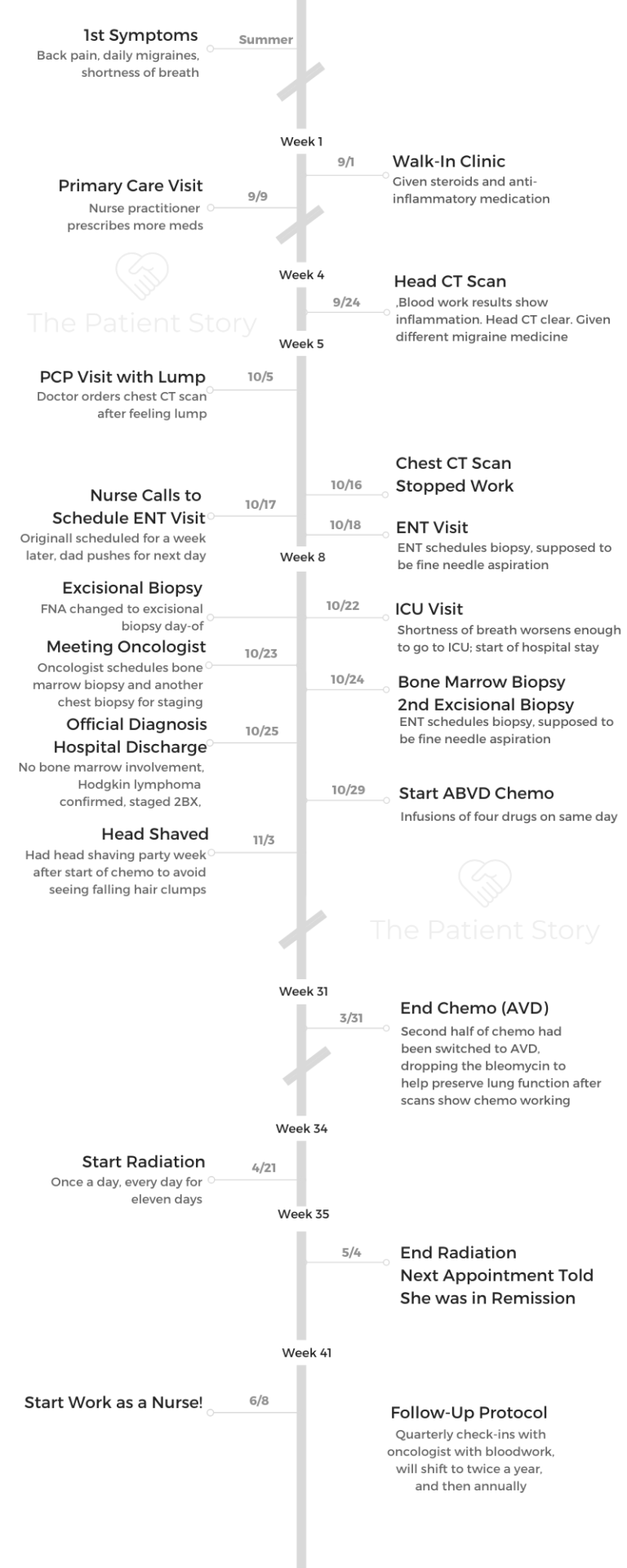
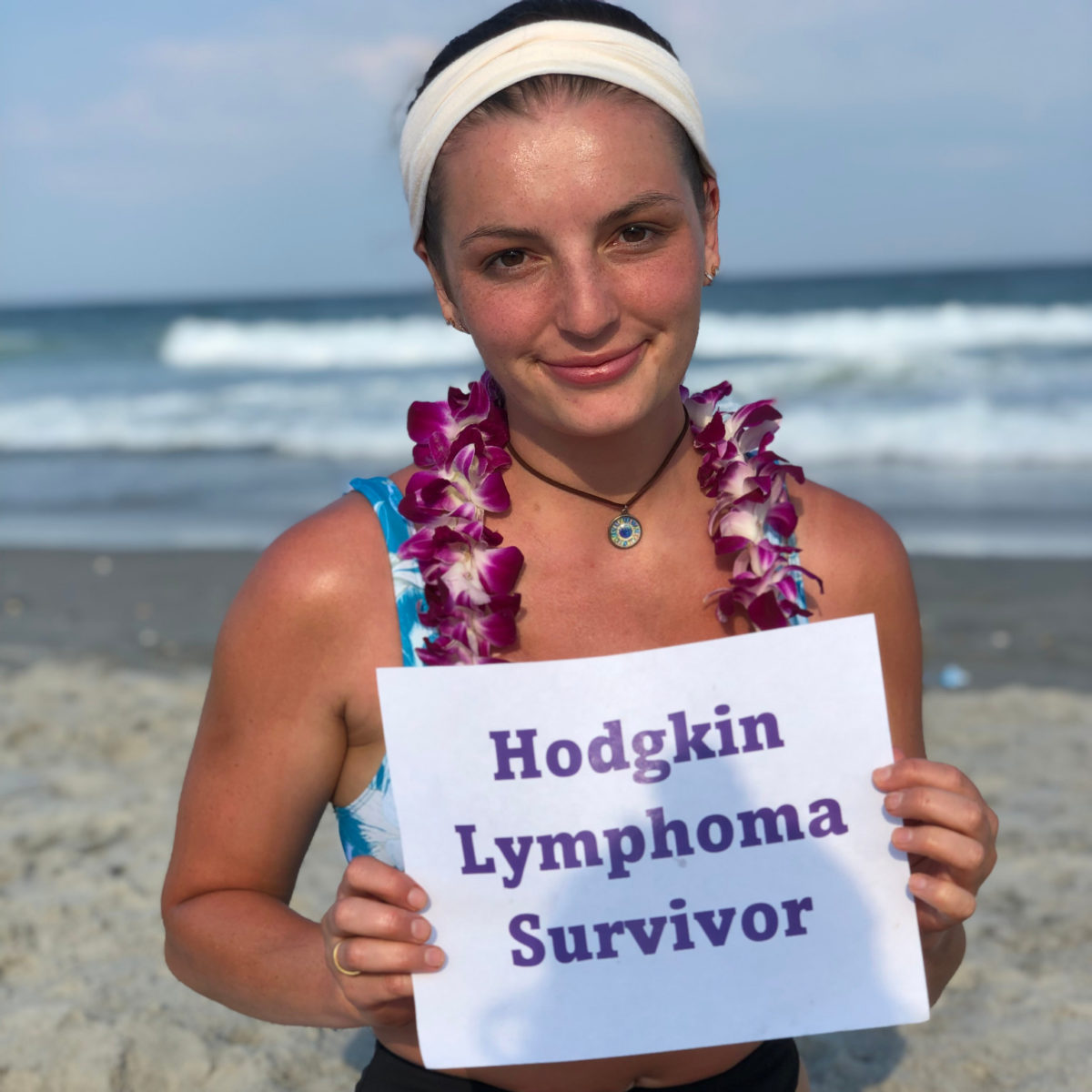
Mara’s Stage 2BX Classical Hodgkin’s Lymphoma Story
Mara shares her stage 2BX Hodgkin’s lymphoma story, which includes undergoing ABVD chemo, taking out the bleomycin (AVD), undergoing radiation, and also going through IVF to preserve her fertility options.

