Tamsin’s Stage C Chronic Lymphocytic Leukemia with 11q Deletion Story

Tamsin was 47 when she was diagnosed with chronic lymphocytic leukemia (CLL), the most common form of adult leukemia. She’s a mother of two teenage daughters and owns a recruitment business with her husband. She shares what it was like to navigate getting a CLL diagnosis and going through treatment, especially during a pandemic.
- Name: Tamsin W.
- Diagnosis:
- Chronic Lymphocytic Leukemia (CLL)
- 11q deletion
- Subtype of leukemia
- Staging: C
- Initial Symptoms: Out of breath, dizzy and nauseous every morning, tiredness, palpitations
- Additional Symptoms: Shoulder pain, night sweats, inexplicable weight loss
- Treatment:
- Obinutuzumab & venetoclax
[Cancer] doesn’t define me… It’s taken over my life for the last year, but there’s so much more to life; that is one part of it.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Pre-Diagnosis
Video
What were the initial symptoms for you?
I was really out of breath… feeling dizzy and sick every morning. When I got up and went on a dog walk, I felt really nauseous but I just kind of got used to it.
The tiredness and palpitations, [they] all just started coming on. Maybe it’s my age [but] I’ve always been really fit and active, so I thought it was really weird.
I started going to the doctor about everything that was happening. It was over a period of time, but I got used to it.
How did it go when you first saw the doctor?
When I went to the doctor, obviously they were looking for something. They were concerned because also I had low iron… low ferritin. I was anemic for probably about six months.
They started by looking for cancer. They did an endoscopy [and] a colonoscopy, and then they sent me for a chest X-ray because I had palpitations.
I went private because some of it was during COVID [so] it was really difficult to get in and see the doctor.

Can you describe how your heart palpitations felt?
I work in recruitment, so it’s quite stressful. Always used to get up at half four, I’d start working, [then] go to the gym at half six. Sometimes I’d have really difficult conversations with candidates or clients.
I remember having one particular candidate. It was a difficult situation and literally, I had to lie down on the floor after I got off the phone because it was like my whole chest was coming in and out. I didn’t know what was wrong… but you just get on with it.
I was lying in bed and felt really ill, thinking, ‘I hope I haven’t got cancer.’
What was going through your mind?
When I was waiting for the colonoscopy and the endoscopy, it was during COVID, so it was taking forever. I ended up paying for it and going private because I was so frightened.
The day of the colonoscopy and the night before, you have [to take] loads and loads of fluid, which made me feel really ill. I was lying in bed and I felt really ill… thinking, “Gosh, oh, I hope I haven’t got cancer.”
I didn’t feel well at all. “It can’t be. It can’t be.” That’s what I was thinking. I just felt so awful. I was really scared that it was going to be that.
Then they didn’t find anything.
Ruling out cancer
Because I was anemic, I think they were looking for a cancer mass. They were either looking in my stomach or in my colon. They were looking for an actual mass of cancer. They wanted to eliminate it.
That’s what they say, isn’t it? We’re going to put you on a pathway, but we want to make sure it’s nothing, not severe. Just to rule it out, that’s what they say. They just wanted to rule out that it wasn’t cancer.
You got great news!
There’s nothing on the colon. We are so pleased. I had a little label [that] I stuck up on my board where my work is and the picture of my girls. If I had a bad day or didn’t feel well, I used to say, “Thank God I haven’t got cancer.” I’d look at my little label and say, “It’s all okay.”
Then they sent me for the chest X-ray and that came back clear as well. So that’s amazing. And then basically that was it.
I didn’t know what was wrong with me… I was exhausted and I thought, ‘None of you actually know how I’m feeling.’
But now what?
I didn’t know what was wrong with me. Then you think, everyone’s life is carrying on, I’ve just got to carry on. I carried on.
I was still working full time, training at the gym all the time, and I was pushing myself. People would say, “She can’t really be poorly because she wouldn’t be able to get up at half four in the morning, won’t be able to do the gym, wouldn’t be able to work.”
I was exhausted and I thought, “None of you actually know how I’m feeling.” But everyone says, “Oh, you can’t possibly be.”
What happened when you went to see a cardiologist?
They put a heart monitor on me for a week. They didn’t see anything that was untoward. There was only one little blip. They said, “You’re probably okay.”
I still [don’t] feel good, but I’ve had all those checks. Maybe it is just my lifestyle, the way I get up early, train, work all the time, kids… Everything.
I was still really tired and felt nauseous… had a pain in my right shoulder… and the pain in my groin.
New symptoms
I was still really tired and felt nauseous. Then I got my lymph nodes up in my groin and I just put it down to overtraining at the gym.
I had a pain in my right shoulder. I did have a steroid injection to get rid of the pain in there and the pain in my groin. I went to the doctors, and they felt all the lymph nodes were up.
What kind of pain were you feeling?
