Tony’s Chronic Lymphocytic Leukemia Story
Tony was diagnosed with chronic lymphocytic leukemia (CLL), the most common form of adult leukemia. For treatment, he took targeted therapy BTK inhibitor drug.
He details self-advocacy as a patient, how he broke the news of the cancer to his loved ones, and navigating life with cancer. Thank you for sharing your story, Tony!

Timeline
- APRIL 2016: Needle biopsy, surgical removal of lymph node
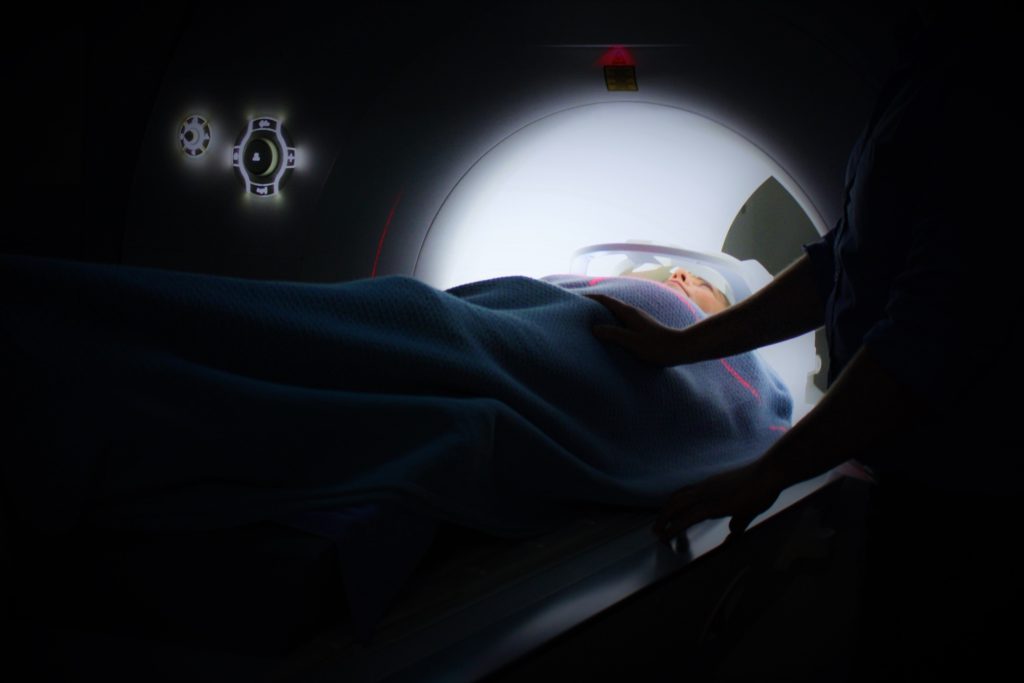
- APRIL 2017: MRI
- JULY 2017: PET scan, bone marrow extraction
- AUG 2017: EKG
- OCT 2017: CT scan
- DEC 2017: EKG
- JAN 2018: EKG
- On-going – Blood tests weekly for awhile and then monthly
- Tests & Diagnosis
- Treatment Decisions
- Chemotherapy
- Mental & Emotional Impacts of Cancer
- Waiting for scan results
- Dealing with the "watch and wait" approach
- Big surprises during cancer treatment
- What helped you manage your emotions?
- What got you through the toughest times?
- Were there moments you had to advocate for yourself in and out of treatment?
- Could you work through treatment?
- Paying for cancer treatment
- How did you break the news to your children?
- How important is it to have caregivers?
- Advice to others who are just now getting diagnosed
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
It’s okay to be anxious and scared about this. You won’t have those feelings 24/7 every day.
I laugh a lot. I have fun. I love my life. I don’t love CLL, to be honest. It’s not part of the plan that I had for my life, but it’s here. At the moment, it’s highly responsive to treatment, and you have to remember that and understand that really is an amazing thing. It is.
Tony D.

