Stephanie’s Stage 2BX Classical Hodgkin’s Lymphoma Story
Stephanie shares her Hodgkin’s lymphoma story after being diagnosed with stage 2BX and undergoing Stanford V (5) chemo and radiation.
Now in remission, she shares her guidance on how to deal with hair loss, being an advocate for yourself as a patient and working during cancer treatment.

- Name: Stephanie O.
- Diagnosis:
- Hodgkin’s lymphoma
- Stage 2BX
- B = having specific symptoms like unexplained weight loss, fever
- X = Bulky disease (site of disease >10 cm or bulky relative to chest size)
- 1st Symptoms:
- Shortness of breath
- Dry cough
- Treatment:
- Chemotherapy
- Stanford V (5)
- 12 weeks
- 1 infusion each week
- Schedule of IV drugs (per Stanford Medical)
- Weeks 1, 5, 9: Mechlorethamine (or Cytoxan on weeks 1 & 5 if you are on a study), doxorubicin, vinblastine
- Weeks 2, 4, 6, 8, 10, 12: Vincristine, bleomycin
- Weeks 3, 7, 11: Doxorubicin, vinblastine, etoposide (for 2 days)
- Radiation
- 20 days
- Monday through Friday for 4 weeks
- Chemotherapy
- Diagnosis
- Treatment Decisions
- Tests, Scans, Biopsies
- Chemotherapy
- Radiation
- Quality of Life
- Describe the hair loss
- What helped with the shaved head?
- What was the worst part of treatment?
- What helped you get through those tough times?
- Finding your cancer community
- Any big surprises during treatment?
- “Be your own advocate”
- Tips on whether someone can work while undergoing Stanford V regimen
- Advice on how to get the right support?
- Message to patients and caregivers now dealing with cancer
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I want to tell them what that doctor told me. Of all cancers you had to get, this is probably the better one because it’s so well researched. It’s so curable.
It’s going to be hard. It’s going to be a disruption to your life, but it’s not going to be life-ending. That for me was such an important message for me to hold on to through all this.
Stephanie O.
Diagnosis
What were your 1st symptoms?
I had been coughing for the better part of a year, sometimes worse than others. That was really my only sign.
I’d been active. I’d been living my life normally, fully. But I was coughing a lot. Then I was going to the health center at school or whatever was available, and they would always just say, “Oh, maybe it’s allergies. Maybe you’re fine health-wise.”
