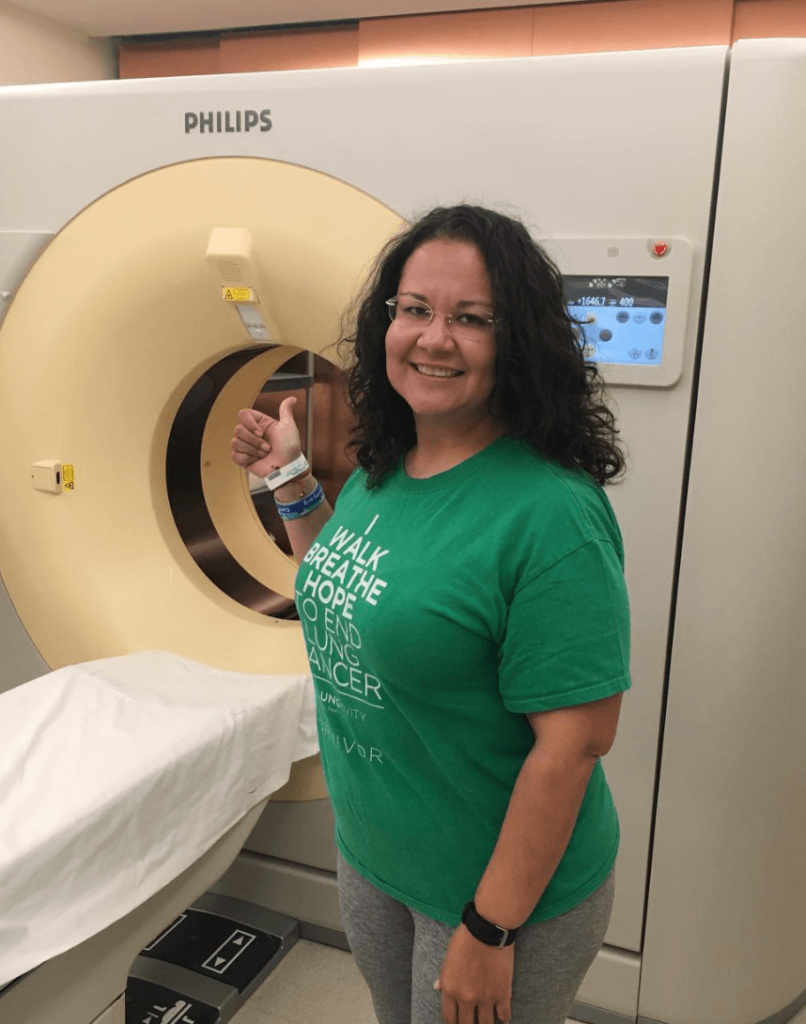
Yovana’s Stage 1B IMA Non-Small Cell Lung Cancer Story
Yovana was diagnosed with stage 1B non-small cell lung cancer (NSCLC), invasive mucinous adenocarcinoma (IMA), an extremely rare subtype. In her story, Yovana talks about surgery and recovery, being a self-advocate, and her new normal after cancer.
- Name: Yovana P.
- Diagnosis:
- Non-small cell lung cancer (NSCLC)
- Invasive mucinous adenocarcinoma (IMA)
- More on IMA from the Journal of Thoracic Disease
- Staging: 1B
- 1st Symptoms: No apparent symptoms
- Treatment:
- Surgery:
- Lobectomy of left lung
- Surgery:
Cry if you must. Feel your feelings, but know that the sun will shine again tomorrow.
Don’t take a single breath for granted. There is light at the end of the tunnel. There is hope.
Yovana P.
- Diagnosis
- Did you have any symptoms?
- What happened when they found the mass?
- What happened with the pulmonologist?
- You saw the cardiothoracic surgeon next
- What was the CT-guided biopsy like?
- How did your doctor tell you about the diagnosis?
- How did you process the diagnosis?
- How did you break the news to your loved ones?
- Surgery
- What was your treatment plan?
- Did you have to take care of anything before surgery?
- Did they have to run tests before surgery?
- Were you nervous before surgery?
- How did the surgery go?
- How was surgery recovery?
- What was your follow-up appointment like?
- Is there anything you know now that you wish you would’ve known at the beginning?
- Reflections
- How did finding a cancer community help you?
- How important was it for you to have a support system?
- Was it hard for you to ask for help?
- What was the lowest point for you mentally and emotionally?
- Can you talk about self-advocacy?