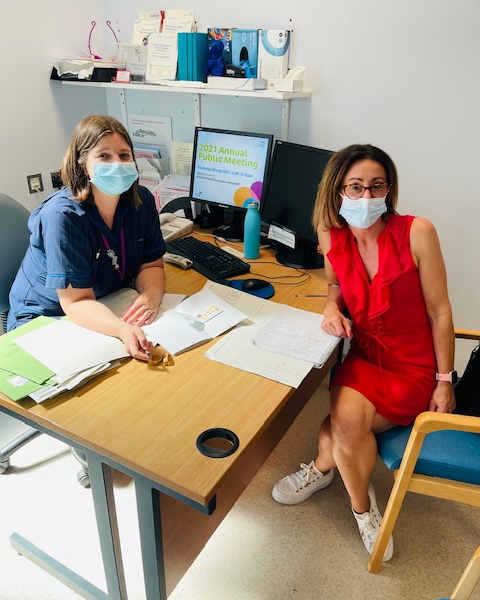
It was in my shoulder blade. I thought I had been overtraining and it was just constant. It was painful the whole time. It was just always there, like a dull ache, and it hurt whenever I moved it. And that’s where the cancer was in my bone marrow, in that shoulder.
Then in the groin, it was really hard. My stomach was pretty rock hard. The lymph nodes were up in my stomach as well.
Night sweats
I got these night sweats and I thought, “Maybe it’s because we’ve changed the duvet. Is it my age?” All these things. Probably only four weeks of night sweats. It was very quick, right at the last bit.
Inexplicable weight loss
I’ve been doing lots of weights and everything [so] I had dropped a little bit of weight and the rest of it came off.
I remember going to Cornwall to see my sister and would eat loads of chocolate, ice cream, fish and chips, and everything. Came back and weighed in; I was seven and a half stone. I thought these scales are broken. Literally thought they were broken.
People were saying to me, “Blimey, you’re really skinny. What have you been doing?” And I said, “I’ve just been working out loads. I’m really tired. I’ve been working at the gym and working hard.” But I was really skinny and, everything wasn’t right. I didn’t feel good. It didn’t feel right.
Everything wasn’t right. I didn’t feel good. It didn’t feel right.
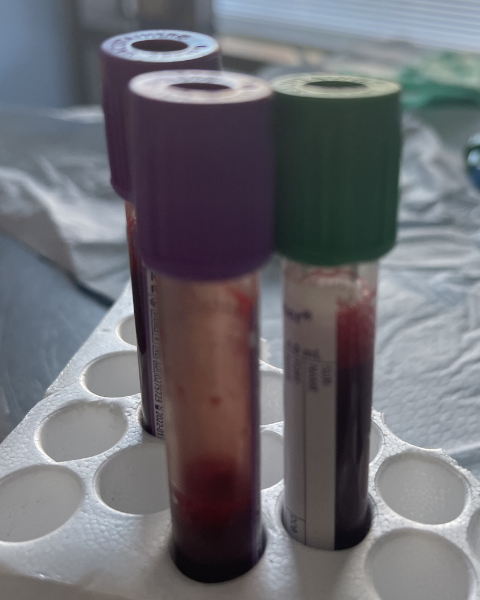
Diagnosis
“The” blood tests
I went to see a really lovely doctor that I’ve had for years. I said, “I am so tired.” He said, “Well, Tam, with your lifestyle, who wouldn’t be?” I said, “I know, I’m really tired, but my lymph nodes are up.” He felt those and I said, “I want a full blood count.” He said, “Okay, I think you’ll be absolutely fine.” I said, “Yeah, me too.”
Life was so good. We’d just moved into office accommodation. I’ve recruited a new person. [The] business was amazing. The girls were good [and] my husband, [the] family’s good. I know I’m going to be okay. I was absolutely sure.
He felt in my groin. He felt them up there. He felt under my armpit, didn’t feel them there, didn’t feel them in my stomach. He said, “I think you’ll be okay.” Literally, I ran out of the doctor’s surgery and thought, “I’m going to be okay.”
Getting “the call”
I was at work and I went to view a property and that’s when I got the call from the doctor’s surgery telling me to go in straight away to pick up a letter to go to [the] hospital that night. I got the call and I said, “I’m really busy. I’m actually at a property. I’m really busy.” She said, “You’ve got to come into the doctor’s surgery now.”
She said, ‘You’ve got to come in now and then you’ve got to go to [the] hospital.’
I felt really irritated because I didn’t want to have a call like this because I wasn’t expecting it and [she] said, “You’ve got to come in now because you’ve got to go into [the] hospital. You’ve got to go to QMC and they’ve got to rehydrate you because you’ve got something showing that you’ve got hypercalcemia.” I thought, “Well, what’s that?”
I said, “Do I have to come now?” She said, “You’ve got to come in now and then you’ve got to go to [the] hospital.” I said, “What? Straight to [the] hospital?” And she went, “Yeah, you’ve got to go straight to [the] hospital.” And I said, “Shall I wait for my husband?”