- Name: Mara T.
- Age when diagnosed: 21
- Diagnosis:
- Hodgkin’s lymphoma
- Stage 2BX (bulky)
- 1st Symptoms:
- Shortness of breath
- Back pain
- Daily migraines
- Tests & Biopsies:
- Chest CT scan
- Excisional biopsy
- Bone marrow biopsy
- PET scans
- Pulmonary function test (lungs)
- Blood work before every treatment
- Treatment:
- ABVD Chemotherapy Regimen
- 3 cycles
- Each cycle = 1 month, biweekly
- Total: 6 infusions
- AVD Chemotherapy
- Dropped bleomycin to preserve lung function after scan showed chemo was helping
- 3 cycles
- Radiation
- 11 days or sessions
- ABVD Chemotherapy Regimen
- Egg-freezing:
- Decided not to freeze eggs to avoid one more medical procedure
- Diagnosis
- What were your 1st symptoms?
- Going checked out at the walk-in clinic
- Going to the doctor's
- When did you find a lump?
- Scheduling a chest CT scan
- How did you pass time waiting for tests and results?
- Describe the CT scan
- CT scan contrast dye warning
- Describe the results call the next day
- Digesting news of the mass
- Getting an earlier appointment (self-advocacy)
- Describe the ENT visit
- What was the biopsy like?
- Tips on getting the biopsy
- Going to the ER
- Roller coaster of optimism and reality
- Preparing for Treatment
- ABVD Chemotherapy
- Radiation
- Reflections
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Just take care of yourself. It’s okay to cry. It’s okay to hate your life. You don’t have to be an influencer. You don’t have to make it an amazing, beautiful thing. If you want to, that’s fine.
I wrote in journals things I was thankful for sometimes, but I also wrote journals about ‘Wow, this week really just took it out of me.’
Do what is best for you during this time because you’re literally fighting for your life.
Mara T.

Diagnosis
What were your 1st symptoms?
My whole life I’ve had tiny, little headaches, but no real migraines. Last summer I started getting migraines daily, where it felt like something had popped inside of my head. I’d get lightheaded.
I was having back pain in my middle of the back when I sat in certain positions and a little bit of shortness of breath. I was always anemic, so my fatigue wasn’t new, but it definitely got worse.
After that, I went to my doctor, and everything was normal with the labs except for one result. I had a lump up here on my shoulder, my clavicle area, so he did a CT.
Going checked out at the walk-in clinic
I went to the walk-in clinic on September 1st, the day before my 1-year wedding anniversary. They gave me steroids and an injection of an anti-inflammatory medicine.
That obviously didn’t fix anything, though, considering the migraines were from compression of my superior vena cava by the tumor growing in my chest.
Going to the doctor’s
The next week, I went to my primary care doctor’s office. His nurse practitioner prescribed some meds to “reset” my body. Her hope was to knock me out for the day and then have me wake up feeling better, almost like turning me off and then turning me back on again.
She also gave me a medicine to take when I felt a migraine coming on. That medicine made me feel like I was having a stroke. I was so confused and out of it.
I went back to the doctor on the 24th, and they ran some blood test that showed that my ESR was high, which is a non-specific marker of inflammation.
When did you find a lump?
My friend and I were studying for nursing school, and she came over. She was like, “I have this lump that comes up on my shoulder that comes up whenever I get stressed out.”
I was like, “Rachel, that’s so gross.” I was teasing her. I reached up and felt mine. I was like, “I do have a lump there.” I texted my mom and asked, “What do I do?”
She said to wait 2 weeks because the lymph nodes swell all the time for no reason, and then you can see the doctor. So I waited the 2 weeks and called him. He saw me pretty quickly — if not that day, then the next day.
He felt it, and his whole face dropped.
Scheduling a chest CT scan
He went from being the friendly, regular doctor to seeming bummed about it. He knows my family since my family is medical. I don’t know if that made a difference to him, or if it was because I was young and he knew. It still sticks with me that I can see his face. He had to not say anything to let me onto it, but I knew.
I had had a head CT already, but he ordered a chest CT after that because Hodgkin’s presents with that huge mass in your chest usually. And it was there.
He couldn’t get me in for a CT scan until October 16th, so the next 11 days were excruciating.