- What is your “new normal"?
- How was the financial aspect of treatment?
- What advice do you have for someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Diagnosis
Did you have any symptoms?
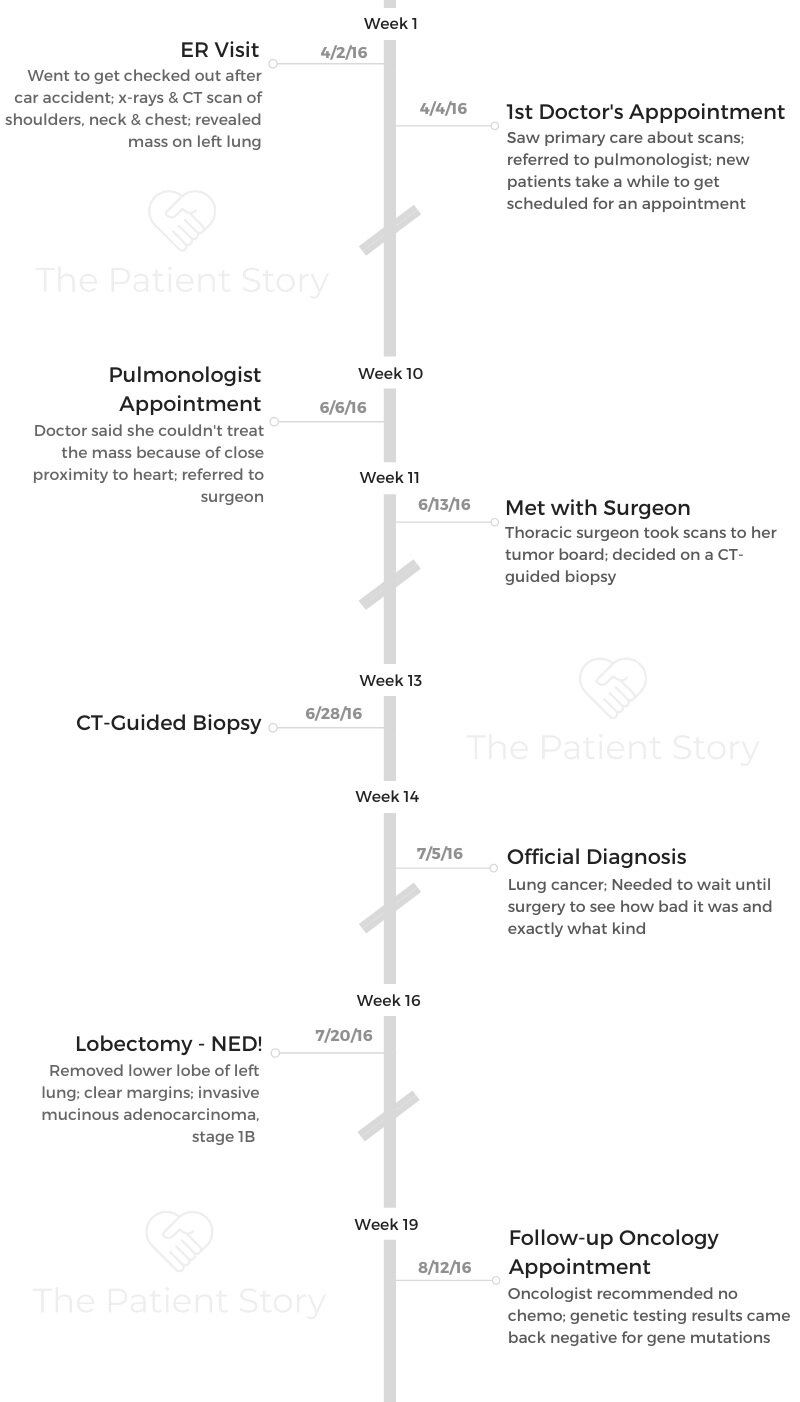
I didn’t have any symptoms. I was actually in a car accident. As a precautionary measure, I went to the ER, and they did tests and scans. That’s when the mass was discovered on my lung.
I had experienced whiplash, and I was concerned about my right shoulder and my neck. They took X-rays and CT scans, and that’s how it was found.
What happened when they found the mass?
The ER doctor recommended that I follow up with a specialist or pulmonologist. The doctor didn’t tell me much, but they said there was something suspicious on my lung that I should get checked out.