I just couldn’t quite believe it all. She went, “You’ve really just got to check in and get on your hydration as soon as you can.” So I drove straight to the doctor’s. She said, “I’ve got this letter for you to go to [the] hospital.”
I took the letter and I literally drove to [the] hospital. Rang my husband and said, “I’m going to [the] hospital. I’m going to Acute Admissions. Meet me there in a bit or I’ll ring you in a bit.” That was how kind of quick it was. It was just bonkers.
I was really worried because I thought there must be something really wrong with me… I had a weird feeling.
What were your thoughts after getting the call?
I must have been so frightened. I remember ringing a friend on the way to [the] hospital and I just said, “I don’t know why they’re getting me in so quick.” I didn’t know what it was for.
I don’t like to Google anything but I’ve been driving… going literally from the doctor straight into town. I was really worried because I thought there must be something really wrong with me.
Also, it was one of my best friend’s 50th birthday and we were supposed to be going to Wales. I had a weird feeling. I just thought, “There is something really wrong with me. I’m not going to make it. I know I’m not going to make it go away.”
Then I checked in and they put me on the drip to get me rehydrated.
First hospital stay and more tests
I thought I was going to come home. Then they said, “We’re going to put you on a drip for 12 hours.” I was like, “Oh, my goodness, what? So I’m going to be here overnight? I haven’t got anything on me.” I had to ring Mike and the girls, and they brought my suitcase in and they found me. It was like an admissions ward. There are about 30 people in there.
I saw a doctor and a whole load of trainee doctors. They did an examination of me and then they said, “We’re going to run a load of tests tomorrow.”
I still didn’t really know what I was in for. I kind of knew. I’m sure they must have said we’re going to run some tests to see if it is what it is. But it was surreal. It was like someone else’s life.

It was surreal. It was like someone else’s life.
Getting the diagnosis
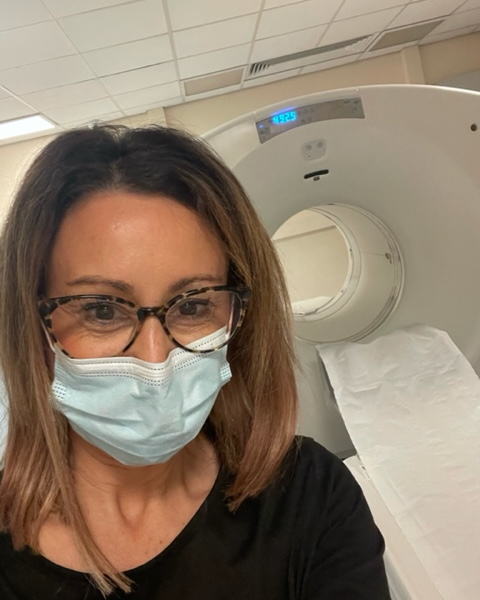
In the morning, they came in and said, “We’re going to test you. Do your [blood tests]. Put you through a scanner. We’re looking for blood cancer or lymphoma,” or whatever they said.
I was in this bed with the curtains around me and I thought, “Oh, my goodness.” Then I told my family everything.
They did all the tests and said they’d get back to me in the morning because I’d gone and had these tests quite quickly. I thought by lunchtime they’d let me know and they hadn’t.
I’ve been on my own the whole time and I was really fed up because I hadn’t had my results. I actually knew someone that worked at Queen’s Medical Center — he was a surgeon — so I texted him. He came down, sat on my bed, and talked to me for a bit, so that was nice.
Then [the doctor] came through and she said, “We’ve run your [blood] and you have got blood cancer and we need to carry on testing you so we’re going to be keeping you in. Is there anyone that you’d like to ring?” I said, “I’ll call my husband now then.” So I did.
You can’t sugarcoat it. I’m really direct and I like things in black and white.
The first thing I said is, ‘How long have I got? Have I got three months? Have I got six months?’
Initial reaction to the diagnosis
I think the first thing I said is, “How long have I got? Have I got three months? Have I got six months?” I’d never had blood cancer. They didn’t know what cancer it was.
They said they’ve got to do lots more tests on me, bone marrow and all the rest of it. She kind of said, “It’s not like that, but we’ll let you know. We’ll get on with everything. We’ll transfer you from this hospital, and then you’ll be an inpatient and they’ll get on with everything.”
I don’t know initially what I thought. I just didn’t know what to expect. As soon as you get a cancer diagnosis, you think, “That’s it.” But they were really good when they moved me over to the other hospital. I met one consultant and then I met my [CLL] consultant. Then it felt better.
What helped get you through that time?
It was just getting through every day. I slept in one night and I remember speaking to a friend. I Facetimed her and she said to me, “Oh, my God. You look awful. Just do your hair and get your makeup on and crack on with it.” And I thought, “You know what? That’s it. I can never be a mess.”
I’ve had [an] allergic reaction so I have looked horrendous after I initially had Obinutuzumab. But I told myself, “I’ve just got to get on with it every day and I’ve got to put a smile on my face and just crack on with it, with everything.”
