Fabiola’s Stage 2BX Relapsed Hodgkin’s Lymphoma Story
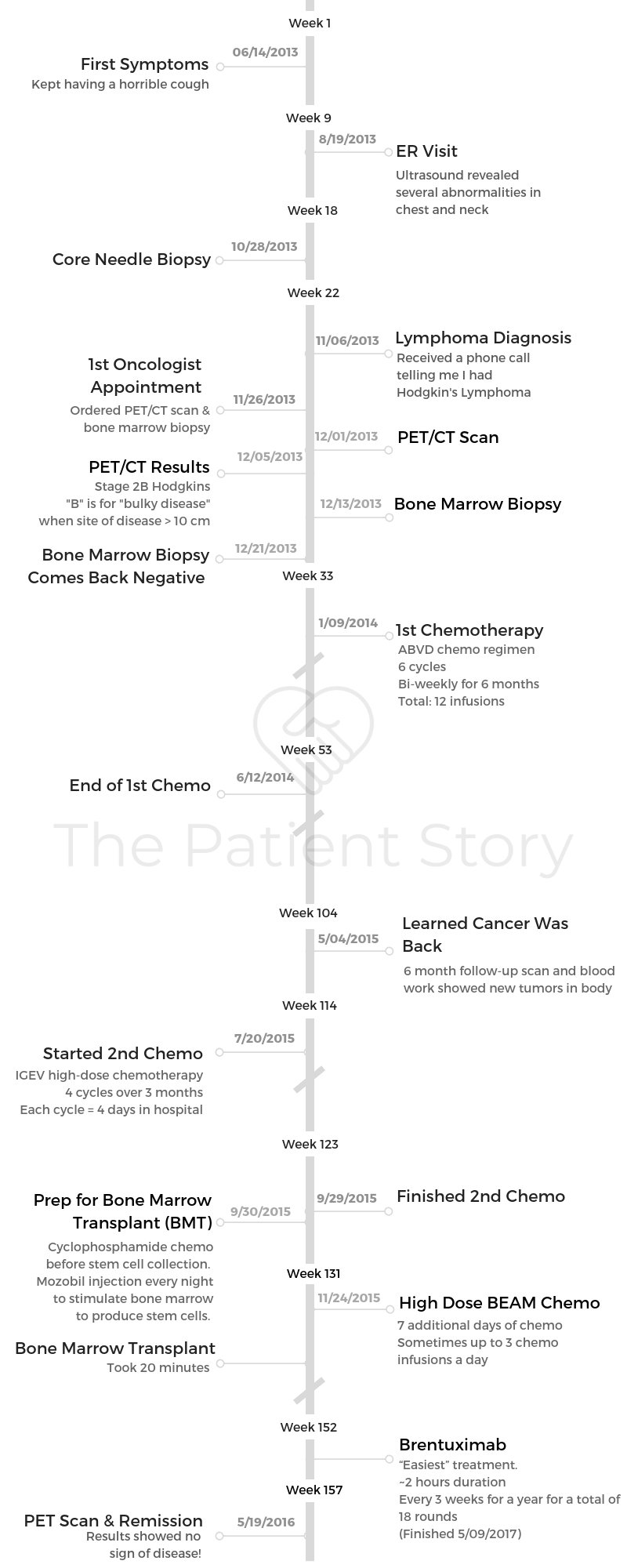
Fabiola shares her Hodgkin’s lymphoma story, which includes getting staged at 2BX (bulky disease), undergoing 6 cycles of ABVD chemo, relapsing, going through more chemo (IGEV), a bone marrow transplant (BMT), BEAM chemo and then immunotherapy.
She also highlights the importance of getting good support, self-advocacy and survivorship.

- Name: Fabiola L.
- Diagnosis:
- Hodgkin’s lymphoma
- Stage 2BX
- B= having specific symptoms like unexplained weight loss, fever
- X = bulky disease (site of disease > 10 cm or bulky relative to chest size)
- Relapsed after first chemo
- Complete response after bone marrow transplant
- 1st Symptoms:
- Shortness of breath
- Dry cough
- Treatment:
- ABVD chemotherapy (1st line)
- Adriamycin, bleomycin, vinblastine, dacarbazine
- 6 cycles
- Biweekly for 6 months
- Total: 12 infusions
- IGEV high-dose chemotherapy (2nd line)
- Ifosfamide, gemcitabine and vinorelbine
- 4 cycles
- Each cycle = 4 days in hospital
- Duration: 3 months
- Bone marrow transplant (BMT)
- Cyclophosphamide chemo before stem cell collection
- Slow collection: 2.7 million stem cells over a week
- BEAM chemotherapy
- Carmustine, etoposide, cytarabine, melphalan
- 7 infusions
- Up to 3 times a day
- Immunotherapy: Brentuximab
- 1 time every 3 weeks
- 1 year
- ABVD chemotherapy (1st line)
- Diagnosis
- What were your first symptoms?