I wasn’t thinking cancer at all. I had applied to the Peace Corps the year before and had the TB skin test come back inconclusive. I had a treatment for it. I thought, “Is this related to that?” Once I touched base with my primary care, he said it wasn’t.
Since I live in Arizona, valley fever is very common. That was another direction we went in, because it might have been that. Cancer was the last thing on my mind and everyone else’s.
My doctor referred me to a pulmonologist because that wasn’t his specialty, but no one was saying, “Cancer.”
What happened with the pulmonologist?
It took me a few months to get in to see her because as a new patient, you don’t get high priority for an appointment. For a few months, I was just thinking, ‘What’s in my lung?’
Then 2 months later, I saw her. She told me that because of the location of the mass, there was nothing she could do. It was on the lower-left area area near my heart, so she referred me to a surgeon. She did request a PET scan at that time, but I didn’t realize what a PET scan was.
You saw the cardiothoracic surgeon next
A couple of weeks after that, I saw the surgeon, and she confirmed that the scan showed activity. Again, I didn’t realize what that meant.
She took everything to her tumor board and see what they recommended. When she came back from that, she said they recommended that I have a CT-guided biopsy just to check it out.
I wasn’t living in the city at the moment, so I would make the 2-hour commute to the Phoenix area. I had to be there super early in the morning.
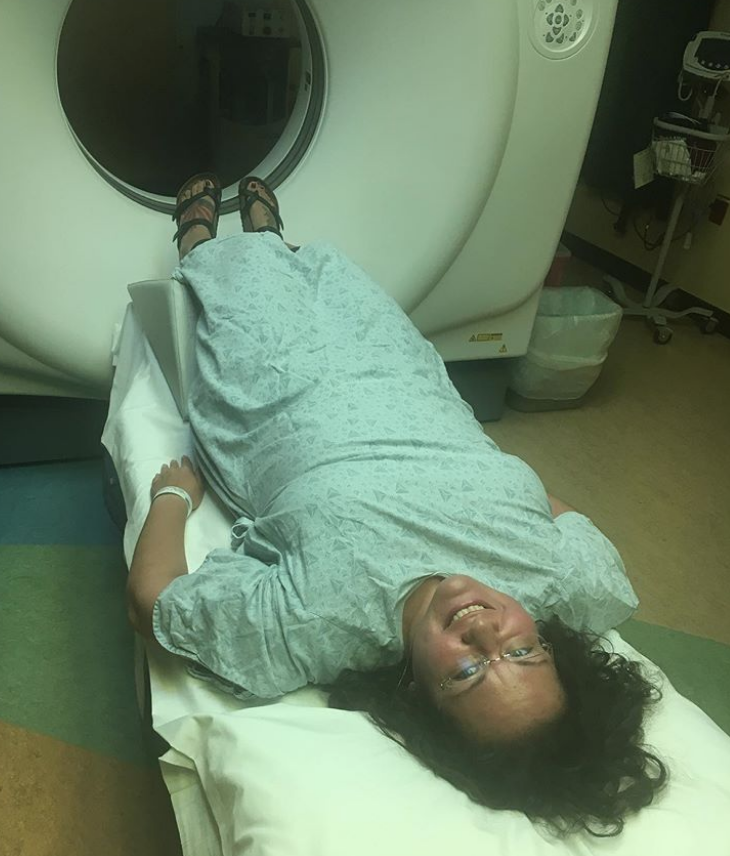
What was the CT-guided biopsy like?
They put me in sort of a twilight zone. I wasn’t out, but I wasn’t alert. They got a few good samples.
I had to wait in the hospital for a few hours, and then they recommended that I not drive back home.
They didn’t want to chance the change in elevation collapsing my lung while I was driving back north, so I stayed in town another night as a precautionary measure.
This was the week before the 4th of July. The holiday happened, and then I got my results.
How did your doctor tell you about the diagnosis?
I wasn’t living in town, so my doctor called me. She said, “We found the last thing we thought we would find, which is cancerous cells.”
I heard that, and I thought, “Oh, I have cancerous cells. No biggie.” I messaged my sister and told her, and my sister asked if I was okay. I was like, “Yeah, why would I not be?”
She said, “You do know what that means, right?”
How did you process the diagnosis?
I think I experienced a moment of denial. I thought, ‘She didn’t come out and say I had cancer. She said I have cancerous cells.’ It took me a while to process.
I had a follow-up appointment the next week, and I got a pamphlet that said ‘lung cancer.’
