearly double the number of Americans whose lives could be saved by screening, from 8.5 million to 15 million.
At St. Elizabeth Healthcare, where Dr. Gieske works, he says their lung cancer screening program captures 35 to 39% of eligible patients.
But that’s much higher than the overall rate in the U.S.
“Unfortunately, right now, even if we look at the USPSTF (2013), we’re capturing about 6.5 percent of the eligible population in this country. So not a not a very good performance.”
He says the number falls very short, especially compared to the rates of screening success of other cancers.
“For example, in our system right now, we capture somewhere in the range of 70 to 80 percent of patients that are eligible for breast cancer screening and for colon cancer screening.”
Dr. Gieske blames 3 main factors for the low lung cancer screening rates:
- The screening criteria isn’t based only on age, like mammograms in breast cancer or colonoscopies for colorectal cancer.
- Perception that lung cancer = hopeless.
- The stigma and blame thrown on lung cancer patients.
On the perception of what lung cancer means, Dr. Gieske says, “Patients say, ‘Well, why even go after it? You’re going to die anyway.’ And it’s going to be a lot of education for physicians, for managers, for associates in the hospital system, for the community, for the patients to really start moving that dial from the nihilism to hope.”
Another big battle ahead in raising awareness about early screening and about lung cancer in general is the stigma attached to the cancer type.
“It’s one of the cancers that a lot of people are used to thinking that, well, they brought it upon themselves.
When you hear somebody has lung cancer, the first thought that pops into your mind is, ‘Well, you smoked, right? How much did you smoke?’
And as we know now, 15 to 20 percent of lung cancers are not from smoking. And it’s changing the stigma and changing the face of lung cancer. Anyone with lungs can get lung cancer and The White Ribbon Project has that as its tagline.
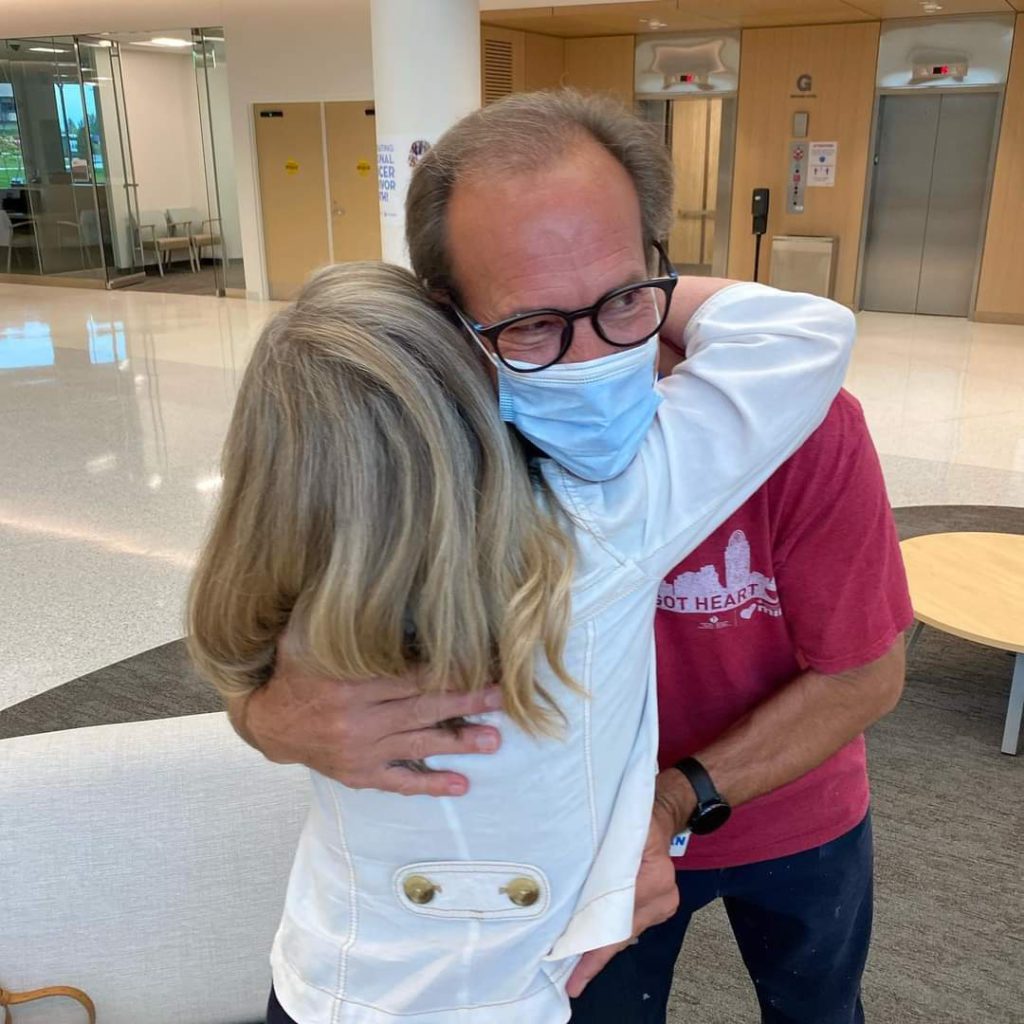
The White Ribbon Project is a grassroots campaign homegrown by lung cancer patients and caregivers, looking t o support one another.
The organization creates white wooden ribbons to signify lung cancer awareness. It’s an open invitation to anyone who wants to say lung cancer is also my story.
“One of the best things that The White Ribbon Project has done is they’ve created a community of survivors and a community of advocates that are able to simplify the terms that we use with lung cancer and lung cancer treatment,” Dr. Gieske says, adding, “To provide a high level of hope for patients that are diagnosed with lung cancer. And it’s a growing community.”

He says St. Elizabeth’s was the first cancer center that hosted the white ribbon build and through that process, built more than 128 white ribbons.
One of those ribbons made it up to Everest Base Camp with Dr. Gieske. It was the motivation he needed to keep going, despite the challenges on the trip up.
“It was just really the emotional kind of spirit and the drive of advocating for lung cancer that really helped propel me up that mountain…
I was meant to be there. It was meant to happen.”
→Back to The White Ribbon Project Stories

Inspired by Dr. Gieske's story?
Share your story, too!
More non-small cell lung cancer (NSCLC) stories
Dr. Ross Camidge, Non-Small Cell Lung Cancer, Stage 4 (Metastatic)
Symptoms: sore shoulder muscle, breathing sounded different
Laura R., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent cough, fatigue, bone pain
Treatments: Targeted therapies (tyrosine kinase inhibitors or TKIs, including through a clinical trial)
Drea C., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptoms: Swollen ankle resulting from a deep vein thrombosis or blood clot, mysterious bruising, extreme weight loss, persistent shortness of breath, rattling sound coming from the throat while breathing
Treatments: Radiation therapy, chemotherapy, targeted therapies
Lysa B., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptom: Severe but intermittent back pain
Treatments: Chemotherapy, radiation therapy, targeted therapy (including through a clinical trial), surgeries (lung resection, metastatic spine tumor surgery)
Ashley C., Non-Small Cell Lung Cancer, HER2+, Stage 4 (Metastatic)
Symptoms: Fatigue, breathlessness, persistent back pain, multiple rounds of bronchitis
Treatments: Chemotherapy, targeted therapy