My head CT was the same day maybe, but the chest CT was so far out. It was nerve-wracking to wait that long, but I was like, “If it’s that big of a deal, it would be done quickly.”
My husband and I were housesitting a week before that happened. I joked with him. I had been getting those migraines for so long. I was like, “What if this is the last normal weekend to get away?”
He was like, “Don’t say stuff like that. You’re just being dramatic.”
But it was.
How did you pass time waiting for tests and results?
The waiting is always the hardest part.
I would not repeat that weekend between knowing and chemo for all the money in the world. I would rather do chemo over and over again than do that weekend of waiting.
My biggest thing was trying to live a normal life because I knew things were going to change. My husband and I went to the zoo, which isn’t an option right now with there being a global pandemic. But we went to the zoo, and I got out of breath. I knew that was from the cancer.
It was nice to have that memory of normalcy hanging out with my family. I got to be normal for a bit. That was my last bit of real normalcy. On my off-weeks from chemo, I felt okay, but I still wasn’t able to go to the zoo or do normal people things.
Describe the CT scan
For the CT scan, they start an IV. They can do it with or without contrast; mine was with. They start an IV. They have you lie on a table. You go through a short tunnel — more like a donut than a tunnel. They do the contrast through your IV, doing it slowly so it goes through right at the perfect tunnel.
You’re in and out in like 5 or 10 minutes. It’s super fast and easy.
CT scan contrast dye warning
It makes you feel like you peed on yourself, but I knew that was coming because my techs told me.
Describe the results call the next day
I was on my way home from nursing school, and my friend was riding with me. I still didn’t think anything was wrong-wrong. I was driving, and I got the call.
I’d been waiting all day. I had to call them for results because they were trying to figure out what to do.
I got the call and answered it over the car speaker. She was like, “We have a follow-up with an ENT for you.”
I was like, “Oh, okay. What did my scan results say?”
She was like, “Well, actually we found a 7-centimeter mediastinal mass.”
I was like, “Hmm. What does that mean exactly?”
I started crying while I was driving down the most dangerous road around here. My friend sat there, and he was like, “It’ll probably be fine.” He did not know what to do.
I dropped him off, and I did not speak to him. I went straight home and called my mom, who was on a work call.
I told her they found a lump, and she said, “Oh, that’s not good.”
Digesting news of the mass
At 7 centimeters, we didn’t really know how big that was. We don’t use the metric system or anything. When my dad got here — we met at my house — I was like, “How big is 7 centimeters?” He was speechless at that point, so he just showed me his fist.
I was like, “Wait, what part of the fist are you talking about? Diagonal? What is happening there?” So we joke about that. He just kept doing the same thing over and over again.

Getting an earlier appointment (self-advocacy)
My appointment was supposed to be the next week, but my dad freaked out and pulled some strings. I understand the scheduling restrictions. We had to go very early in the morning.
I don’t know if it was that pressing of a matter (it doesn’t move that quickly), but it was the waiting that we didn’t want to do because it was so hard to wait.
Describe the ENT visit
Between getting my scan results, I got a paper copy. It said ‘likely lymphoma,’ and that’s when I was like, ‘Oh, this is really happening.’
I had done a lot of research of people who had the similar lymph node, the supraclavicular one, and the mass in my chest. Almost every single person had lymphoma.
So we know, and we go there. He said, “We can biopsy the one in your shoulder. That’s not a big deal.” I was like, “Do you think it’s Hodgkin lymphoma?” He said he wasn’t sure, but I think he knew.
He was super casual about everything, like it wasn’t the day of my cancer diagnosis. My appointment was Friday. He scheduled me for the next Tuesday to do my biopsy.
What was the biopsy like?
I had a really weird experience. Not everybody does this. I was supposed to get a fine needle aspiration, which is when they ultrasound it and stick it in there to get a tiny little chunk. But I got there, got changed, went to see the surgeon, and I said bye to my parents.
He’s like. “I’ve reviewed your film, and I think I can get a biopsy of your chest. Have you eaten today?”
I was like, “Yeah, I ate. I’m not going to pass out during the test. You didn’t tell me I couldn’t eat because of the fine needle aspiration.” He was like, “Okay, we’ll just heavily numb you.”
So I had chest surgery while wide awake, where they numbed up my chest really well. They stuck some decently sized needles into my chest. I still have 1 or 2 scars from it.
It didn’t hurt at all. I just felt pressure sometimes.
Whenever they took a sample, it punched, because it was a punch biopsy. He went in 1 time and got 5 or 6 samples, because it’s hard to diagnose Hodgkin’s without a full excisional biopsy.
He had to get a bunch of samples, and the pathologist was looking at them as he was getting them. He tried to pull that needle-side out, and it squirted blood. He was like, “Oh, I think we’ve hit an artery, but it’s fine and not a big deal.”
He just stuck it back in and waited for it to cool back down. Then they did another one on the other side, going in a different angle, and got a bunch of samples from that.
It turned out those samples weren’t enough. However, the preliminary report did say it was probably Hodgkin. They just didn’t have enough to prove it.
Tips on getting the biopsy
A lot of people say not to do the fine needle biopsy. If you’re going to do it, do the full excisional biopsy because if they see anything sketchy in there, they’ll make you do the excisional biopsy anyway. So if your doctor will do it, it’s going to hurt, but it’s not going to hurt anything.
Going to the ER
I went to small group that night with my husband, and I kept yawning, but it felt like I couldn’t get a good yawn in. I felt like my chest was not doing the work of breathing.
With him having nicked that artery earlier in the day, my parents said, “We should go to the ER. We don’t know what’s going on in there, if you’re bleeding or something else is happening.”
I got to the ER, and I was crying because I couldn’t breathe. My husband was driving me there, and he’s not medical at all. I got there, and I was like, “I can’t breathe. I have cancer, but I can’t know for sure that I have cancer.”