When bad things happen, I’ve got to do that and that’s really what I’ve done. For my girls. I didn’t want them to see I’m not going to go to pot over it. I’m not going to fall apart. I can’t fall apart because of it.
I told myself, ‘I’ve just got to get on with it every day and I’ve got to put a smile on my face.’
I’m not going to fall apart.

Finding out what’s important
At the time, I didn’t want my whole life. I couldn’t go to work. My husband had to hand his notes in at his job so he could run the business. Overnight — because I had [to] stay in [the] hospital — I had to suddenly let everything go.
All of a sudden, the most important thing in the world was — when they let me out the first weekend — just seeing the girls and coming home and family. My other half, my dad, his partner, and talking to family. You suddenly realised what is really important.
I’m really competitive at work. I’m competitive in lots of different ways and I strive for more all the time. Then all of a sudden, it came down to what’s really important.
A lot of the time, I get grateful every day for being alive and that’s how I start my day.
Video

Processing your emotions
It’s really difficult, isn’t it? A lot of the time, I get grateful every day for being alive and that’s how I start my day. Remind myself that I’m really lucky because it might not have been like this if I hadn’t been diagnosed. It wouldn’t be like this.
Then on the other side, the hard side, I had allergic reactions with Obinutuzumab that brought my whole body out, an enormous rash. I had to have an ambulance out because they thought my throat was closing up. Those times, you feel absolutely on the floor and I won’t go into it too much because I’ll end up crying for ages.
Lowest point
There are really dark days and there were really bad times. But I did reach out when I felt really, really bad because there were some days that I just thought, “You know what, I’m not going to do this anymore.”
I did reach out, but I’ve never felt like that before. And thank God I haven’t felt like it recently, but those days, they do come.
Also with COVID and shielding, I felt like I’d given up my business. There’s one day [when] Mike drove off, driving my car to my workplace with my girls in the office. But then I’ve got a different life today. I do work. At the time, it was just really hard.
There are really dark days… there were some days that I just thought, ‘You know what, I’m not going to do this anymore.’
Getting help
I did reach out to Macmillan Gateway in Nottingham when I had those days where I didn’t think I was actually going to… I didn’t want to do it anymore. That was my lowest and no one would understand — unless you’ve been there — what it’s like. It’s really, really just awful.
We have Macmillan’s Nurses, but there was another one called Macmillan Gateway that was a charity and it’s based where I live in Nottingham. I just rang them up and I said how awful I felt.
It was the first time I’d said it and it took me months to say it… I just didn’t want to carry on. I reached out and they were really good. They then gave me some sessions with someone on Zoom and then I noticed my improvement.
I just had to find ways around everything, like ways around shielding. How I could go out and see people and just everything with things with work. I have had to find different ways of coping and getting around situations, like being able to see friends.
I used to love going out and then all of a sudden, you’re stuck in because you’ve got no immunity and [there’s] COVID. It was hard.
When I was down there, I couldn’t see a way out… Everything was really difficult.
How bad did it get?
[I] just basically [wanted] to take an overdose. [It’s] just not wanting to wake up.
You can’t really talk to any friends or family about it because no one gets it. Everyone’s trying to be really positive and upbeat. Everything is being done to help you. It’s all really good, which it is.
I’m absolutely eternally grateful for all of that help, the hospitals, everything, and my consultant nurses.
But that feeling of everything’s disappeared overnight… I don’t have that life anymore. I’ve got to live this life. Do I want that life? I do want that life today. That’s the difference. I do. But when I was down there, I couldn’t see a way out.
I was just at the beginning of all the treatment, the allergic reactions, and feeling awful. Also, I was on a lot of painkillers and steroids. My body’s never had loads of stuff like that and it’s going to have its toll on you.
I just felt everything was hard. Everything was really difficult. I’ve never felt like it before.
I got help. I’m just really grateful for the people that were there.

The importance of a support system
I did reach out and I got help. I’m just really grateful for the people that were there. It’s got to be professional people that will be able to help you because no one else understands that.
I’ve got a really good blood cancer friend and she gets it. Someone else with a similar [diagnosis], if they’ve got blood cancer or other people like those.
A really lovely guy [who] came and fixed the windows, he’d had another blood cancer. You get it if you’re in the same exclusive club. The cancer club. It’s always good to talk to other people with cancer that’s been through treatment.
When I went into [the] hospital and with my allergic reaction — because I kept having to go back in — they were going, “Oh, yes, you’re the one with the allergic reaction,” because I had it so badly and no one had had an allergic reaction like that recently. I knew it was pretty rough.
I think the mental side of it, the leaving [and] having to step back from work and step back from my whole life as I knew it overnight. It was just gone, from Thursday through to Friday, it had disappeared and we had to move really quickly. My husband got into the business so that was great.
The most important thing was the girls, really, they kept me going. That’s it, isn’t it? Family, friends.