That’s when I really knew.
It took me a while to put everything together because I thought the only way you could get lung cancer was if you smoked. I had never smoked, and it didn’t make sense to me at all.
How did you break the news to your loved ones?
I had a family text thread going on. I was keeping them updated. Once it was confirmed, I sent a text to that thread. It consisted of siblings, cousins, aunts and uncles, and everyone.
Everyone was in shock because of the stigma around lung cancer, but everybody was very supportive.
»More: Breaking the news of a cancer diagnosis

Surgery
What was your treatment plan?
At the follow-up appointment, she gave me some options. She said she didn’t know how bad it was and said she wouldn’t know until they got in there.
She recommended surgery. I had been re-invited to the Peace Corps, and I was supposed to leave in December.
I was asking her how this was going to affect my volunteering. I’m a planner, and I had not planned for lung cancer. I was wanting to see how I could get around it.
My surgeon said, “We don’t know. We’ll find out when we do the surgery, but I don’t see how this would change anything.”
She explained the process and my recovery time. I asked her how long I had to think about it because I like to process things. She told me to take a week or 2 and even get a second opinion if I wanted one.
The moment she suggested I get a second opinion, I was like, ‘No, let’s do it. Let’s get it done.’
She was so open, and that just made me feel so comfortable. She sold me on her plan.
Did you have to take care of anything before surgery?
I contacted my HR department and told them what was going on. I told them not to worry and that I would be gone for about 2 weeks. They were like, “That’s a big diagnosis. Don’t worry about it.”
I ended up moving back into the Phoenix area at my sister’s house. In a matter of about 10 days, I had moved back into town, situated myself into my sister’s house, and notified my work.
Did they have to run tests before surgery?
The day before surgery, I went in for some tests. They drew blood and stuff like that. At that point, I signed a release.
Somebody came and asked if I would be open to my tumor being taken to a lab so they could do research on it, which of course I agreed to.

Were you nervous before surgery?
I was a little bit scared because everything was unknown. Everything had been so new to me. There was definitely some nervousness about what the outcome was going to be.
I was more nervous of what they were going to find and how bad it would be than the surgery itself.
How did the surgery go?
It went well. It was completely successful. Before the surgery, the surgeon had asked me if I wanted a port put in just in case I needed chemotherapy.
She said it would be easier to go ahead and place it then rather than waiting. My aunt was with me and suggested that I should do it, so I did.
After I woke up, I saw my surgeon, and she said, “It looks like we got it all.” They didn’t have to put a port in.
They got clear margins. They removed the lower lobe of my left lung, but they got it all. I was very happy with that news.
How was surgery recovery?
I was in the hospital a few days. The worst pain I’ve ever experienced was having them pull the chest tube out. I’d like to think I have a pretty high pain tolerance, but that was horrible.
I got discharged and went to my sister’s house. Life was very different. I couldn’t find a comfortable sleeping position. I had never had that issue before. Walking around the house and the neighborhood was very challenging and tiring.
I don’t know what I was thinking. I had never had a major surgery before, so I guess I didn’t know to expect recovery to be hard.
It would take me an hour or more to walk a mile. It depressed me a bit. I ran 2 half-marathons before my surgery, so once it hit me mentally, it was hard. I was trying to get to December. I had been notifying the Peace Corps of my progress.
What was your follow-up appointment like?
At my first follow-up, my surgeon said she still wanted to refer me to an oncologist just in case he recommended chemotherapy or radiation. She told me I’d have to be under observation for the next 5 years.
If the oncologist didn’t feel like he needed to take me on as a patient, she said she would take care of my follow-up appointments. I did become a patient of the oncologist, though.
I told him about my plan for December as well, and he said, “As long as we can get a CT scan at the year mark, it’ll be fine.”
He said I fell into a gray area. People who are diagnosed as 1A don’t get chemo or radiation. People who are diagnosed as 2A do. I was 1B, so I had a choice.
He said that with my age and overall health, he felt like the side effects of treatment would be more harmful than beneficial in my specific situation. I appreciated that honesty.
Is there anything you know now that you wish you would’ve known at the beginning?
When I tell people I had lung cancer, they say, ‘You don’t look like a smoker.’
I tell them I’m not, and it doesn’t matter. If you have lungs, you can get it. Everyone just kind of equates lung cancer with smoking.
I wish that I had known that lung cancer can happen to anyone. I think I would’ve been proactive about things I was feeling that I may have ignored.
