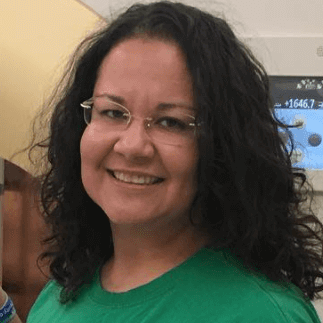
Tara’s Stage 4 ALK+ Metastatic Non-Small Cell Lung Cancer Story
When she felt numbness in her face, arm, and leg, Tara Sanderson realized something was wrong. She describes what it was like to go through radiation and targeted therapy, the stigma of lung cancer, how she approached fertility preservation, and finding a cancer community.

- Name: Tara S.
- Diagnosis:
- Non-small cell lung cancer (NSCLC)
- ALK+
- Staging: 4, Metastatic
- 1st Symptoms:
- Numbness in face
- Eventually in left arm and leg
- Treatment:
- Radiation therapy:
- Targeted at brain stem, 14 treatments
- Targeted Therapy:
- Alectinib, pill taken daily
- Radiation therapy:
Everybody who gets cancer eventually looks up their cancer on the internet, even though they tell you not to. Don’t go off of what you read. Everything you’ll read is terrible and sounds like you’re going to die tomorrow.
Regardless of what you’re dealing with, realize that your mindset about it is going to make the biggest difference. If I gave up, things would be so much.
Tara S.

- Diagnosis
- Treatment
- Fertility
- Support
- Reflections
- What’s hardest for you mentally and emotionally?
- How do you keep your worry at bay?
- Can you talk about the stigma around lung cancer?
- Can you talk about self-advocacy?
- How has the whole experience affected the relationship with your husband?
- What advice do you have for other married couples?
- How is the financial aspect of treatment?
- What is your “new normal”?
- What is it like living with an invisible illness?
- What advice do you have for someone who’s just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
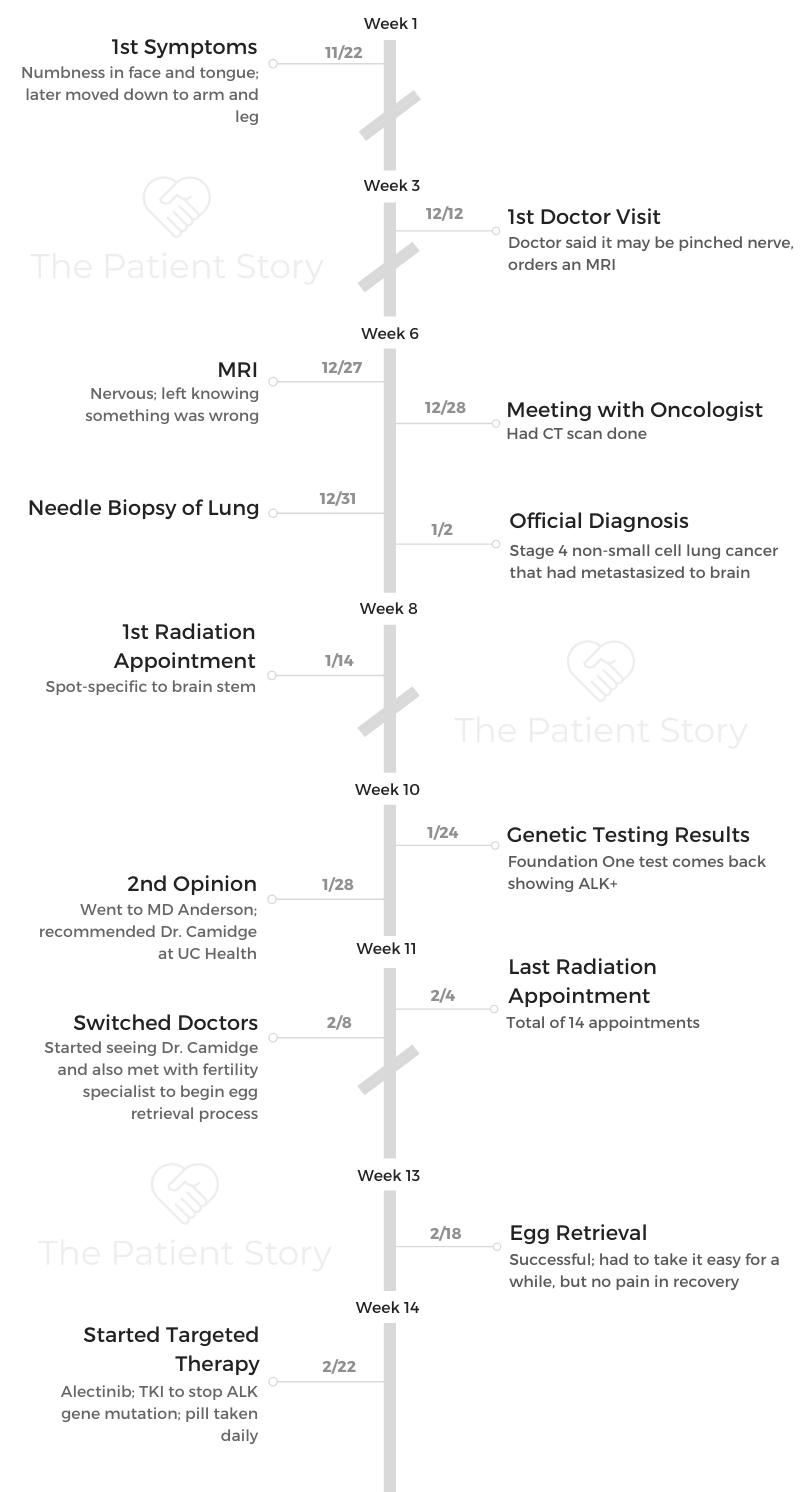
It started on Thanksgiving of 2018. I felt some numbing in my face on the side and into my tongue.
I thought I was having a reaction to something I ate because I normally follow a pretty rigid diet. It was Thanksgiving, and I was eating whatever I wanted, so I just thought my body didn’t like whatever I ate.
I didn’t think too much of it, but it continued on. I couldn’t make sense of it. I was trying to think of what it could be. I had recently gotten an IUD, and I thought it might be because of that. I was hardcore researching IUD side effects.
Then I got vertigo. I had lightheadedness. I got the IUD removed eventually, and that didn’t change anything.
That’s when I went to my primary care physician. She said it could be a pinched nerve. She said, “Worst case, it’s MS.” She wanted to get me scheduled for an MRI and go from there.