Breaking the news
How did you tell your children?
I was in [the] hospital Thursday, Friday, and then they let me home Saturday morning. [When] Mike brought me home, we sat in the kitchen and I just said to him, “I just basically have to be honest, I wear my heart on my sleeve. And also I’ve got to tell them that I’m having a load of tests next week.”
I’ve always been honest and I’m really straight down the line. If I think something, I’ll say it. I am really straightforward and I just kind of said it how it is. I said, “You know what? I’m going to do everything I can to keep on going.”
I didn’t know at the time that blood cancer can be treated over a long period of time. I felt like, “Oh, I’ve got to fight it.” I don’t feel like that now. But I said, “I will fight it and I will do my best and I will.”
I tried to reassure them, but it was awful. There [were] a lot of tears. It was really, really sad. And it was tough, really tough. It was horrible. It’s something you never want to have to do. But you do have to do it.
I think for me, just being they were teenage girls, just to be honest with them. I’ve always been the way I am. I think that was the easiest way for me to be just straight down the line.
Mike had to ring round my family because I couldn’t speak to anyone. When I was in [the] hospital, I couldn’t do it. They all knew the results were coming in so he had to sit in the car and ring everyone. So that was tough for him.
I tried to reassure them, but it was awful… There [were] a lot of tears.
Being open about the diagnosis
I told everyone [because] I had this thing in my head that if we talk about stuff, it becomes less scary. I share everything to do with work and my personal life.
One of my friends [said], “Why are you going to share that on Facebook and Instagram [with] your clients and stuff?” I said, “Actually, all my friends know and all my clients and candidates to me are friends. And if I make this less scary for my daughters and all my daughter’s friends can talk about it, and everyone talks about it as if it’s normal rather than it being, ‘Oh, my goodness, she’s got blood cancer.'”
I just thought, if we can all talk about it, then that’s the best thing. Then the people in the community can help support the girls, their friends can, and the mums and dads… and that’s what they did. They picked up the girls. I think, for me, just say it how it is.
If we talk about stuff, it becomes less scary.
Testing
What’s the lymph node biopsy like?
It’s like a little puncture and they take a tiny bit out. So it hardly takes any time. It was all right. [Like a] local anesthetic. Just an injection. Then literally it’s over and done within 3 seconds.
What was your experience doing the bone marrow biopsy?
The first time they did it, they did it when I was a patient in the ward in the hospital. They said, “We want to do it quite quickly, so we’ll do it on the ward. But if you want to do it as an outpatient next week or whatever, then you can come back and you can have gas and air.” And I was like, “Oh, gosh, no, I just want it done.” So they said, “Okay, well, we can’t give you any relief or whatever.”
There was the doctor and someone else and [the procedure was done] without any gas and air. I lay on the bed and I’ve never felt anything like it. That pain was just unbelievable.
I was in labor for about 48 hours with my first daughter, but that was then a C-section. But this pain, pulling it out was horrendous. It took about 25 minutes to get it out, so that wasn’t very nice. But when I had it done again, later on, I had gas and air, so that was fine.