It wasn’t until I came home that, of course — you know mothers — my mom forced me to go get it checked out because she said, “This has been going on too long. You should go get it looked at.” My mom pushed me to get a chest X-ray just to be safe.
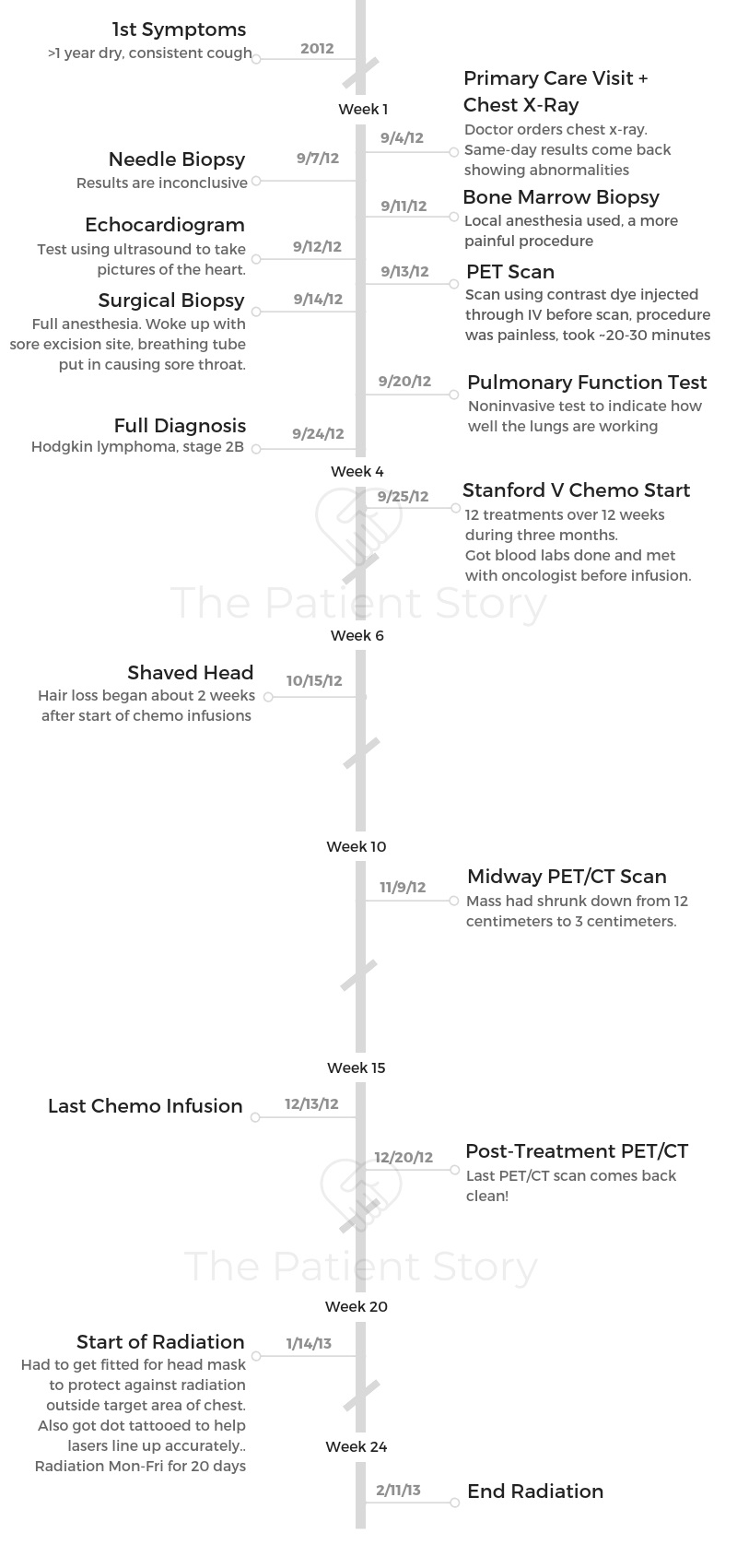
That’s where things all changed. A large mass was found in my mediastinal area, 12 centimeters. What followed was a month of doctor’s visits, tests, scans, procedures, etc. to figure out exactly what was going on inside of me.
»MORE: Hodgkin’s lymphoma patients share common first symptoms
How did you get the official diagnosis?
I got connected to a doctor at Stanford. I remember very clearly that he thought it was going to be cancer, that he thought it was going to be lymphoma.
That it would be a disruption to my life, but it wouldn’t be the end of my life. I remember holding onto that. It made a difference.
It hadn’t spread to any of my lymph nodes or anything like that, so that was good.

How did you process the diagnosis?
I remember the chest X-ray was ordered through my general physician at the time. My mom got a phone call that same day when we came back. Then she just said that something was weird.
You start thinking, but you wouldn’t assume that you have cancer unless you have a reason to assume it.
I remember feeling more helpless before I knew that it was cancer. I remember feeling that limbo, that feeling of knowing something’s wrong but then not really knowing what it is.
I’m someone who likes to have a game plan in life in general, in work, in my personal life. I want to have action steps to take care of problems or to problem solve.
»MORE: Processing a cancer diagnosis
The waiting was one of the hardest parts
The waiting and then the uncertainty. Just not knowing what’s going to happen.
Not knowing what was wrong was a really hard time.
How did you break the news to loved ones?
My mom knew everything before I did in this case. My mom was at the helm of communicating with my doctors and with my nurses.
She would come to every appointment with me, which was so helpful. In retrospect, I think it was hard for me, but that’s just my personality. We just went with it.
»MORE: Breaking the news of a diagnosis to loved ones
Treatment Decisions
How did you decide where to go for treatment?
I have an aunt who’s a doctor in Washington, DC. She knew immediately upon hearing the news that she wanted to do whatever she could to help.