What happened after the first visit with your primary care?
It was the day after Christmas, and we were scheduled to leave on a trip to New Mexico to see my husband’s family. The numbing went into my left arm and into my leg that day.
That was it for me. It freaked me out, and I knew I had to stop being stubborn, so I went on December 27th for an MRI.
I went to a local hospital that was down the street from us. I knew something was up when I was in there for the scan because the technician was asking me all sorts of questions. I just felt like it was a red flag. I walked away knowing it was serious.
Later that day, we got a phone call from my primary care’s office. It was from the person who was on call for her. The poor guy was freaking out. He was not calm at all. He was like, “There are these spots.”
He didn’t say cancer yet because I hadn’t done a biopsy. He told me the sizes. I had one that was 2 centimeters on my brain stem. Another one was smaller and in my frontal lobe.
He said I needed to get in for a CT scan as soon as possible. I got that done the next day. That’s when they found the spot on my lung. They set me up with an oncologist that day as well.
When did you get the official diagnosis?
They were avoiding the word ‘cancer’ for some reason, even though I knew that was what we were dealing with. Nobody wanted to say it.
On December 31st, they went into my lung for a needle biopsy. We got the results back on January 2nd, and that’s when they officially diagnosed me.
My oncologist had steered me in that direction, but he hadn’t said for sure it was cancer and that it had metastasized to my brain until we got the biopsy results back.
How were you feeling throughout the diagnosis process?
The biggest shock of a day for me was when I got the call about my MRI results. Even though I knew it was bad when I was leaving my MRI, it was still so hard to hear.
That’s when I had my breakdown moment and cried with my husband.
After that, I pretty much just knew that I was dealing with cancer. I went into attack mode. I felt like, “I’m just going to handle this.” I had prepared myself for the official diagnosis.
I didn’t know that I was dealing with stage 4 at the time, but I pretty much knew that I had cancer after the MRI. I wasn’t surprised when they told me.
After all the results came back, we had a big talk with my oncologist. That’s when the doom and gloom set in. I asked if it was terminal, and he said, “People live for maybe 2 years. That’s a good timeframe.”
He was not very encouraging, so I’m not with that oncologist anymore. I really struggled with my doctor after that, and I switched later on.
Treatment
You started radiation right away
The spot on my brain stem was causing me so many issues, so they wanted to get me into treatment as soon as possible.
They sent my biopsy results off to see if I had any gene mutations or anything like that, and in the meantime I started radiation.
I had a rather aggressive plan. I got a total of 14 treatments of spot-specific radiation to my brain stem. I would go every weekday for about 15-minute sessions.
Did you experience side effects from radiation?
Radiation itself wasn’t terrible. They do the mask and strap you down to the table, which is kind of freaky.
At first, it was fine. I didn’t really feel much. I was just tired. A few times later, I was throwing up. I was beyond weak. I couldn’t eat. Things started tasting very metallic.
Coffee was the most disgusting thing. Certain smells would get to me. I would open our fridge and want to vomit because of all the smells that would come out. Our trash can would make me nauseous, too.
They told me that hair loss was possible. I noticed I was losing more than normal, but it wasn’t until I put my hair up and saw spots that I realized I was actually losing it.
I was questioning it, though, and thinking, “Well, was my hairline always like that?” It started growing back in, though, and it started growing back in curly, so I know I lost quite a bit. That’s been pretty annoying.
»MORE: Read other patient experiences with radiation therapy