In retrospect, I’m like, “I did have this symptom, and maybe it was related.” Since lung cancer was the last thing on my radar, I disregarded things.
I had a tonsillectomy a year before all this. Ever since that, in the mornings, I would spit up bloody phlegm. My doctor from that said it was a side effect from the tonsillectomy.
After my diagnosis, my tumor was labeled a mucinous adenocarcinoma. After my lung surgery, I’ve never had the bloody phlegm. Had I not equated lung cancer with smoking only, maybe I would’ve looked into it.
Also, for years before all this, I had pain in the exact spot they went in to take the biopsy. I always thought I pulled something. I never thought much about it. I don’t know if it was related, but I wish I would’ve known to speak up about it.
Thankfully, I got into a car accident and found it early by chance. That’s one of the things you think about after the fact. Hindsight is 20/20 when it comes to first symptoms. Your body talks to you, and most of the time, you think it’s not a big deal. I wish I would’ve been more aware.

Reflections
How did finding a cancer community help you?
After spending 2 weeks at home recovering, I realized I wasn’t in a good place mentally.
I ended up looking for a lung cancer support group. My family and friends were great, but I needed to talk to people who understood.
I showed up for a newcomer meeting. Finding the group helped me tremendously.
I saw that they offered yoga. I had been practicing yoga for several years, and it had become a big part of my life.
Then 3 weeks after surgery, I showed up to the gentle yoga class, and it made me feel a bit more normal.
After one of the classes, I introduced myself to the instructor. She would come check on me after class each time and ask how I was doing. I would get disappointed in myself because I was struggling.
She was so supportive. She was like, “Honey, you just had lung surgery. Be kind to yourself and let yourself heal.” That helped me get back to a new normal.
How important was it for you to have a support system?
It was extremely important. They were so helpful. I come from a Hispanic background, and we are a close-knit family. That’s how my mom raised us.
Just to have that and know that I could rely on them meant everything to me. I don’t know how I would’ve been able to cope with it otherwise.
My sister is one of my best friends and closest confidants, so that was amazing. Roles reversed for us a bit because I’m the older sister. She kind of became like a mom to me during recovery, and she still acts that way.
Was it hard for you to ask for help?
It was hard because I was very independent. I’m used to doing everything for myself by myself. I didn’t rely on anyone. I told my sister I was going to be moving back into town and ending my relationship, and I said, “Can I just stay here for a week or 2 until I find a place?”
She said, ‘We have the space. Yes, you can stay here, but you don’t need to leave. Come stay here, and let’s figure everything out.’

That meant a lot to me that she was so open. She made me feel like her home was my home. I still get emotional about it because it was just so special to me.
What was the lowest point for you mentally and emotionally?
The lowest point came 2 weeks after surgery when I was recovering. I was recovering from surgery, but I was also going through a breakup.
When I was diagnosed, the person did not take the diagnosis as well as I had hoped for.
Cancer can be difficult for people because there are so many unknowns, so before surgery, I ended the relationship.
Recovering from surgery and dealing with that was a double whammy. It was difficult in every way. That’s when I sought support outside my family.
Can you talk about self-advocacy?
Other than pushing for still being able to go to the Peace Corps, I was mostly just letting everything soak in. I was coming across all these new terms I didn’t know, and I would write them down and research them.
Once I started going to lung cancer support groups, I realized that we become our own advocates. Then I’d have questions for my doctor at my next appointment.
I gained a sense of empowerment, and I needed to make sure I was taking care of my body.
When you’re first diagnosed, the terms are new, the feelings are new, and everything is new. Find people who have gone through what you’ve gone through, and they’ll be able to help guide you. They might not have all the answers, but it helps tremendously.
»More: Self-advocacy as a patient
What is your “new normal”?
I’m back at work full time. I have a very active social life. I’ve been able to resume the activities I enjoyed beforehand, which are hiking, yoga, and running.
My new normal is that I do have to be kind to my body and know my limits. I know I can’t do that yoga pose I could do 5 years ago, and that’s okay. I can keep on working, and maybe I’ll be able to do. If not, it’s okay. There are other poses.
It’s about realizing that I’m not where I was before, but I’m still able to do so much. My new normal also includes a lot of advocacy because I was so in the dark at the time I was diagnosed. It can affect anyone.
How was the financial aspect of treatment?