She connected us with one of her colleagues at Stanford, whom I initially met with. He wasn’t an oncologist — I think he was a specialist in heart — so he referred us to Dr. Advani at Stanford.
How did you approach treatment and research?
In retrospect and reflecting on it, I think the easiest way for me to deal with it at that time was just to go with it. To not question it. To just trust the process.
Did you get a second opinion?
I didn’t seek out a second opinion. I didn’t really shop around or try out different hospitals or anything like that. We did Google “Dr. Advani,” and it came back with positive responses.
Looking back, I feel really lucky. We got matched with doctors who turned out to be a real godsend, both in terms of their emotional support, as well as the physical healthcare that they provided.
What did you like about going to a private but larger institution?
When I was going through chemo for lymphoma, I was there once a week. I didn’t really do much else. I wasn’t working, as I mentioned, and friends would come by to visit.
When you’re getting chemo once a week, you basically feel like crap, then recover, and then it’s time for your next chemo.
There wasn’t much time to recover or live life in between. I wasn’t really seeing that many people.
Honestly, the nurses at Stanford became like my best friends in that 3 months I was getting chemo.
I remember they were so friendly. They were so personable. They recognized me; I recognized them. It felt like seeing friends, which was nice.
Some of them have been there since when I got lymphoma or when I had my chemo for lymphoma. It’s just been cool developing those relationships with the nurses.
I think Stanford gave us a sense of security knowing that it’s a well-established medical facility. We just never really felt worried with the care that we were getting there.
Then on the more logistical side, they were very helpful all the time in helping to navigate insurance issues. If we had questions — whatever questions we had while I was getting chemo — they were very helpful.
In terms of what I didn’t like, because it felt so big, they’re often behind schedule. There’s no real sense of schedule there, which I understand why. I would often have to wait a long time for things for appointments.
Did you get a port or PICC line?
I did not get a port nor a PICC line, no. Through both of my cancer treatments, I got everything through an IV.
I think initially they said, “You’re young. Your veins are fine. Let’s start you out with just IVs and then see.”
They also said [it was] because ports and PICC lines are just another risk for infection and just another procedure, so for me I was like, “Great.”
I didn’t really mind being stuck with a needle, so we started it that way and then made a mental note that if we needed to make a change, we could make a change.
Did chemo get harder through the veins?
As chemo went on, I think my veins were mad. All the problems that we’re going through, so it got harder and harder.
Also, for me mentally, it got harder. Physically, I never really was nauseous. I would feel low energy or lethargic sometimes, 1 or 2 days after chemo.
But what became the hardest was mentally going to the hospital and getting stuck with an IV. Sometimes just the thought of being in that room toward the end of my treatment would just make me feel nauseous.
Tests, Scans, Biopsies
What tests, scans and biopsies did you undergo before treatment?
- Chest X-ray
- CT scan
- PET scan
- Needle biopsy (inconclusive)
- Bone marrow sample (most painful)
- Surgical biopsy
- Heart echo (+ bubble test, noninvasive test to assess the flow of blood through the heart)
- Pulmonary function test
Describe the chest X-ray
It was painless. It was quick. I had no idea what this would all turn out to become. It was just a routine procedure. It wasn’t in a hospital; it’s just a walk-in clinic.
It was normal, routine, like when you get an X-ray at the dentist. You wear that heavy lead thing, and it’s just quick, painless and noninvasive. I got results the same day, which I realize now is because it was important. It was abnormal.
Describe the bone marrow biopsy
A lot of these tests happened closely with a full day of tests. They took me to another room, where my nurse practitioner [and another person] performed the bone marrow biopsy.
It struck me because it wasn’t any procedural room. It wasn’t like they took me to an operation room or anything like that. It was just in the normal room you see your doctor in.
I remember thinking, “Okay, cool, it’s just another routine test,” how they did a heart function test or all these other things. They were noninvasive. I remember thinking, “Okay, no big deal.” I have a pretty high pain tolerance, so I’m typically like, “Whatever.”
I remember I laid on my stomach, and then they used a shot of a local anesthesia. I couldn’t see it because I was lying on my stomach, so I don’t really know what they did, but I remember it just felt like hammering into my bone.