You got a second opinion
Near the end of my radiation treatment, my husband and I made a trip to MD Anderson and got my second opinion. They told me I was on the right path as far as what I’d been told.
By that time, I had gotten my genetic testing results back and found out I had an ALK gene mutation.
The only new direction they gave me was the leading doctor for that is actually in Denver at UC Health Aurora campus. They told me I needed to be seeing him. They confirmed that I might want to switch doctors to Dr. D. Ross Camidge, a thoracic oncologist.
Issue of fertility post-treatment
Another thing they brought up to me was fertility, and no one had brought that up to me before. They told me I was always going to be on medication since it was a gene mutation.
They said I wouldn’t be able to carry my own children because of that and might want to look into fertility options.
»More: Patients talk about fertility preservation
What pushed you to switch oncologists?
I finished my radiation treatments where I was, and I immediately met with Dr. Camidge and a fertility doctor. I loved Dr. Camidge. He had a completely different mindset than my first oncologist.
He was so positive and said people are living 10-plus years with this, and there’s new research being done. He had a level of hope I wanted from a doctor.
He made me feel like my cancer was kind of like someone who had diabetes. I just needed to take my medication and manage it.
That was so refreshing after being with a doctor who was like, ‘Yeah you have about 2 years to live.’
»More: How to be a self-advocate as a patient
What is the plan with the alectinib?
Outside of the radiation I finished, this is my treatment plan for now. I take it daily. It’s a pill. That’s what’s keeping the gene mutation from forming in my body and continuing to progress. Everybody’s body responds differently.
Over time, our cancers learn to adapt to the medication.
That’s why some people can last years and years, and some people can only take it for a month. It just depends. At this point, the medication has helped shrink the circumference of my tumors a little bit, but I still have them all.
They’re under control, and they’re inactive. I’ve had PET scans periodically showing that they’re inactive. We’re just kind of monitoring at this point and seeing how long they can stay that way. Once they become active again, we’ll have to decide what to do next.
Right now, alectinib is working. They want to just let it work until it won’t work anymore, but then I still have options. Dr. Camidge has said that at that time, his plan will be going into my lung with radiation and treating that. I don’t think he wants to get ahead of it. He wants to still have options once it starts being active again.
How often are you getting scans now?
I’m going in for scans every 3 months. At the beginning, I had every scan possible and had them more frequently.
Dr. Camidge wants to eventually get it to every 5 months, but it’s hard for me.
3 months is a struggle already because I know I could stop responding tomorrow, and I have 2 more months until my next scan.
I don’t want something to be developing and not know. That’s really hard for me mentally.
»MORE: Hear from a lung cancer oncologist, Dr. D. Ross Camidge