I applied for FMLA, and I was approved. I was out of work for about 9 weeks. When I did resume working, I came back slowly. My sleep had been altered, so I was tired a lot. I worked for 4 hours a day the first week, increased to 6 hours, and then went back to full time.
My job was great. My supervisor and coworkers were awesome. I was getting messages and cards. Knowing that’s what I was going to go back to when I went back to work was nice.
My insurance was great. I didn’t realize how good they were until I needed them. That was great. I had been at my job at that point for a little over 9 years without really needing my insurance.

What advice do you have for someone who has just been diagnosed?
Do not go to Google. Google told me there was a 5-year survival rate. I cried. I was like, “I’m not even going to make it to 40.” To read outdated information online was not something I would recommend.
Seek out support groups and other individuals who can mentor you. Be comfortable with your medical team. If you’re not, go get that second opinion. If you feel like you can’t voice your concerns, maybe that’s not the right fit for you.
There’s a lot of research going on. If you’re newly diagnosed, have genetic testing done because there are so many targeted therapies that are available.
Cry if you must. Feel your feelings, but know that the sun will shine again tomorrow. Don’t take a single breath for granted. There is light at the end of the tunnel. There is hope.

Inspired by Yovana's story?
Share your story, too!
Lung Cancer (Non-Small Cell) Stories
Yovana P., Non-Small Cell, Invasive Mucinous Adenocarcinoma (IMA), Stage 1B
Cancer details: Had no genetic mutations; IMAs comprise between 2-10% of all lung tumors
1st Symptoms: No apparent symptoms
Treatment: Lobectomy of the left lung
Dave B., Non-Small Cell, Neuroendocrine Tumor, Stage 1B
Cancer details: Neuroendocrine tumor
1st Symptoms: 2 bouts of severe pneumonia despite full health
Treatment: Lobectomy (surgery to remove lobe of lung)
Terri C., Non-Small Cell, KRAS+, Stage 3A
Cancer details: KRAS-positive, 3 recurrences → NED
1st Symptoms: Respiratory problems
Treatment: Chemo (Cisplatin & Alimta), surgery (lobectomy), chemo, microwave ablation, 15 rounds of SBRT radiation (twice)
Heidi N., Non-Small Cell, Stage 3A
Cancer details: Non-small cell lung cancer (NSCLC)
1st Symptoms: None, unrelated chest CT scan revealed lung mass & enlarged mediastinal lymph nodes
Treatment: Chemoradiation
Tara S., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Numbness in face, left arm and leg
Treatment: Targeted radiation, targeted therapy (Alectinib)
Lisa G., Non-Small Cell, ROS1+, Stage 4 (Metastatic)
Cancer Details: ROS1+ tends to be aggressive. It can spread to the brain and to the bones.
1st Symptoms: Persistent cough (months), coughing a little blood, high fever, night sweats
Treatment: Chemo (4 cycles), maintenance chemo (4 cycles)
Stephen H., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Shortness of breath, jabbing pain while talking, wheezing at night
Treatment: Targeted therapy (alectinib), stereotactic body radiation therapy (SBRT)
Ivy E., Non-Small Cell, EGFR+, Stage 4 (Metastatic)
Cancer details: EFGR-positive
1st Symptoms: Pain & stiffness in neck, pain in elbow
Treatment: Two targeted therapies (afatinib & osimertinib), lobectomy (surgery to remove lobe of lung)
Ashley R., Non-Small Cell, EGFR+ T790M, Stage 4
Diagnosis: Stage IV Non-Small Cell Lung Cancer
1st Symptoms: Tiny nodules in lungs
Treatment: Tagrisso (Osimertinib)
Shyreece P., Non-Small Cell, ALK+, Stage 4
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Heaviness in arms, wheezing, fatigue
Treatment: IV chemo (carboplatin/pemetrexed/bevacizumab), targeted therapy (crizotinib, alectinib)
Amy G., Non-Small Cell Squamous, MET, Stage 4
1st symptoms: Lump in neck, fatigued
Treatment: Pembrolizumab (Keytruda), SBRT, cryoablation, Crizotinib (Xalkori)
Dan W., Non-Small Cell, ALK+, Stage 4
1st Symptoms: Cold-like symptoms, shortness of breath, chest pains
Treatment: Radiation, targeted therapy (Alectinib)
Tiffany J., Non-Small Cell Adenocarcinoma
1st Symptoms: Pain in right side, breathlessness
Treatment: Clinical trial of Tagrisso and Cyramza