It was crazy. To this day, after everything I’ve been through, I still think of that as the most painful thing that I’ve done.
It would be interesting to see it happen, because I’m actually curious to see what that procedure looks like now that I have like a feeling of what it feels like.
I remember she was very apologetic. “Sorry! I’m so sorry I have to do this.” I remember they did it a couple times, and I was like, “Oh, my gosh, I can’t take this.”
She was like, “Okay, okay, it’s good enough. It’s good enough.” That was kind of the feeling. I asked them to stop.
Describe the CT and PET scans
Next was a CT scan and then a PET scan. I did those scans, and then there was a needle biopsy, which was inconclusive, but the CT scan and the PET scan confirmed that there was an issue.
The chest X-ray was outside of Stanford, but after that, I was referred to Stanford. I think then they ordered the CT and PET scans for their own purposes and information gathering.
I remember having to wait in a waiting room, and then a nurse came to start an IV. At that time, starting an IV was no big deal. As treatment went on, it became harder and harder for nurses to find good veins.
I have really small veins. I started learning tricks, like if I’m given a heat pack, my veins will pop out.
I started advocating for myself more because nurses were poking me 2 or 3 times, or poking me and then trying to move the needle to find the vein.
It was with contrast dye, so they had to start an IV in me. I remember waiting for quite some time at that center.
I just remember when the contrast goes in, it feels like you need to pee. Your whole body’s kind of tingly.
The PET and CT scans themselves were pretty fast. I’d say like 20 to 30 minutes total.
Describe the surgical biopsy
I remember I had to go under. There was as pre-op area, where I had to wait a long time. I think this was the first time that I remember feeling sad or feeling alone. I think several factors caused me to do that.
One was it was at nighttime. It was just a whirlwind of tests. We knew something was wrong. We knew it was likely cancer. We knew also that most likely I would be okay; it wasn’t a cancer that would kill me.

I remember they said 90% of these cases are not just in remission, but you’re cured. We knew all this, but it was just a whirlwind of, “Okay, we need to do this test, this test, this test.”
Waiting for the surgery, I remember feeling, “Oh, shit, what’s happening to me?” I was just quiet because it was just me. I was waiting to go into the operating room.
I remember thinking, “Oh, this is cool, Stanford.” They gave me an iPad to play on. I didn’t have my phone with me, and I remember thinking it was cool.
Stanford’s so fancy that they have iPads that you can use while you’re waiting to go into the operating room! Funny little thing to remember.
They had a breathing tube in me, too, so my throat was really sore. Those were the 2 things that I remember. It’s been like that every time I have surgery, too.
Scanxiety: waiting for results
I’m the kind of person who hates waiting, not just for something as big as this, but just in general. I wouldn’t classify myself as a patient person.
I dealt with it by looking online. I just thought, “Oh, maybe I can find out by Googling my symptoms or looking at forums.” What do most people do, or what happens to most people with these words that I’ve heard?
Talking to doctors, it’s like a new language you learn. I remember thinking I don’t know what these words mean, but I had to learn them, and all of a sudden it became this language that I spoke.
I think I did a lot of passing the time waiting by doing research online, which I don’t really recommend. But it made me feel empowered to get as much information as I could.
»MORE: Dealing with scanxiety and waiting for results
Chemotherapy
What chemo regimen did you undergo?
I had 2 choices. The standard procedure was called ABVD chemotherapy, and an alternative that was presented to me was the Stanford V regimen.
I remember that they told me that they both have kind of the same success rate, and either way I’d have to get radiation after chemo since my tumor was so big.
I ended up choosing the Stanford V regimen because it was more condensed. It was weekly treatment packed into 3 months, whereas the ABVD was biweekly treatments over the span of 6 months.
Either way I had to have radiation, and I wasn’t working at the time, so I was like, “I’d like to get this over as soon as possible.” I just chose Stanford V because it was more condensed.
Describe the Stanford V regimen
12 treatments over 12 weeks. Once a week.