It was really confusing. They thought it was just an anxiety attack because of everything going on in my life. But then they did a CT scan, and it showed bilateral pulmonary embolisms, so I had blood clots in my lungs.
At the moment, I was really optimistic about everything. I was like, ‘I can do this. I’m tough! Cancer doesn’t have anything on me.’
Then reality hit, and cancer actually has a lot on me. I was humbled very quickly.
Roller coaster of optimism and reality
In the beginning, I posted this Instagram post, “Everything is going to be fine. This is the ‘good’ cancer.” That’s a load of BS. It’s not the “good cancer.”
There’s no such thing as a good cancer.
I was super optimistic there, saying, “I’m going to ICU, but I’ll be fine.” Then ICU delirium kicked in, where I got no sleep and there was beeping all the time.
The next week at chemo, I had an anaphylactic reaction to one of the pre-meds. I didn’t even get to start chemo before I tried to die again. It was just constant kicks to the shin, over and over again. You think you’re doing fine, and then it’s bam, you’re not doing fine anymore.
Every week, I’d be like, “It’s going to be fine. I’m going to do this differently this week and this differently next week.” But chemo is just designed to suck.
»MORE: Processing a cancer diagnosis
Preparing for Treatment
Describe meeting the oncologist
They usually don’t [meet the patients next day], but since I had the preliminary results, they called him and said, “Do you want to meet her?” He said yes.
We heard he was an early rounder. He came in at 5 in the morning. We had just gotten to sleep because I was on blood thinners, and they were checking levels all night.
He comes in and is super casual, swearing a ton. He’s young and funny. We loved him instantly.
My family was in shambles at that point, but every time we meet with him, we feel better about the situation because he’s so casual about it. He’s confident in what he’s doing; he had a plan in place. I know it’s his job, but it’s comforting to have someone with good bedside manner who makes you feel like everything’s going to be okay when you have no idea what’s going to happen in life.
You’re trusting someone to put these intense chemicals into your body — and to do it and for it to be worth it, because if I did it all and it wasn’t worth it, that would not be good.

Describe the bone marrow biopsy
This is one time I got to be a patient advocate for myself. This doesn’t happen to most people.
I got to the biopsy. They laid me on my belly, pulled me over to a table, and gave me Benadryl and a little bit of Versed, I think. They were going to put me all the way to sleep since they were going to do a chest and bone marrow.
But I didn’t go all the way to sleep, and they started doing things. I could feel them pushing down on my hips and moving me around. I wasn’t all the way sedated and so confused because I was kind of sedated, so I was really out of it because I was so high. They were doing these things and told me I’d be asleep. I wasn’t asleep, so I was crying. I was like, “Why am I not asleep?”
Everyone was just walking around me, doing their jobs. They probably thought I wasn’t going to remember any of it, but it’s still stuck in my head. Then they were like, “Why is she not asleep?” So they gave me more meds, and I went to sleep instantly.
Port placement
The whole time I was in the hospital, I had IVs in my forearm. Every time I would move my arm, the IV pump would start beeping and hollering, so it was not easy to sleep.
They were like, “We’ll get you a port.” They kept pushing it back every day, and I still had these terrible IVs in my arm. They couldn’t place them because I was so dehydrated. Every day was like, “You’re getting the port. Oh, you’re not getting it.”
The last day, I got my port really late in the day. I was still high when I came back. Then they said, “Okay you’re going home.” My best friend was working. She was like, “I’ll pull your IVs out.” I thanked her.
She was pulling them out, and the tape was pulling my arm hair because I still had arm hair at that point. I was like, “Rachel, you’re so bad at this!” She was such a good sport. She said, “You’re fine. You’re funny.” I was so high. Then I fell asleep instantly. I had weird dreams; it was all over the place. That was a fun sedation experience!