Tests & Diagnosis
What were the first symptoms of CLL?
Over the Christmas and New Year holiday period, I felt a lump in the back of my neck. I thought this was a muscle knot and kept trying to rub it out. It got bigger.
I made an appointment with the doctor in early January of 2016. I was told it was probably an infection that had caused a lymph node to enlarge and nothing to worry about.
However, it didn’t go away. About 3 weeks later I met with another doctor, as I discovered another lump. Neither of these doctors were my primary care physician; he was unavailable.
I met with 2 of his partners for these appointments. Since this new lump was lower than the first one, it was assumed that it was still an infection, as a lower lump would imply that the infection was traveling down my body.
At that point I was prescribed an antibiotic, also given a precautionary blood test, and eventually told that it had ruled out any invasive cancers. I decided I was just being neurotic and tried to just wait for the infection to play itself out. It didn’t.
How did you finally get diagnosed?
I made another appointment in mid-March and was able to meet with my primary care physician. He suggested it was time for me to meet with an ENT (ear, nose, throat) and referred me to one he had worked with often.
In early April, I met with the ENT. He did a needle biopsy, which he told me would not really be conclusive. He told me essentially it would let me know if there was a change if I had it, but it could just as easily be incorrect. He did the needle biopsy, and about a week later, I went in to go see him for the results.
Then he told me I had CLL. But in an interesting way, it’s often been referred to by people as the ‘good cancer.’ I’m not sure how you actually put those two words together, but he was told that it was really easy to treat.
It was so much better than all these other possibilities. I left that appointment feeling highly anxious but really mixed. I saw another ENT shortly after that just to get a confirmation and make sure we were on the right track.
He confirmed it was CLL.
I was next scheduled for surgery to remove one of the lymph nodes, as well as some other tissue. One week later on May 5, 2016, the results were in, and I was diagnosed with chronic lymphocytic leukemia (CLL) — a form of leukemia.
Editor’s note: The same cancer found in lymph nodes, not the blood/bone marrow, is classified as SLL, a type of non-Hodgkin’s lymphoma.
How did you process the cancer diagnosis?
People often describe these things as a journey or a rollercoaster ride of emotions. Those didn’t seem to work for me. I was not going on a trip, and there were no thrills involved.
Honestly, it just sucked. Sometimes I’d be angry or numb or beyond sad, and other times optimistic.
My wife had breast cancer about 10 years ago, and she went to the same center. We both walked into that meeting thinking, “Okay, they’re going to tell us what the treatment is. Get into treatment, and it won’t be fun, but then the cancer will be gone. We’ll go back to sort of ‘life as we know it currently.’”
But when we got into the meeting and she was explaining it to me: “CLL does not currently have a cure.” It’s very receptive to treatment for the vast majority of people, so she helped me understand that, that we weren’t going to go in, do some chemo, and everything was going to be fun.
I don’t mean that in a light way, but I was hoping for a beginning and ending point. This currently doesn’t have that way of thinking about it.
»MORE: Processing a cancer diagnosis
Dealing with CLL as a chronic illness
Getting adjusted to the idea that I will likely have this the rest of my life. Obviously there’s lots of research that’s being done, so that could change. In 2 years we could be looking at a completely different scenario.
But it’s not 2 years from now, so when [my oncologist] was telling me this, I was asking her about the treatment potential. At that point she had not done most of her tests, CAT scans and all the other kinds of things that needed to be done.
Essentially, she laid it out as I would have a couple options for treatment. Those would hopefully kick the CLL into remission, and that would be for an indefinite period of time. Then when it came back, when the symptoms started to reappear, I would go through treatment again.
Those intervals, the remissions would become shorter. But she also said it’s harder to know what that means. Some people go into remission for years. Some people go into remission for shorter periods of time.
I overused the word ‘anxious,’ but that’s pretty much where I was. I just walked out of that meeting going, ‘Whoa, this is not what I was expecting at all.’
Support from your spouse
The good fortune that I have is my wife has been through this experience of cancer.
Being a survivor, she continues to live with the fact that she had cancer and none of us are promised a complete cure. She’s had a lot more time to think through all of those things.
She goes in for the anxious breast exams and all of those kinds of things. That was really helpful. She really helped me to scale it back, so I didn’t go completely off the edge of the cliff and try to stay as focused as I could at trying to figure out what the next steps were.
If there’s a short answer to your question, it was horrible. I don’t know how else to describe it. I don’t know that it’s ever a part of anyone’s game plan, but it was definitely not part of my game plan.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer

Describe each test and biopsy you experienced
- APRIL 2016: Needle biopsy, surgical removal of lymph node
- APRIL 2017: MRI
- JULY 2017: PET scan, bone marrow extraction
- AUG 2017: EKG
- OCT 2017: CT scan
- DEC 2017: EKG
- JAN 2018: EKG
- Ongoing: Blood tests weekly for a while and then monthly
Most of the tests were non-invasive and pain-free. The bone marrow extraction sounds awful, but it was done at the medical center, and I never felt anything despite being awake throughout the procedure.
I didn’t have much of an issue with the MRIs, but was a bit concerned about the confined space and did take Xanax before each one. I was surprised that for one of the MRIs they put a kind of cage over my face (oddly Hannibal Lector-ish!) because I couldn’t move my head. I would have appreciated knowing that ahead of time, but it wasn’t really a big deal.
Treatment Decisions
How did you choose hospitals?
I went to Lacks Cancer Center for two reasons. Most importantly, it provides coordinated care. I typically go in and have blood tests and then see my oncologist about 20 minutes later.
She already has my test results by the time we meet. They also have a pharmacy, social workers, a mental health therapist, etc.
Most of my tests can be performed there or in the hospital that is adjacent. They coordinate and set up nearly all of my appointments. This is huge. It makes what is already a stressful experience just a bit less confusing.
The other reason I elected to go there is because they are a research center, and they coordinate with a number of other cancer centers.

What did you like about your hospital?
It’s not a huge medical center, but large enough to offer nearly all the services I need.
I can’t stress enough how much the coordinated care at Lacks has been helpful. I have friends who have not utilized this kind of a center, and they have to deal with the added stress of setting up and coordinating doctor visits and tests on their own. It may not sound like a big deal, but it is.
My doctors talk to each other, and the staff do everything they can to make an already overwhelming situation as manageable as possible. I can’t say enough about them and wish that everyone had this option.
Chemotherapy
What treatment regimen did you undergo?
I had 2 options:
- I could do several sessions of chemo and immunotherapy to push the CLL into remission. My oncologist did tell me that this would be intense, and I would have to stop working throughout the treatments.
- The second option (which I elected) was to begin taking a medication called Imbruvica, or ibrutinib. I take 3 capsules per night and will continue to take this until it no longer works. In both cases, the remission period is indefinite, so I decided to start with the less potentially debilitating medication route.
I should note here that there are a number of criteria you have to meet to qualify for using Imbruvica (hence the bone marrow extraction), but I qualified. In August, I will have been on this medication for 1 year.
Describe week 1 of the ibrutinib pill
Looking at the list of potential side effects for Imbruvica is a bit overwhelming. Thus far, I have been fortunate and have not experienced many side effects.
Recently, I started taking a medication to lower my blood pressure, as elevated blood pressure can be a side effect. I also bruise and bleed more easily, but not really very problematic.
Did the weeks get better or worse?
When you take Imbruvica, your blood has to be checked weekly for a fairly long period. It was explained to me that as the medication attacks the cancer cells in my blood, this impacts the white cells, etc. Mine continued to improve and are currently at normal levels.
When I was not feeling as great, it was usually one of two things. My bones were aching, or I was nauseous. The latter was the biggest pain. It turns out that I have a lot of enlarged lymph nodes in the trunk of my body. Add to that the “fatty liver” fun, and you get nausea.
Describe any hair loss
I’m 63 and already have experienced a receding hairline. I have noticed more loss, but not really anything worth worrying about.
Mental & Emotional Impacts of Cancer
Waiting for scan results
One of the advantages of the coordinated care I receive at Lacks Cancer Center is a very fast turn around on most tests, including MRIs.
I had the usual nerves while waiting for results, but the folks were great about trying to get information to me as quickly as possible, and I can also call them at any time with any questions without feeling like I’m being neurotic!
Dealing with the “watch and wait” approach
My first year was monitoring without treatment — “watchful waiting.” On the one hand, I was happy not to have to start any treatments. On the other, I was often anxious about when things would change and I would begin treatment to the point where it felt obsessive.
My medical team was amazing at helping me to understand what was going on with my body/cancer, and that was helpful. Lacks also has a therapist who only works with oncology patients. I found that meeting with him was invaluable.
Big surprises during cancer treatment
This shouldn’t have been a surprise, but it was: my body no longer responds to some things the way it used to. For example, I am more susceptible to infections and viruses.
In December of 2017, I got an ear infection (as far as I know, my first ever), and in one day it got so bad that I had to go to the doctor’s, but it was too little, too late. My eardrum ruptured, and it took nearly a month to get everything healed.
On another occasion this past fall, I got food poisoning. I looked up the typical duration, etc. and just tried to stay hydrated. Bad idea.
In fact, just about everywhere you look at Lacks, there are signs indicating that at the first sign of illness I should contact them. I didn’t. I ended up being extremely dehydrated in just a few days and had to go into Lacks to be hooked up and hydrated.
What helped you manage your emotions?
The cancer center has a therapist available who only works with oncology patients. He has been amazing for gauging how I have been handling things emotionally based on his experience with other patients. He also helps me with strategies for managing my emotions, promoting good mental health, etc.
I also started writing a blog about my experiences. Doing so was both cathartic, and it gave me a venue that gave people a way to talk with me about cancer.
I have found this really helpful, as most of us don’t know what to say in these type of situations. When people don’t talk about your cancer with you, it can get very lonely.
And laughter.
Sometimes people ask about my use of humor regarding my experiences with cancer. Here’s what I think. Cancer can steal a lot from you: peace of mind, a sense of healthiness, etc. But at some level, I have to maintain some control.
Humor has always been my best defense, and I have no intention of allowing cancer to control it. Don’t be fooled, though.
I hate cancer. Having it sucks. It scares me. It makes me beyond sad and angry at times. But I have to take control where and when I can, so sometimes I laugh.