The way Stanford V works is you don’t get the same drugs every week. I think it was a 2- or 3-week rotation. Depending on where in the rotation I was, I would either get 1 infusion or 2-3 different infusions.
Most of them were just through the IV. I do know there was one that was given through a syringe, a red one. Vincristine.
Generally speaking, I think treatments took the better part of a day, at least 5 hours. It was pretty comfortable at Stanford. I would just sit in a chair, and they would hook me up.
They had TVs on the chairs. For the most part, I was awake for most of the day. Sometimes I’d take a nap or read.
I also would have to do lab work before. Every time I showed up for chemo, I would go to lab, get my blood drawn. I would see my oncologist, who would check my white blood cell count. Then if it was okay, I would go upstairs to get the chemo.
There was one time during my second or third week where my blood count was too low, so then they started me on Neupogen and then sent me back to get chemo the next day.
How was the infusion process?
What really triggered it for me was when they start your IV, they have to flush it with saline. When they push it through the syringe to make sure your line is clear, I’d taste the metallic taste.
For some reason, when saline drips through the IV, I don’t taste it, but when it’s pushed through the syringe, I taste it. That became this mental association for me with chemo and being sick.
I remember that would trigger this nauseous feeling, and I would kind of gag, especially later on during the last few weeks of my treatment. It was really hard.
Also, the Coban [tape] that they used to wrap your [arm] whenever they draw blood, that smell would somehow trigger nausea, too.
Once I knew that, I would ask them, “Okay, I know you have to flush my IV, but when you do it, can you use as little as possible? Don’t push the whole through it?”
Sometimes, if the nurse is really nice, we’ll draw some out of the saline bag for the IV, and they’ll use that to flush. Or instead of using Coban to wrap my arm, they’ll use a band-aid or paper tape.
I learned to start asking for things that would help me.
Describe the chemo side effects
- Fatigue
- Slight nausea
- Constipation
- Mouth sores
- Food aversions
I would say 2 to 3 days after, I’d be pretty tired. I would kind of sleep the whole day. The next day, I would be back to normal for the most part.
I had aversions to food. Food I normally really liked, I could not stand the smell of or would make me feel kind of queasy. I remember really enjoying tomatoes with all of our lasagna, or tomato sauce stuff.
One of our family friends bought an ice cream cake from Cold Stone. I remember devouring that. Just weird food, not cravings, but just things that didn’t normally appeal to me would appeal to me.
I lived at home at that time, so my mom had to stop cooking food when I was there. Or she’d have to cook it and then put it away right away.
What helped with the side effects?
- Anti-nausea: Zofran
- Constipation: stool softeners, Colace
- Mouth sores: special mouthwash and toothpaste
We had just as many side effect medications. I had medications I was taking to stay ahead of the nausea, like Zofran, things like that.
I remember my nurse practitioner telling me it’s a lot easier to stay ahead of the nausea than to feel nauseous and then try to take medication to combat it. I took that to heart, and I really religiously took the anti-nausea medications.
But then with that came constipation, and I did have trouble with that. So I had other medications like stool softeners to deal with that.
I also had some dry mouth or mouth sores, so I had a mouthwash I used to help with that and a special toothpaste I used for that. But I don’t actually remember that bothering me too much. I think it did come up a little bit, but it didn’t hold me back. It didn’t make me feel terrible or anything.
I had to have Colace. It wasn’t prescription stool softener; it was just drugstore stool softeners. I don’t think it worked because I still had problems. I ended up having a liquid fiber kind of thing that I would dissolve in water and then drink it. It was nasty, but it worked.
»MORE: Cancer patients share their treatment side effects
How was the Neupogen shot?
The first time I got it, I remember it hurt a lot. Then my nurse told me, “Next time, take Claritin before you get the Neupogen.” Ever since then, I did that, and it helped so much.
How many scans did you undergo during chemotherapy?
They did a scan halfway through my treatment, and then they did one at the end as well.
For the midway PET scan, the mass had shrunk down from 12 centimeters to 3 centimeters. The post-chemo scan came back negative, so everything was good.
Radiation
You underwent radiation after chemo
I think they were saying it was because there could be traces that don’t show up on the scan, and I understood it as just to be safe.