When did you get the full diagnosis?
That was during the (hospital) stay. The doctor came back and said, “Yes, that looks like Hodgkin lymphoma. This is our plan.” But it wasn’t an exact turning point because there was some gray area in there.
The staging was part of the bone marrow biopsy. They didn’t do a PET scan because as long as it wasn’t in my bone marrow, it wouldn’t change the treatment plan at all. So they did the CT scan.
They diagnosed me as stage 2B, and it was bulky because for the size of my chest, 7 centimeters is a lot.
Oncologist description of treatment plan
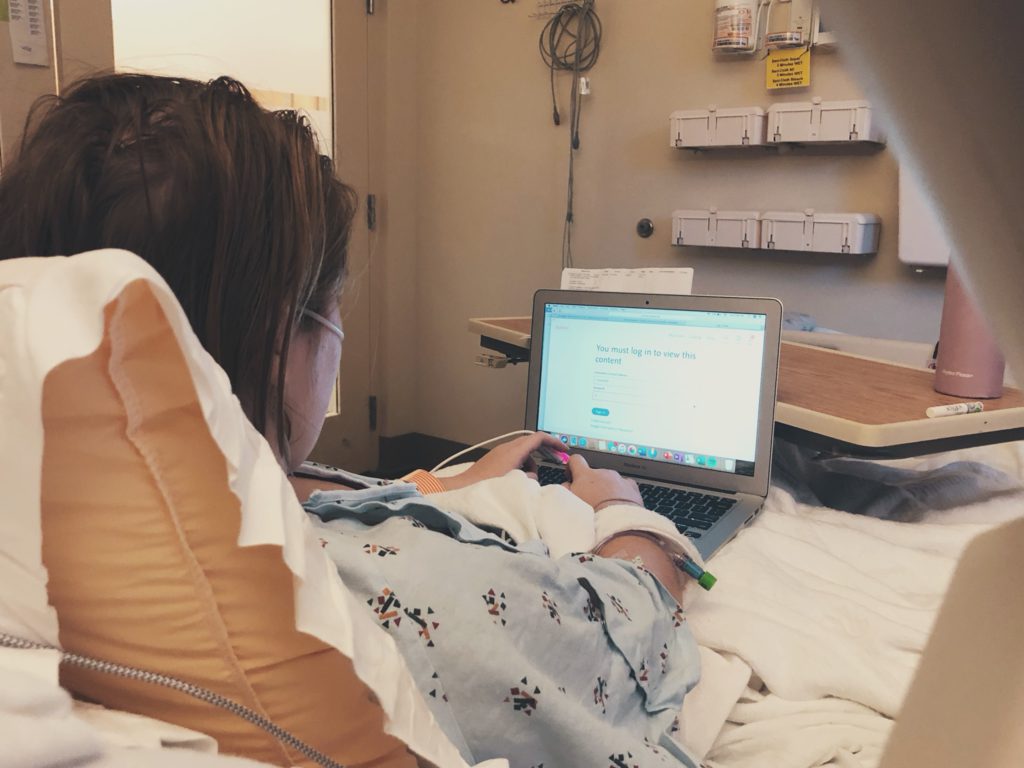
I don’t really remember because I was so sleep deprived at that point. My mom and I had done a lot of research during the down time in the ICU of what we’d expect to do.
As long as there’s not real lung involvement, they usually do ABVD chemotherapy. We weren’t sure if they would do the “B” or not, since I’d had the pulmonary embolisms. But we ended up doing ABVD, and we trusted him with everything in us.
He said we’d do 4 treatments of ABVD, do a PET scan, make sure it’s reacting, then drop the B so I wouldn’t have long-standing lung issues.
Talk of fertility preservation
My husband and I never wanted to have kids. The doctor said they would use Lupron before the first chemotherapy, and I said, “No, I don’t want to do an extra medicine for children I don’t want to have — especially with the chemo. I don’t know what it’s going to do to me.
A lot of people still have kids, and it’s not a big deal at all. I always felt if I could change my mind, I could adopt, and I didn’t want to put my body through that. So it wasn’t a worry for me at all.
»MORE: Fertility preservation and cancer treatment
ABVD Chemotherapy
Accessing your port for chemo
I was nervous about getting my port accessed the first time, but they took me back and were like, “We’re going to access your port.” It happened so fast. I never got my port numbed the whole time. No shade to people who do, because I know needles are not fun. I used to give blood before I got sick, so I’m cool with needles.
It literally felt like nothing. There’s such a thin layer of skin between my port and the outside world that it was just, ‘Bam, you’re in. You’re good.’
The part that bothered me about the port access was the flush because I would taste the saline flush. It tasted like metal. That triggered all kinds of flashbacks for me.
Describe the chemo regimen
I did outpatient chemo. I got there first thing in the morning because I wanted to get it over with and sleep all day. I’d get there, do lab work, then meet with my oncologist every other time, so once a month.
Then he would talk to me, and I would go get the chemo. They would do all the pre-meds. The first time, I had that anaphylactic reaction, and my oncologist came running, which was very impressive. Doctors usually don’t run for things, so I was like, “We love you.” They gave me a lot of Benadryl.
I got my actual chemo. Getting chemo itself isn’t that bad. It’s all the time afterward. After that, it was pretty miserable for the rest of the day.
I don’t remember most Tuesdays. On Wednesdays, I’d be sort of out of it, which was good since I had class on Wednesdays for nursing school. I don’t remember a lot of the tests that I took, but I passed them!
It was all 4 drugs on Tuesdays. We’d get there 7:30 a.m., start labs then, and if we didn’t meet with my oncologist, we’d be out of there by 11:30 a.m.
The first time took a little longer since they pushed everything slower, just to test my body and see how it could do, and because of the reaction. On oncologist days, I’d probably leave there by 1 p.m. or 2 p.m.
I did it from the last week of October to March 31st. I never skipped anything. I didn’t have to be delayed or anything, so I did it as fast as possible. But it was still a long time.
I got the Neulasta, which injects a medicine that stimulates your white blood cell count. I never got neutropenic throughout my whole chemo. It was a win for sure.
»MORE: Read our comprehensive ABVD chemotherapy info page

ABVD side effects and what helped them
The day of, I’d get really nauseous. Part of it was the medicine I was allergic to was the anti-nausea medicine that was supposed to be really good for coverage.
So day of, I’d take Zofran every 4 hours and Phenergan. My mom stayed home with me on the days of chemo and would work from my house. She set a timer on her phone, was amazing, on top of it constantly.
I could not have done it without her. My husband set alarms all night. We’d get up at 4 a.m. for it. I took Zofran so much.
After the nausea, I don’t think I threw up, but maybe once or twice. It was a constant feeling of impending nausea. After the Neulasta went off, which was what stimulated the white blood cells, I would get really bad body aches. I felt like a walking bruise.
I would try to lay in the bathtub to make it feel better. My husband would have to pick me up out of the bathtub. He was really the MVP, too. My mom and him made everything amazing, along with my dad pulling all the strings.
The body aches went away. They gave me a painkiller for it, but I didn’t like the way it made me feel, so I didn’t take it. It was just sleepiness.
All that Zofran makes you constipated, so I had to take MiraLAX. I was super exhausted and wanted to sleep the whole time.
Describe the constipation
I texted one of my friends at 2 in the morning and said I might never go to the bathroom again. She was like, “You’re going to be fine.” She’s a nurse, too, so she was chill about everything. I was like, “This is the end of the world for me. I feel I might be dying right now!”
Tips on getting through chemo side effects
Once you go through one chemo week, you know what symptoms you’re going to have the next time unless they change something.
My mom kept track of what symptoms I had and when, so we could medicate for it beforehand. That made all the difference in the world. Knowing that you’re going to throw up is not really helpful.
If you’re going to throw up, the deed’s pretty much already done. So we wanted to keep ahead with the Zofran. My mom’s a nurse, so she’s pretty aware of those things. That helped a lot, too.
My biggest things were to listen to my body. I drank a lot of water. My mom had that on a timer, too, even though I would have to wake up to drink. That made me want to yell at people, but staying hydrated made a big difference.
I just listened to my body. I didn’t move when I didn’t feel like it because it didn’t make any difference in my outcome. It was living second by second for me at the time.
»MORE: Cancer patients share their treatment side effects
Describe the mid-chemo PET scan
Everybody does it differently. My doctor’s office was lax on restrictions, so I didn’t have to be carb-free the first day like a lot of people do. My thing was just no food or drink after midnight, except for a cup of water in the morning if you need to take medicine.
You got there and check in. They started an IV, and they inject radioactive glucose into you. That’s very scary when you don’t know what’s in it.
You chill out for an hour, and they wait for it to go through your system. I just laid there. Animal Crossing was out, so I played that while I waited. Then they make you go pee so you don’t have a lot of stuff happening in your bladder — so it doesn’t light up.
Then you lie on a table, and they take you through [something that’s] more of a tunnel than a donut. Then they pull you out, and it moves so slowly that you’re like, “Am I actually moving, or am I just sitting very still?”
You hear what sounds like a fan running. They slowly put you in, then you’re in it. They get whatever images they need, and you’re out of it all of a sudden. Then you’re like, “Okay, that was it, I guess.”
You have to wait, which is a horrible experience because you wonder, “What if there’s something really terrible I’m going to find out tomorrow?” Actually getting that scan done, you’re like, “It might actually be real.”