What was the hardest part of treatment?
Everything in that first month. There was just so much going on, and that’s what made it hard. There wasn’t one thing. It was all back to back and led to pure exhaustion. When I was going through it, I had to just get through it.
I had the mentality that I was just going to do whatever it takes. It wasn’t until a few months afterwards that I realized how hard everything was.
Fertility
Did you go through with fertility treatment?
Dr. Camidge was very encouraging. He told me I should do the fertility path if I potentially wanted to have kids.
He said, “Even if you don’t decide to use the eggs that you freeze, it’s just a good option to have.”
At that point, I knew I was going to have to get on a TKI, which is an inhibitor to stop that gene mutation from forming. He told me that once I was on that, if I got pregnant, it would result in a miscarriage.
Before we started that, I went through the whole process of freezing my eggs. I went from taking steroids and going through radiation to taking all these other pills.
I was so out of whack. My body was freaking out. The fertility treatment was about a 2-week process, and right after that I started alectinib, which is a TKI for an ALK mutation.
»MORE: Fertility preservation and cancer treatment
What was the fertility treatment like?
That was actually one of the hardest things I went through, just because my body was so weak and drained at that point. Having to take shots 3 times a day, having my hormones out of whack, and all that. At the end of the 2 weeks, they gave me a trigger shot and actually went in to retrieve the eggs.
The surgery was an outpatient procedure. That was the easiest part of the whole process. You’re knocked out, so it makes it easy.
I was at a high risk for a few things because I had so many eggs at that point. They took precautions, but nothing wound up happening, and I was fine. I just couldn’t work out or be very active for a while afterwards, but other than that it went well.
Now, they’re frozen and waiting. It’s hard because if I ever want to do anything with that, it’s an expensive process. I don’t know what we’ll do, but it’s a nice option to have.
»MORE: Read a patient’s detailed IVF journal
How was the emotional aspect of fertility treatment?
I’ve always looked forward to being a mom. I was a nanny for a long time. I was a teacher before I got diagnosed. I’ve always loved kids, so to be told that I couldn’t have my own was a really hard thing to hear.
It helped knowing that while I might not be able to carry my own child, I might be able to have my own. Regardless, I don’t know if I’m going to go that route. We might adopt. I don’t know what my husband and I will do.
At least there’s a little bit of hope that I might still be able to have that biological child, though. I’m really glad I did the fertility treatment. It eases my mind.
I wish I could carry my own child, but for whatever reason, that’s not what God wants for me. I might not be able to make sense of it now, but I will later.

Support
It can be hard to ask for help. How did you handle that?
I’m very stubborn and try to do things myself. I look back and think of certain moments, where I’m like, “Oh, wow. I really should’ve asked for help.” What caused me to ask for the help I did ask for was just needing it so bad. I had to grin and bear it and ask.
I woke up for one of my radiation treatments, and I was so sick. I was going to drive myself, and I just knew that I couldn’t do it, so I had to call and ask for help.
People are really so grateful when you do ask for help, because they want to help. They don’t know what they can do, so when you ask for help, it’s a blessing for them to be able to help you. I had to view it that way, but it took me a while to get there.
How important is it to have a support system?
Outside of my aunt, mother figure, and my husband, I had my school community. I was a high school teacher before I got diagnosed, and they were all so supportive. They were sending cards, buying me dinner, and loving on us.
Having all these levels of support really help you push through it when you’re feeling drained. Allowing people to be there for you and support you is so refreshing.
It brings some life that you’re missing. It gives you a boost.
What were some specific ways people helped you?
The one that sticks out the most is something a woman at my work who I’m friends with did for us. She got a chain of people to cook us food for more than a month. Every week we had 2 meals waiting for us on our doorstep.
It was one of those things I didn’t even have to ask for. She just went and did it, no questions asked.
It really opened my eyes to how I want to respond when someone I know is sick. I want to just take action and help instead of putting the pressure on the sick person and being like, ‘Let me know what I can do.’

Did you get involved with a cancer community?
At the beginning, I didn’t talk to anyone. Later, Dr. Camidge told me there was a Facebook group for people with ALK mutations. My husband had actually already found it, but I didn’t want to join. I had to come to it on my own terms.
In the group, there was a woman in our area who is big in the lung cancer community. She reached out, and I got to meet with her. Since then, I went to her fundraiser event and got to meet more people with our cancer.
She’s brought me in to another Facebook page that’s just people with my cancer in Colorado. They do meetups as well.
I’m slowly getting connected, but I have to go at my own pace.
If I go onto that group every day, there can be a lot of bad news. If I get into it too much, it can get me in a negative mindset. At the same time, it’s so nice to talk to people with my same type of cancer.
I just have to walk a fine line and find the balance for me. I don’t think there’s a wrong way to do it. It’s just about what finding works for you.
»MORE: Join other patients and caregivers on The Patient Story Instagram