What got you through the toughest times?
See above and add: family, friends and the kindness of others.
It [was filled with weeks] of emotional highs and lows. I suspected that would be the case for some time. I was not sure I’d ever felt so loved and cared for by so many people. So many notes, texts, phone calls, etc. of support. One thing I have discovered is that I have to take a break from thinking about cancer at times.
Were there moments you had to advocate for yourself in and out of treatment?
Initially, my doctors followed all of the recommended protocols for responding to my symptoms. What didn’t happen was follow-up. I initiated most of those.
It made me feel a bit like I was being neurotic by calling for appointments. The lesson I learned, even if you have great doctors, you have to advocate for yourself and listen to your body.
Could you work through treatment?
Yes.
Paying for cancer treatment
I am thankful every day for great insurance. Additionally, the social worker at the Lacks Center completed paperwork that reduced the enormous costs of the medication I am taking daily.
How did you break the news to your children?
When my wife was diagnosed with breast cancer (10 years ago), we were at Lacks Cancer Center, and they had a whole team of people who met with us, including a social worker.
I think I was, it was fair to say, fairly nearly hysterical at that point. My wife was actually handling it better than I was.
What I said to the social worker at the time was, ‘We have to go home, and we have 2 very young children at home. They don’t even know that we’re here. Somehow we have to explain this to them. How do you even do that?’
I will never forget her because what she said was like, ‘Be honest with them. Tell them what they need to know. You will always be truthful with them.’
Our kids were very young, but the thing she said is, “What kids and young adults or anybody in your life fears is what you’re not telling them. That you’re hiding something.”
We were honest. My wife brought both of the kids one at a time to sessions where she was getting radiation. The technicians showed them how it would work, all of those kinds of things.
When we told the kids about my cancer diagnosis, my kids are older. It was oddly enough equally difficult, and in some ways, it was a different kind of level of difficulty because they were adults.

How important is it to have caregivers?
Essential. My wife or another family member has gone to every appointment and medical test with me.
In addition to providing emotional support, having someone else at an appointment allows you to have another set of ears. I am often too emotionally involved/anxious, and I either misinterpret what is being said or miss it all together.
Advice to others who are just now getting diagnosed
I was often told I had the “good cancer.” I don’t even know what that means. True, CLL is often very responsive to treatment, but it is not currently curable.
Take it seriously and do everything you can think of to keep yourself healthy mentally, physically and emotionally.
Be prepared to make adjustments. I now buy flight insurance in case I end up not being able to take the trip I was planning on due to medical changes, etc.

Inspired by Tony's story?
Share your story, too!
Chronic Lymphocytic Leukemia (CLL) Stories
Nadia K., Small Lymphocytic Lymphoma (SLL)
1st Symptoms: Rash, lump under arm, fatigue
Treatment: Ibrutinib and acalabrutinib
Tamsin W.
1st symptoms: Out of breath, dizzy, nauseated, tiredness, palpitations
Treatment: Obinutuzumab & venetoclax
Michele N.
1st Symptoms: Slow healing, scalp infection, enlarged lymph nodes
Treatment: Clinical trial of ibrutinib, fludarabine, chlorambucil and rituximab; acalabrutinib
Sean R.
1st symptoms: No apparent symptoms; went to ER for unrelated shoulder pain
Treatment: Clinical trial, Ibrutinib & Venetoclax
Tony D.
1st Symptoms: Lump in back of neck that got bigger in a couple weeks
Treatment: Targeted therapy - orall pill (Imbruvica), takes 3 pills a night