Handling the “scanxiety”
I actually didn’t handle the wait well at all. With my last scan, I went to the medical records office myself and got the results. I tried to fill the time, but there was always still that time running in the back of my head where it was like, “Okay, they should call soon.”
There were some times when my doctor’s appointment would be a couple days later, and I was like, ‘I’m not waiting for that doctor’s appointment. ‘
“You need to call me when you get those results. This is not a joke, not a drill.” I needed to know what’s happening because I was still having some of the symptoms. We knew it wasn’t reacting perfectly, and it wasn’t.
Avoid comparing scan results
You shouldn’t compare your cancer journeys to other people’s.
But a lot of my friends were getting clear scans by that point. Mine wasn’t clear; I had a Deauville score of 3. They said it was just because of the size of my tumor.
But they still dropped the bleomycin because it had gone down. It wasn’t actively growing anymore, so they dropped the bleomycin and let me go on with chemo.
It was disheartening to not get the results I wanted, because I wanted it to be over so badly. I was hoping when I went into that appointment that he would be like, “You’re doing so well! We’re going to drop a couple of rounds.”
Side effects during second half of chemo (AVD)
I think the nausea got a little better without the bleomycin, but it was still pretty killer. One less medicine is always a relief.
Radiation
What was the plan heading into radiation?
I didn’t get scanned after chemo before radiation, except a CT scan to determine where they would radiate me. That didn’t change my radiation plan at all.
We weren’t sure about radiation, but we met with the radiation oncologist. He was like, “Your odds of getting a second cancer from radiation this low is slim to none, and your odds of relapse are a lot higher without it.
I would rather risk a 1% change of a secondary cancer that I can monitor for than risk a much higher chance of relapsing with the same cancer and getting elevated chemo. I don’t want that at all.”
I finished chemo on March 31st and then started radiation at the end of April.
Describe the radiation therapy
I started on a Tuesday because they didn’t have an opening on that Monday. I went Tuesday through Friday, Monday through Friday the next week, then Monday and Tuesday the last week.
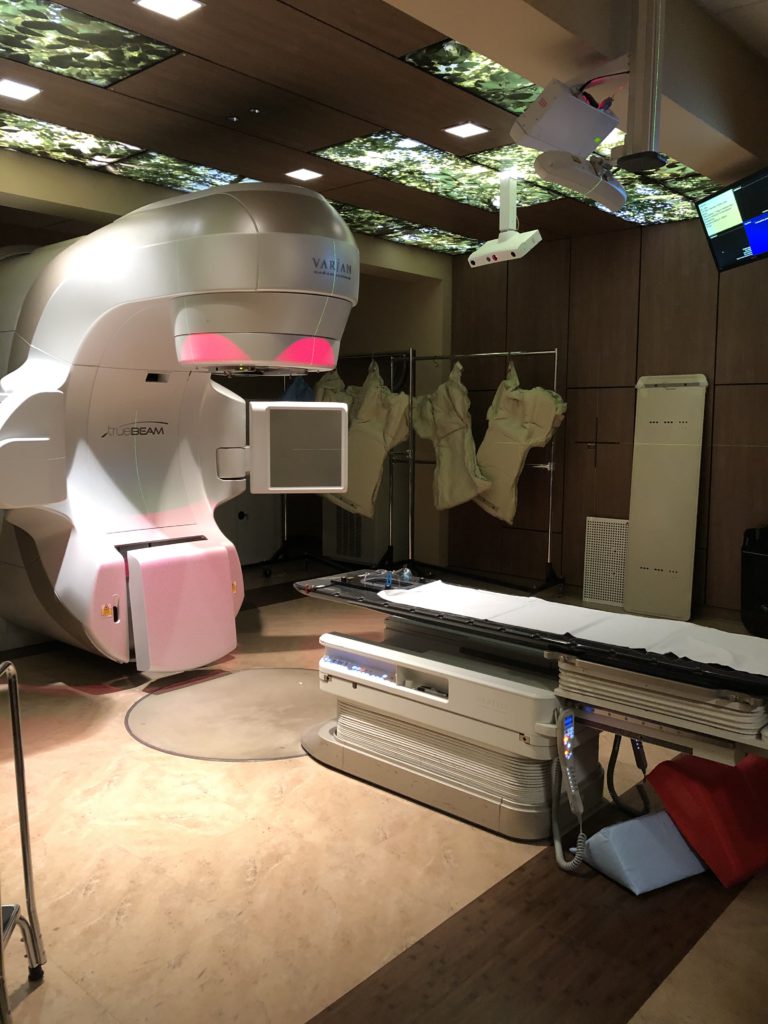
They had special parking for me, so I didn’t have to square up in the parking lot to get parking. I would go in, change into a gown, then go into the room where the radiation was. It was super fancy and futuristic.
They made me take my shirt off. They’d have 3D models of my chest up on the wall. They would ask me to breathe normally, then I’d have to hold my breath a couple of times so they could make sure they were getting the right part of the tumor.
It was about 15 minutes. It wasn’t bad at all. There was a big arm that comes across that tilts, turns, goes up, goes down, so it gets different angles.
They didn’t tattoo on me. They just put markers and stickers to hold it. That was nice, too.
Were there radiation side effects?
For radiation, I didn’t think it was that bad. It was just an inconvenience to go every day. But I didn’t have any side effects except for a bit of fatigue and a little bit of chest pain, maybe where the mass was going down.
Radiation was a cakewalk compared to chemo. I would do it over and over again to not have to do chemo.
Miscommunication and scare after radiation
I had another scan on June 9. It didn’t come back the way my oncologist wanted it to because he didn’t realize that I had radiation, so I got the scan done.
Then I didn’t hear anything from my oncologist. I knew he was out of town, and I was leaving messages at his office like, “Please answer me. I need answers.”
I went to Medical Records to get my own record. It said I still have a Deauville score of 2. The Deauville scale is 1 to 5. 1 is great; 5 is not good. I thought my chemo wasn’t working, that I’d have to get a stem cell transplant or something.
I get to the doctor’s office for my appointment, which is a week and a half later, which is a painfully long time, especially when I don’t know what’s happening. My oncologist is on time, which doesn’t happen for oncologists. He’s like, “When do you start radiation?” I told him I already did radiation.
He was like, “Are you kidding me? I presented your case to the tumor board this morning because I had thought you had relapsed. You still have activity from the radiation, but you don’t have an active tumor.”
I love him, though!
When did you officially learn you were in remission?
After that (at the same appointment), he felt so much better and said everything was fine. He has that chill personality where he just makes us feel better. My mom was Facetiming us because of COVID. My husband was there, but he works there with my dad.
My mom asked, “Is she in remission?” He said, “I guess you could say that.” So casual about it. My mom started crying. My dad started crying.
I was just sitting there feeling good I didn’t have to do any more chemo when I thought I had to.
Follow-up protocol
I’m not getting any more PET scans. I have a CT scan coming up and, if it doesn’t come back perfect, then I’ll get another PET scan.
Because I did have increased activity on the last one, they want to make sure the mass isn’t growing at all. As long as that’s okay, I’ll get my port out. Then I’ll only get CT scans if something comes up or if things aren’t perfect. They don’t want to give me more radiation.
I’ve had a million CTs and actual radiation, so it’s not that big of a deal. But they still want to keep it to a minimum. I’ll follow up with my doctor every year.
Reflections
Hair loss
I had a head shaving party pre-pandemic. All of my friends came over and all brought me hats. We had a bonfire. I had a photographer and a makeup person, who made me feel pretty, to shave my head. We went out to my parents’ backyard. They have a nice meadow.
We set up a mirror and stool. My husband shaved my head. Then my dad had to step in and help because my husband was leaving really long pieces randomly. I had rat tails sticking out all over me!
They took pictures that made me feel beautiful. You see the videos of people on Facebook shaving their head and crying. I teared up, but it made it more of a positive memory in my mind, as my last hurrah.