Reflections
What’s hardest for you mentally and emotionally?
With my cancer, I can stop responding at any time. I feel normal for the most part, but it’s hard carrying around that weight of not knowing what comes next when I stop responding to the medication.
I don’t know what treatment plan I’m gonna have to be on. Are they going to develop something before then that I can go on instead, or am I going to have to do chemo?
It’s hard to struggle with the unknown.
How do you keep your worry at bay?
I’m really into journaling. I see a therapist, which I highly recommend. Even if you’re not going through cancer, I think everyone should see a therapist.
I’m really into my Christian faith. I do devotionals and try to stay strong there because that helps me a lot. I try to keep my mind right. I can’t change this situation, so I just have to make the best of it.
It’s not going to do me any good to be negative and unhappy about it, because that won’t change anything.
Can you talk about the stigma around lung cancer?
I get insecure about it, so I nip it in the bud. When I tell people, I’m like, “I have lung cancer, but I’ve never smoked before.” I know that’s what’s going through their minds, and I don’t want to have that stigma attached to me.
That’s what I thought prior to having lung cancer, honestly. I always correlated a diagnosis with smoking. I never knew there was another side to lung cancer.
I’ve noticed that I always preface my diagnosis with that because of my own insecurity about it.
I wish people knew more about it, but I’m glad I can then explain the other side of lung cancer that people may not know about.
Can you talk about self-advocacy?
Having cancer forces you to be an advocate. Every time we went into the doctor’s office, we had a list of questions. I would email questions I had if I needed the answer right away. I changed my doctor because I wasn’t happy with my first one.
If I’m going to bug you, sorry, but I’m new to this. If I sound stupid, sorry, cancer is new to me, and I have questions. My doctor now is really good about answering my questions.
»More: Self-advocacy as a patient

How has the whole experience affected the relationship with your husband?
We got married in September of 2018. When I got diagnosed, we had only been married a few months. It’s basically been a year of cancer for us.
It’s brought us closer, if anything. It’s challenged us in ways that most couples never have to deal with.
I’ve learned to rely on him in ways that I never had to. I really appreciate him. He’s been there for me at all my appointments and everything.
It’s helped us appreciate each other and appreciate life more. Thankfully, he’s had a really good mindset, too, which has really helped me.

What advice do you have for other married couples?
Stay close. Don’t let it divide you and cause arguments. It adds so much stress to your life, but you just need each other so much in that time. Be aware of what your partner needs. There were times he needed to get involved and talk to people in the cancer community, and I wasn’t ready yet.
Understand that what you need and what the other person needs isn’t always going to be the same thing at the same time, and learn how to navigate and respect that.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
How is the financial aspect of treatment?
Overall, we’ve been really blessed. I had good health insurance through my job when I was diagnosed, so that helped initially. To get my eggs frozen, it was $10,000. We didn’t just have that kind of money lying around, but we have amazing people in our life.
The woman who’s like a mother to me and her husband put up the money for us to get it done. They said, “Here’s money for the medical bills.” Without her even knowing, it was the amount we needed for the fertility treatment.
Outside of that, we’ve had people offer to start a GoFundMe. Our insurance is really good, though. The only thing I’m worried about now is the surrogate process if we decide to go that route later.
It’s like $90,000 on the low end. I don’t know if I’ll be able to use those eggs, but we’ll see. Who knows what will happen between now and then?
As far as the stuff that’s keeping me alive, everything has just been working out really well. The medication I’m on is really expensive, but there’s a program that you can go through to get coverage on it. That’s been taking care of the cost of that. My original oncologist’s office set me up with the program.
If you’re wanting to get into a financial program and don’t know how, ask your nurses. They want to help you.


What is your “new normal”?
As far as my husband and I, he has dreams. He has a side business and wants to quit his regular job. We have certain areas we’d like to go or live in. He’s being more proactive in that area, and I’m doing the same. I’m not wasting time at a job I don’t love. I’m trying to figure out what’s next for me.
Some days I wake up great, and other days I’m a wreck. It doesn’t really ever feel normal, but I just keep going. I still feel uncomfortable with the fact that I have cancer. It has made me appreciate things more, and I’ve learned to adjust.
Feeling uncomfortable is partially about the type of cancer I have because it’s lung cancer. I always want to preface it. I look young, and I don’t fit the bill of cancer. I’ve gone into MD Anderson, and I’m the youngest person there. It’s just uncomfortable.
Some days, I feel normal. I feel like myself. Other days, I have no energy, and it dawns on me again. For whatever reason, sometimes it’s triggered.
It’s not, ‘every day is great,’ or ‘every day is miserable.’ It’s a constant up and down. I’ve had to learn not to be so hard on myself on bad days.
What is it like living with an invisible illness?
That has been really challenging. I don’t want to complain because I’m not on the other side of things where I’m losing my hair and look like a cancer patient.
I don’t want to complain, but I still have cancer. I still have side effects from medication. I still struggle emotionally.
A lot of people get excited when I have a good scan, and it’s almost like they think I’m over it.
It’s like, “No, all my tumors are still there.” Everything can change tomorrow. I’m learning to handle that. It’s a struggle that I’m still trying to work through.