Treatment
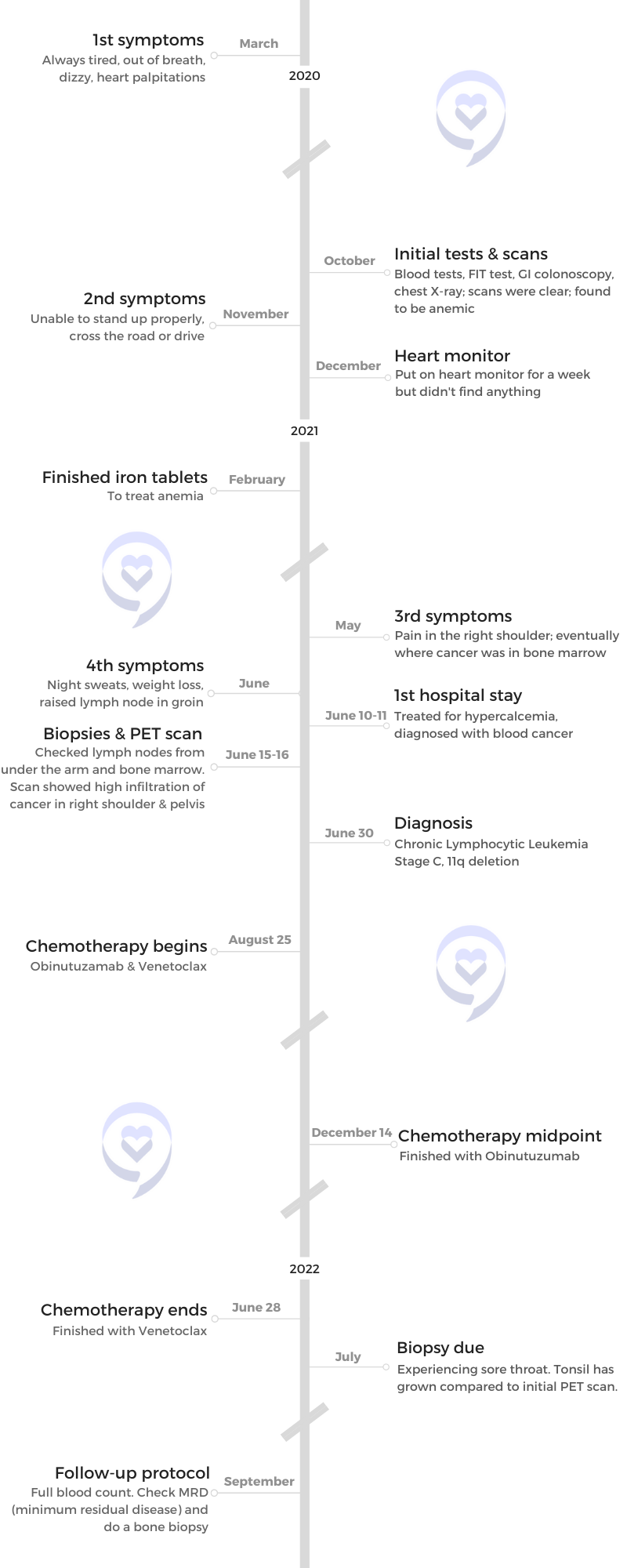
The first doctor’s meeting
I can remember going in for the first meeting… [taking] my notepad and pen and all my questions. I wish I’d got that now on me because I’d be able to tell you what I asked.
[My concern] was how quickly I could start my treatment. It was all new to me. They literally gave me a booklet on chronic lymphocytic leukemia to read because it was all brand new.
Then they also said then that they were looking at my DNA to see what deletions I’ve got and that would determine which drugs I would start on in August. They still had to wait for that. They’d given me the diagnosis.
There were so many questions.
I’d ask questions like, “How long am I going to live?” “How long remission do people get?” I didn’t really understand… “Could I have a stem cell transplant now? Could I have that done now?” But you can’t. That’s the last thing that you have done if you can be treated with drugs.
There were so many questions. I didn’t understand much and I don’t think I took very much in either.
Video
Finding a CLL specialist
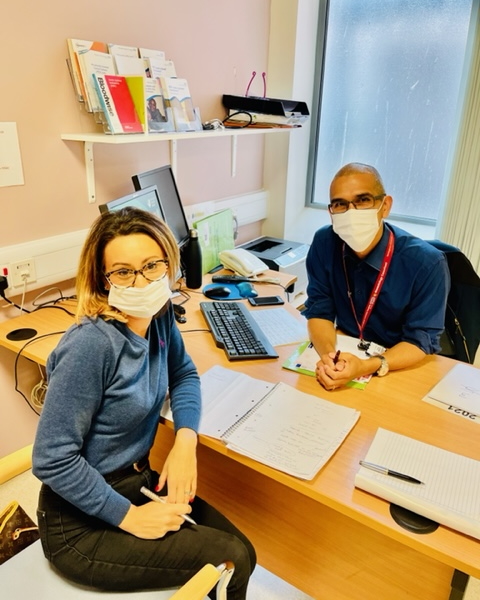
When I was in the hospital and they were doing all the tests on me, my [CLL] consultant, Dr. Martinez Calle, was my consultant from the get-go. He was the second consultant I saw and that is literally who I had from the beginning.
I remember saying to him on the ward, “Are you going to look after me there?” I want to know who’s going to be looking after me because I had seen so many people over such a short period of time. I kept writing all their names down because you just really want someone to be responsible for you and to know that if you’ve got a problem, you know who’s going to deal with it. So right from the get-go, I had my consultant.
What were your treatment options?
There were two. There was a FLAIR drugs trial that I could have done if I didn’t have my particular deletion or there was the Obinutuzumab and Venetoclax.
Venetoclax was approved about four or five years ago, and Obinutuzumab and Venetoclax have got the best results for CLL.
With the prognosis, if it was traditional chemotherapy that I would have had, then with my particular deletion, I think I would have had a worse prognosis. Whereas with these modern drugs, your prognosis is as good as someone without a deletion. I’ve got [as] good a chance as anyone else.
With these modern drugs, they haven’t got all the ten years to say, “Oh, well, so many people get to five years.” On the old medicines, 80% get five years without needing further treatment. There were options, but there weren’t any options when I got my results back. I literally knew what I was going on.
I wanted to know how effective it was and what the results were, what my life expectancy was like.
What was your reaction to your treatment plan?
There are different choices if you don’t have certain deletions, but if you do, then this is the option that will go down. I wanted to know how effective it was and what the results were, what my life expectancy was like.
I was joking. “Oh, are you going to cure me? Will I last the 20 years?” I think he thought I was a bit bonkers because I asked all kinds of funny questions.
He is really good. The thing is, I wanted answers. Am I going to live forever? And it’s not curable, it’s treatable, and that’s what I had to get my head [around]. I was really scared that I wasn’t going to last very long.