I think it was part of the regimen. Just to complete it, I had to do 20 days of radiation every Monday through Friday. Every day.
Describe the radiation
It was super easy. I had to go in at first to get fitted for something. They put this cage over my head because the target area was in my chest, so I had to get a mold of my face, my neck and upper chest area.
I remember they made this cage that would fit my body. Then they used that to keep me in the right position each time and to make sure I’m lined up with the lasers each time.
I also had to get one tiny tattoo, a dot that looks like a freckle. I think they used that to help make sure everything was lined up correctly. It’s on my chest, in between my boobs.
It’s a tiny dot. It literally looks like a freckle. You can’t even see it. I remember the tattoo was just like a pin prick. One tiny second.
Once that was set up, every day when I went in for radiation, they would put the mask on me, which would then help me get in the right position.
I was lying on my back. There were these machines that would radiate me. I don’t remember seeing any lights.
Were there any radiation side effects?
It was super quick. I remember they told me that my skin might get a little bit dry or start peeling like I have a sunburn, so just to keep it moisturized.
I didn’t actually have any problems with that at all. It was super quick. It didn’t feel like anything.
Compared to chemo, it was just in and out, 30 minutes each time. It was super fast, super easy.
»MORE: Read other patient experiences with radiation therapy
What was the follow-up procedure after chemo and radiation?
I had to visit my oncologist once every 3 months for maybe 3 years. Then I had to see them once every 3 months. Each time they did a blood test.
I think at first it was once every 6 months I did a PET scan for the first year after, then one a year.

Quality of Life
Describe the hair loss
I remember my first treatment, nothing really happened with my hair. I think 3 weeks, in my hair started falling out, just a little bit at a time.
Then I remember it got to point where it was just getting everywhere all around me — on my pillow, on my clothes. It was really more irritating than anything else.
I have a scar on my neck from the biopsy. They cut me open there. I was sore in that area. That was my first time going under anesthesia. I learned from that that I get very nauseous after anesthesia.
I ended up having my boyfriend at the time, now husband, take the clippers. We shaved it so that I had a buzz cut. It was just nice not to have to worry, ‘When’s my hair going to fall out? How weird do I look?’
And all that comes with it. Going back to my need for control, it gave me control of something. I’m going to decide when my hair comes out right now.
What helped with the shaved head?
It ended up not being as traumatic as I thought it was going to be. To shave my head, that is. Throughout treatment, I ended up getting a free wig from the Leukemia and Lymphoma Society at one of their centers, but it didn’t really suit my style.
I ended up ordering wigs online and getting 2 wigs. I got a long one, and then I got one that was half a wig. It has the bangs and the bottom part, and I would wear the beanie over it. That one ended up being a lot more comfortable.
Through chemo, I was never confident. I always saw women rocking a wrap or a scarf or just even nothing. I remember thinking, “Wow. They still look so feminine, even though they don’t have long hair,” which I never expected.
But I never had the confidence or the courage to do that. I always went out with a wig on. I think during treatment, it wasn’t hard for me. The reality was I had cancer, and I was getting treatment.
I think the hard part was how long it takes your hair to grow back after and how even though I was done with treatment — my cancer was gone, the scan showed I was healthy — when I looked in the mirror, I still didn’t look like myself. I think that was the hardest part.
»MORE: Dealing with hair loss during cancer treatment
What was the worst part of treatment?
For me, my personality and who I am as a person, I think losing control was the hardest part. Definitely. That was a hard thing because all my time was consumed by chemo and cancer.
The only time I really went out of the house was to either go get chemo, go to a doctor’s appointment to go get images, or whatever.
For 3 months of my life, everything revolved around cancer.
I didn’t drive myself to my own appointments. I was never alone really. Sometimes, yes, I would be getting chemo, and my mom would go downstairs to the cafeteria. It was always me and my caretaker.
At the time, I didn’t realize it bothered me so much, but looking back, I really felt like I was so young. I just finished grad school. I was just about to start getting my adult life going.
I think it was a huge blow to me to not have any control of my health, of where I was going, of how I spent my time, things like that.
What helped you get through those tough times?