What advice do you have for someone who’s just been diagnosed?
Everybody who gets cancer eventually looks up their cancer on the internet, even though they tell you not to. Don’t go off of what you read. Everything you’ll read is terrible and sounds like you’re going to die tomorrow.
Regardless of what you’re dealing with, realize that your mindset about it is going to make the biggest difference. If I gave up, things would be so much.
Even though I don’t want to have cancer, my mindset about it has allowed me to grow so much and opened up a lot of possibilities for me. Realize that you can make cancer a better or worse experience based on how you think about it. It’s all about how you handle it.
I wish I could say something profound that would solve everyone’s worries about it, but I think I’m still learning about it.
Having hope and getting the help you need to get through it is important. Find what you need, and figure out how to get it done.

Inspired by Tara's story?
Share your story, too!
Lung (Non-Small Cell) Cancer Stories
Yovana P., Non-Small Cell, Invasive Mucinous Adenocarcinoma (IMA), Stage 1B
Cancer details: Had no genetic mutations; IMAs comprise between 2-10% of all lung tumors
1st Symptoms: No apparent symptoms
Treatment: Lobectomy of the left lung
Dave B., Non-Small Cell, Neuroendocrine Tumor, Stage 1B
Cancer details: Neuroendocrine tumor
1st Symptoms: 2 bouts of severe pneumonia despite full health
Treatment: Lobectomy (surgery to remove lobe of lung)
Terri C., Non-Small Cell, KRAS+, Stage 3A
Cancer details: KRAS-positive, 3 recurrences → NED
1st Symptoms: Respiratory problems
Treatment: Chemo (Cisplatin & Alimta), surgery (lobectomy), chemo, microwave ablation, 15 rounds of SBRT radiation (twice)
Heidi N., Non-Small Cell, Stage 3A
Cancer details: Non-small cell lung cancer (NSCLC)
1st Symptoms: None, unrelated chest CT scan revealed lung mass & enlarged mediastinal lymph nodes
Treatment: Chemoradiation
Tara S., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Numbness in face, left arm and leg
Treatment: Targeted radiation, targeted therapy (Alectinib)
Lisa G., Non-Small Cell, ROS1+, Stage 4 (Metastatic)
Cancer Details: ROS1+ tends to be aggressive. It can spread to the brain and to the bones.
1st Symptoms: Persistent cough (months), coughing a little blood, high fever, night sweats
Treatment: Chemo (4 cycles), maintenance chemo (4 cycles)
Stephen H., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Shortness of breath, jabbing pain while talking, wheezing at night
Treatment: Targeted therapy (alectinib), stereotactic body radiation therapy (SBRT)
Ivy E., Non-Small Cell, EGFR+, Stage 4 (Metastatic)
Cancer details: EFGR-positive
1st Symptoms: Pain & stiffness in neck, pain in elbow
Treatment: Two targeted therapies (afatinib & osimertinib), lobectomy (surgery to remove lobe of lung)
Ashley R., Non-Small Cell, EGFR+ T790M, Stage 4
Diagnosis: Stage IV Non-Small Cell Lung Cancer
1st Symptoms: Tiny nodules in lungs
Treatment: Tagrisso (Osimertinib)
Shyreece P., Non-Small Cell, ALK+, Stage 4
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Heaviness in arms, wheezing, fatigue
Treatment: IV chemo (carboplatin/pemetrexed/bevacizumab), targeted therapy (crizotinib, alectinib)
Amy G., Non-Small Cell Squamous, MET, Stage 4
1st symptoms: Lump in neck, fatigued
Treatment: Pembrolizumab (Keytruda), SBRT, cryoablation, Crizotinib (Xalkori)
Dan W., Non-Small Cell, ALK+, Stage 4
1st Symptoms: Cold-like symptoms, shortness of breath, chest pains
Treatment: Radiation, targeted therapy (Alectinib)
Tiffany J., Non-Small Cell Adenocarcinoma
1st Symptoms: Pain in right side, breathlessness
Treatment: Clinical trial of Tagrisso and Cyramza