Consultants, they are how they are and they just say it how it is, which I like. He didn’t have all the answers that I wanted because I want to live for a really, really long time and I don’t want to have cancer.
What was your treatment pathway?
I was asking what the plan was and why couldn’t I have the transplant straight away. He was saying, “This is what we would do.” He went over it. “Venetoclax, Obinutuzumab, and then when it comes back again, then you can do this. Or if that doesn’t work, well, then we couldn’t do that.”
When I was allergic to Obinutuzumab, they thought they were going to switch me on to an older drug, which they didn’t. But then they got it. I had [an] antihistamine infusion and steroids and all sorts before I’d have my infusion, so I was okay. We didn’t have to swap. But he explained it.
Starting treatment
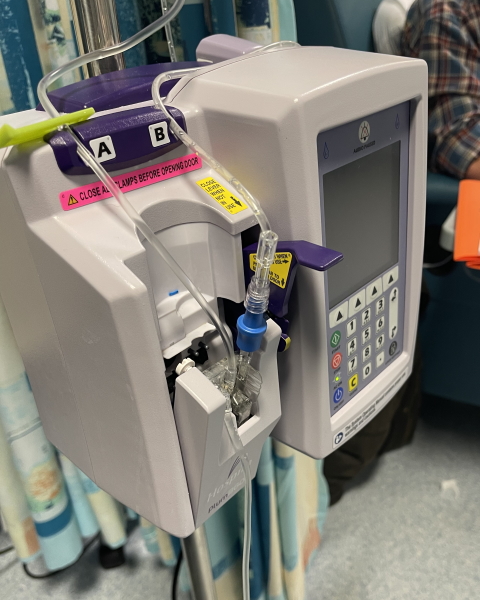
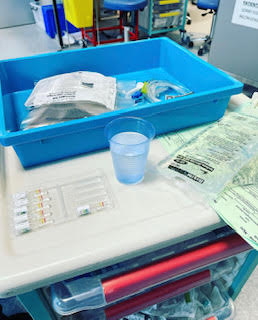
In the beginning, I was on Obinutuzumab from August until the end of December, that was it. Five months and it was quite close together in the beginning. I think it was weekly and then it went further out, spread apart to monthly.
The Obinutuzumab, the first time I had it, they do a tester of 3 hours putting it into you. Then after that, literally I was in about 8 hours, so it was quite a long day on the drip.
I was super organized. They used to laugh because I’d take a massive bag. I’ve got all my food in there, my drinks, my mobile phone charger, a book… I was always on the phone the whole time I was in there.
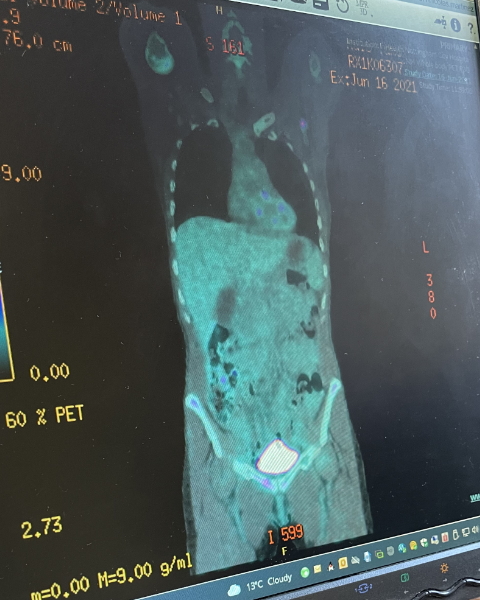
The Obinutuzumab and Venetoclax, I started in August. You start on 100 mg for a period of time. Then they test your blood. Then they go [up to] 200 [mg], then they ramp it up 300 [mg], and then they go again to 400 [mg]. So I’m on 400 mg daily.
They have to test your blood because Venetoclax breaks down the cancer cells so quickly and you literally wee it out, so it can damage your liver and all the rest of it. They keep a really close eye on your blood. I was in and out at the beginning when they were increasing it three times a week to have my [blood tests] done.
The first time, it was just a few hours then it went up to 8 hours. It was always a whole day of Obinutuzumab. It was weekly and then it went kind of monthly and then finished. It wasn’t too bad, to be honest, after they got the allergic reaction under control.

My whole body was kind of all swollen. I felt like my throat was closing up… That was really scary because it felt like I was being suffocated.

Did you feel any side effects with Obinutuzumab?
My whole body was kind of all swollen. I felt like my throat was closing up, so that was pretty bad. That was really scary because it felt like I was being suffocated. That was really horrible.
I feel more tired now at this stage than I did in the beginning. I think you’re in complete shock because I went straight into treatment so I was running at 100 miles an hour at everything anyway.
I didn’t really feel that tired. I felt tired when I first got diagnosed. But then once I started treatment, I wasn’t as tired.