That was the week after I started my chemo, but I was not feeling it too badly yet because it builds up over time. My hair didn’t get a chance to really fall out. It definitely got a little thinner.
But I felt it was less traumatic to have a good experience with the head shave and not have it fall out in big clumps.
Some of my friends don’t lose their hair all the way, but I didn’t want to go through that. I’m glad I didn’t, because it didn’t fall out completely, but it got really thin. I don’t think that would have been very good for my self-confidence.
Plus, I feel like it’s a badge of honor with cancer. I did the whole experience. I did everything. It makes it easier not to have to wash hair, too, when you can’t move.
»MORE: Dealing with hair loss during cancer treatment
Keeping the humor
One time we were in the lobby. My appendix had shown up badly on my first scan because I had appendicitis. My oncologist came out to the lobby, where we were all sitting, and said, “You have the ugliest GD appendix I’ve ever seen!”
All the old people were like, “…?!” It was so funny because you have to know him to understand him. That’s just who he is. He’s funny. He’s like, “Your appendix looks like Megan Fox’s thumbs!” I was like, “I don’t know what that means, but okay.”
What was the support you needed most during treatment?
At first, I felt like a burden asking anyone for anything. But then I realized if it was one of my loved ones in that position, I would do literally anything for them, no matter whether I just sat down or something. You want to take care of people.
I would do it for a stranger, too. That’s why I’m a nurse.
I had to learn there’s no trophy for doing it without asking for help. There’s no reward at the end for ‘I did this on my own.’
There’s nothing in that. You can make your experience a lot better just by asking for a little bit of help.

People from my dad’s work would bring Chick-Fil-A over, and that would make a huge difference. My mom staying here and my husband being so willing to get up all night really changed things, because I don’t think I could have functioned without my mom being here all day. It sucks so bad.
She was on top of everything. She made sure I was hydrated, as much as we fought over that. She set timers on her phone. She knew what to expect every time, too.
Whenever she would leave, my husband would take over. They were really the OGs there. My dad, all the time, would make me food I liked. If I was craving barbeque or something, he would smoke some barbeque for me.
He would text me every day and tell me he loved me. He took it very hard emotionally, but he’s recovered somewhat now.
How did cancer impact your relationships?
My dad was always a good ol’ country boy. When I got diagnosed, I remember I got my scan results back. I wasn’t technically diagnosed yet, but we knew.
I know he cried a lot. He cried on my front yard, and then when I was in ICU the next week, he kind of got it together a little more. But he was sitting there beside me, and he was crying.
I asked what was wrong, and he said he didn’t take me catfishing this summer. I was like, “Oh no.” He kept thinking that he gave me cancer with the Vienna sausages I ate when I was little. I was like, “I don’t think that’s related to that!” But I appreciate the thought.
My mom handled it really well. Our relationship was great through it all. I think she tried to be strong for me a lot, so I’m waiting to see. I feel she has to take time for herself, too. I think she’s getting better about that.
So much happened at once, and she had to step up. She did an amazing job. I couldn’t have done it without her, at all.
She still has her own needs that I want her to go do, like get a massage, but you can’t spoil yourself when there’s a pandemic!
When I said, “I’m so glad this is over,” my husband said it wasn’t that bad. He lives in his happy little world, so it didn’t change with us. I did see a new side of him. He was my high school sweetheart, so we kind of grew up together into the people we wanted to be.
I got to see him as a caregiver more, where we’re usually pretty equal. That was cool to see that side of him. I don’t think it made us any more close or distant. He just lived his life, and I tried to stay alive.
Taking care of caregivers
That’s important. I don’t want to damage my mom long-term. I need her; I love her.