I think just looking forward. Counting down. “Okay. Now I’m two-thirds of the way down on treatment. Now I only have 2 weeks left to go.”
Just knowing that each week it was moving forward, and of course, I’m sure getting positive results from the scan helps, too. Just knowing that it’s working helps.
But I felt like, ‘What other choice do I have? I have to keep moving forward, and each day that passes, I’m one day closer to the end.’
I had so much support, too. My friends really rallied. They sent me nice things. I think it was a huge shock for them, too. It was the first time, for a lot of us, that someone so young could be diagnosed.
We hear about cases all the time. Like, “Oh, our grandparents have cancer,” or “So-and-so feels bad because his dad had cancer in high school.”
But it was the first time for my friend group that it was so close to them. They really rallied. They sent me letters. It was really sweet. I appreciated it. It helped me definitely through hard times, too.
But I will say, I definitely also felt like, “Well, you guys don’t really get it, either.” Which is not meant to take away from their concern, their support and their love, because I definitely felt that. But ultimately, I did feel like I’m the one who has to go through this.
Finding your cancer community
I looked up recommendations where there was young adult cancer survivors. I tried to look for blogs of people who had been through this experience.
I remember finding one blog where this woman had posted, “Week by week, my hair grows back to normal.” That kind of thing. It helped me to see like, “Oh, 12 weeks out of treatment, this is what her hair looked like.” Or, “She stopped wearing a wig 16 weeks out of treatment.”
It helped me to see that. Also, I remember looking up organizations. I remember just Googling “young adults,” “cancer,” “lymphoma” to see if there were people I could relate to.
Any big surprises during treatment?
Physically, it wasn’t easy, I remember. But it wasn’t as bad as media and movies and TV shows portray it to be.
I was really lucky, but I was never bent over the toilet trying to vomit or feeling like I need to vomit. I didn’t really have that kind of feeling. That was what I thought it was going to be like, because a lot of times that’s how it’s portrayed in media.
“Be your own advocate”
The medical experts have a lot of scientific and medical knowledge. I don’t discount that at all, but I think ultimately we know our bodies best. I think for big picture treatment things, it’s good to have their guidance.
But in terms of how to make yourself feel comfortable or advocating for yourself, I think really no one is going to advocate for yourself more than you are.
» MORE: How to Be Your Own Advocate

Tips on whether someone can work while undergoing Stanford V regimen
With this regimen, I don’t think so because you’re going in every week. You don’t have enough time to really recover in between. If you’re working at home, maybe.
I guess it depends on your job. I’m a teacher, so there would have been no way for me to come into the classroom in between treatments.
Advice on how to get the right support?
I think the most helpful thing for my friends was when I could hang out with them and not talk about cancer.
I totally get it. They want to help. They want to know how things are going. But my treatment started in September and ended in December.
I remember there was one time when a bunch of people were home for Thanksgiving, and I remember feeling it was so nice to hang out and see friends and just hang out.
They were home in town for Thanksgiving, and we all met up. It was just nice. It was like old times.
Every other conversation, I remember starting with, “How are you doing? How are you feeling? How are the treatments?”
I get it. People are coming from a place of concern, of love, of support. But it was nice just to be able to forget about that for a little bit.
Even after treatments were over, a lot of conversations began with, “How is your health?” Sometimes friends who I haven’t seen for a long time were out of concern asking, “Is everything good with your health?”
I get it, and I understand it. But it was important to me that cancer didn’t label me. I don’t want to be the thing people think of when they think of me.
Message to patients and caregivers now dealing with cancer
I want to tell them what that doctor told me. Of all cancers you had to get, this is probably the better one because it’s so well researched. It’s so curable.
It’s going to be hard. It’s going to be a disruption to your life, but it’s not going to be life-ending. That, for me, was such an important message for me to hold onto through all this.
No matter how alone I felt or how much I was like, “Oh, this sucks.” At least I didn’t have something that was more life-threatening.
It was never a question of, ‘Will I survive this?’ It’s just, ‘When will this be over?’

Inspired by Stephanie's story?
Share your story, too!
Hodgkin’s Lymphoma Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)