Did you feel any side effects with Venetoclax?
No, not at all in the beginning.
At the moment, I’ve had a sore throat for about eight weeks. I don’t know whether that’s that or just because I’m a bit run down maybe. I’m not really run down, but because you don’t really have much immune system, you kind of don’t know whether it’s the drugs or whether it’s just me.
Post-treatment
Follow-up protocol
They’ll [check the minimal residual disease and do another bone marrow biopsy] after I finish, which is at the end of June and then my appointment back at the hospital is July the 12th.
Then I go to three monthly [blood tests], so they’ll keep a check on it then. I think, that will be it. Hopefully.
I was 0.0045% when they did it out of 500,000 and now they’re going to do it out of a million when I go back. They’ll see hopefully it’ll have gone down because that was [in] December-January [when] I had it done and now it’s going to be the end of June or July so it’s a lot further on. I hope it will be even lower than that. Then I think it’s literally just every three months. Then I’m going to be looking out for symptoms.
In a weird way, I can’t wait to party and celebrate when I finish my treatment.
Preparing yourself for life post-treatment
I’ll be honest. Because I’ve got this sore throat, I’ve got a biopsy in July on my tonsils.
In a weird way, I can’t wait to party and celebrate when I finish my treatment. I’m going to see all my girlfriends, so that’s going to be good. Then it’s just living.
I have got a lot of energy, but hopefully once I finish the drugs and it kind of comes out of my system a bit more… I know with Venetoclax it can build up. [In] the beginning, it’s like that, and then towards the end, it’s gone up, so I know that I’m almost there. I’m almost finished.
Towards the end of my treatment and in August, I’ll probably be quite tired. I hope that I’ll get a boost of energy because I’ll be off the drugs that I’ve been on for absolute ages.


Feeling hopeful for the future
I hope that I’ll have more full energy and I hope that I’ll just live in the day. I tend to live in the day a lot. I am really grateful in the morning and I live every day as if it’s… Not my last day, but I really appreciate everything.
Everything means so much more when you’ve got cancer, doesn’t it? All those special moments.
I used to cry before. Now I cry even more so. I always cry at things like new babies. I can’t help myself. I love new babies, but everything means so much more.
When the girls came out for a walk with us, they said, “Oh, I bet this is the best day of your life, isn’t it?” And I said, “You know what? Yeah, it is, actually. Yeah, it is. Yeah, I love it. You know, it’s really good.”
I don’t want to think about cancer, I don’t want to think about it. But I also need to get my neutrophils and everything back up. And that’s a long-term thing, isn’t it? With blood cancer, you have low immunity.
Everything means so much more when you’ve got cancer, doesn’t it?
Any advice you can share?
I just think live every day as if it is not your last, but enjoy everything. Take every opportunity.
I always think fake it to make it. A lot of days, you can just pretend you haven’t got cancer and forget about it. Especially with a chronic disease, just get on with life and live it.
It doesn’t define me. I know it’s taken over my life for the last year, but there’s so much more to life; that is one part of it.
Just go out there and grab everything and all the people you love. Keep them close to you and just live life. You just have to live your best life every day, don’t you?
Enjoy everthing. Take every opportunity… Especially with a chronic disease, just get on with life and live it.

Inspired by Tamsin's story?
Share your story, too!
Chronic Lymphocytic Leukemia Stories
Nadia K., Small Lymphocytic Lymphoma (SLL)
1st Symptoms: Rash, lump under arm, fatigue
Treatment: Ibrutinib and acalabrutinib
Tamsin W.
1st symptoms: Out of breath, dizzy, nauseated, tiredness, palpitations
Treatment: Obinutuzumab & venetoclax
Michele N.
1st Symptoms: Slow healing, scalp infection, enlarged lymph nodes
Treatment: Clinical trial of ibrutinib, fludarabine, chlorambucil and rituximab; acalabrutinib
Sean R.
1st symptoms: No apparent symptoms; went to ER for unrelated shoulder pain
Treatment: Clinical trial, Ibrutinib & Venetoclax
Tony D.
1st Symptoms: Lump in back of neck that got bigger in a couple weeks
Treatment: Targeted therapy - orall pill (Imbruvica), takes 3 pills a night









2 replies on “Tamsin’s Stage C Chronic Lymphocytic Leukemia with 11q Deletion Story”
This was excellent. My CLL is indolent (CD38). Diagnosed in 2005. Still in Watch and Wait. Symptoms have evolved and I have learned to live with them. I have changed oncologists/hematologists several times for various reasons. it too me almost a year to completely accept the fact that I have CLL.
Thanks for sharing that with us. Your story matters! We’re hosting a CLL Watch & Wait live discussion next Wednesday and we’d love for you to join us. It’s a great way to connect with the CLL community and ask questions directly to experts. Here’s the registration link: https://us06web.zoom.us/webinar/register/4316825510683/WN_2BZkHF7_SiWd_FkAKtQXJQ.