Be open to people
I think just asking for help is the biggest thing. I got “Most Talkative” in high school, and I didn’t even have to campaign for it. I’m not shy with anybody.
Even with my nursing instructors, they made a huge difference because if I wasn’t feeling okay, if I couldn’t go take a test on a Wednesday, they were cool about me taking it later. I don’t think I postponed anything, but they always had it as an option. They were very adjustable to my clinicals.
Just being open with people. There’s no prize in not asking for help. There’s no prize in being strong. Everybody’s going to say you’re strong no matter what. They don’t know that I cried on the bathroom floor every night.
Just be open with people about things. You don’t have to overshare like I do, but you can ask for help when you need it, and you can tell your oncologist when you have symptoms that aren’t managed. We had to go into a lot of work for nausea control.
The people around you will help you no matter what, especially your medical team because that’s their job. They want to make you feel better. They know a lot of things, and they’ve seen the stuff you’re doing before.
So just ask for help. Be honest with people.
For the first two months, I ate SpaghettiOs 2 or 3 times a day. I hadn’t eaten those since middle school, but that’s what I ate. Everyone around me loved me because of it!
You’re fighting a battle for your life, whether you want to call it that. Do what you have to do to stay alive and take the fewest casualties inside of yourself.
Finding your cancer community
My big thing about humor is I follow The Cancer Patient on Instagram. The memes on there made me feel like somebody got me, and it helped me find friends. I have one local friend who had lymphoma; she had non-Hodgkin’s. I love her, but it helped me find more people, too.
It’s good to have that community. It’s nice to know someone’s going through it. I would never want anybody to have to go through it, but hey, if we’re in this, might as well be in this together.
It helped me find and make friends and get someone who understood me. It helped my humor a lot. Everybody’s like, “Maybe you shouldn’t joke about this thing.” I’m like, “I’m going to! It’s my trauma, and I’ll do what I want with it.”
I found a lot of them through Reddit. I posted, “Does anyone want to make a group chat?” So I made one and made all these friends all over the country and the world.
They were all getting diagnosed the same time I was, but we had different kinds of lymphoma. It was nice to see this is what’s happening. These are the tips we’ve learned from each other.

I would put tape around my medicine bottle so I would know which to take in the morning. They would tell me their tips. I found a close-knit group of friends I could depend on. My friend Hannah, who’s from here, has Burkitt’s lymphoma. We kept in touch all the time. She was a good friend.
My friends on Instagram who I made. I made a lymphoma group on Facebook. It just helps to have people around you who are going through the same thing and that you can influence them. They can help you back.
Community is such a big part of being a human. It’s part of the human experience. Going through something like this is so unique anyway.
Going through it during a pandemic, nobody else out there understands that except my friends who are currently going through this during a pandemic.
It was good to have that community I could count on. We keep up with each other. We root each other on during scan days. It’s amazing. I love my friends, my “lymphomies”!
Perspective going from patient to nurse
I feel like it makes a difference with my patient care. Sometimes you see someone laying in bed, their pain really high, and you think maybe they’re just being whiny.
But I don’t see that anymore because I looked pretty healthy, aside from the baldness and the paleness. I was in serious pain. It makes a difference in how you can see other people.
I’m trying not to say to my patients that I had cancer, but in my heart, I’m able to use that experience and understand this is the lowest low for people. I don’t want to do anything that’s going to take away from that. I want to be able to help them get through this as easily as possible.
So I think [cancer] has made a big difference in my ability to be compassionate.
Last message
It’s okay to not be strong through this. Ask for help. Everybody’s going to tell you you’re strong and you’re a warrior. When it’s all over, you’re going to be impressed that you did it, but it’s okay to not be strong.
It’s okay to cry on your bathroom floor. It’s okay to cry in public. It’s okay to embrace the suckiness of it.
It sucks. Chemo sucks. It’s not fun. Nobody enjoys having cancer. It’s not something we all shoot for in life.
Just remember you have to take care of yourself, because after it’s all over, there’s still lasting damage. I had to go to therapy because I had bad PTSD from the whole experience.
Part of what my therapist had me do was she had me write a journal about every single event that had happened. She had me write about how I had felt at the time and how I feel now. If I had taken the time to process those feelings as they came along, I wouldn’t have needed as much help.
You still need help after something traumatic like this, but I needed to take time to process everything. I didn’t take that time because I had so much going on in life that everything happened so quickly.

So just take care of yourself. It’s okay to cry. It’s okay to hate your life. You don’t have to be an influencer. You don’t have to make it an amazing, beautiful thing.
If you want to, that’s fine. I wrote in journals things I was thankful for sometimes, but I also wrote journals about, ‘Wow, this week really just took it out of me.’
Do what is best for you during this time, because you’re literally fighting for your life.

Inspired by Mara's story?
Share your story, too!
Hodgkin’s Lymphoma Classical Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)
























8 replies on “Mara’s Stage 2BX Classical Hodgkin’s Lymphoma Story”
Hi everybody, here every one is sharing such knowledge, so
it’s nice to read this website, and I used to visit this webpage
every day.
Heya i’m for the first time here. I found this board and I find It truly useful & it helped me out much.
I hope to give something back and help others like you helped me.
We’re so glad Mara’s story helped you! If you want to sign up for our latest stories, subscribe here: https://forms.gle/eBYDHr7fQSv6Z9Sm8.
You can throw them the ball or go for a run together.
Your photos look terrific !!!
Thanks for the kind words to Mara!
Its like you read my mind! You seem to understand a lot about this, like you wrote the book in it or something.
I believe that you could do with a few % to power the message
house a little bit, however other than that,
that is fantastic blog. A fantastic read.
I will definitely be back. Greetings from Ohio!
I’m bored to tears at work so I decided to
check out your blog on my iphone during lunch break.
I love the information you present here and can’t wait to take a look
when I get home. I’m surprised at how quick your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyhow, very good blog!
I’ll immediately snatch your rss as I can not find your e-mail subscription link or newsletter service.
Do you’ve any? Please allow me realize so that I may just subscribe.
Thanks.
Bill, thanks so much for this wonderful comment. If you want to be one of the first to get access to our newest content, here’s our link!
https://forms.gle/eBYDHr7fQSv6Z9Sm8