- What led you to go to the doctor's?
- List the tests and biopsies you had to undergo before diagnosis
- Describe the moment you were diagnosed
- How did you break the news to your loved ones?
- Describe that first meeting with the oncologist
- Getting a second opinion
- What did you like about being at a smaller or bigger place for treatment?
- How was your medical team?
- 1st-Line Treatment & Side Effects
- 2nd-Line Treatment & Side Effects
- Bone Marrow Transplant
- When did your oncologist talk about the bone marrow transplant (BMT)?
- Describe the preparation before the bone marrow transplant (BMT)
- What additional chemo did you have to undergo?
- Describe the high-dose BEAM chemotherapy
- How was the brentuximab (immunotherapy) infusion?
- Brentuximab side effects
- What helped you prevent the side effects?
- After the Transplant
- Finances & Support
- Reflections
- What surprised you most about the experience?
- What helped you manage your emotions and thoughts?
- What got you through the toughest times?
- Did you use alternative or holistic medicine?
- Were there moments you had to advocate for yourself in and out of treatment?
- Navigating survivorship
- How do you handle the anxiety around follow-up scans and your health?
- Message to other patients
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

The time will pass.
You will get through treatments.
You will ring the bell at the end of your chemo or radiation.The most important thing is to heal. You need to heal emotionally, spiritually, mentally and physically. We are often so concerned about the physical aspect of the disease that we forget how important our mental health is.
I suppressed my emotions, and at the end I was very depressed. I have healed, but it was not an easy road. Take care of yourself, every aspect. Be kind to your body and nurture your mind.
Fabiola L.
Diagnosis
What were your first symptoms?
For several months, I had shortness of breath and a dry cough. I dismissed these signs because I believed it was a cold or a flu.
»MORE: Hodgkin’s lymphoma patients share common first symptoms
What led you to go to the doctor’s?
In the summer, I had a motorcycle accident. I decided to go to urgent care, where they did an ultrasound of my chest, neck and abdomen.
My healthcare provider decided to follow up with an MRI that showed extensive disease progress. At this time, I was unaware of what was going on. I thought it was routine work-ups.
List the tests and biopsies you had to undergo before diagnosis
In August, I had my first MRI. This was one of the worst tests I had to have done. I did not know how small an MRI machine was. I felt like I was suffocating and became very scared.
After a 45-minute exam, my eyes could not stop running, I kept crying and prayed I never had to have another MRI in my life.
Because the MRI showed a 16 cm by 18 cm mass in my chest and several smaller masses in my neck, my healthcare provider sent me in for a needle biopsy of my neck in October.
This was a simple outpatient procedure where they used lidocaine and inserted a needle with a guided ultrasound. This exam allowed them to take several samples of the lymph nodes that showed disease.
At this point, I was still unaware of what was occurring. On November 6, I was diagnosed with Hodgkin’s lymphoma, bulky disease.
Describe the moment you were diagnosed
In November, both of my grandparents passed away. I was in class doing a biology lab when I got an unknown phone call.
I decided to answer the call, believing it was my mom telling me she was going to fly out to Mexico for the funeral. This was not the case.
It was my healthcare provider calling me to tell me I had lymphoma, a cancer, and tried to explain to me how lucky I was. That this was the best cancer to have.
I remember not being able to breathe. I sat outside of my classroom, and my eyes just teared up. I was so heartbroken.
I was studying hard to be part of the medical profession, and now I had become a patient.
I remember being so afraid to sleep, so I stayed in school until 2 a.m. in the library working on my senior thesis. The moment of my diagnosis felt like I was in a complete standstill. I continued to work on homework, but I have never been the same since my diagnosis.
»MORE: Patients share how they processed a cancer diagnosis
How did you break the news to your loved ones?
After the call, a professor of mine saw me and asked what was wrong. I told her, and she quickly offered to take me home, but I decided I couldn’t break my parents’ heart anymore. They had suffered enough pain from losing their parents.
I decided to call my sister, who has always been my best friend. Within minutes of talking to her, my entire family called me asking me if it was true. I was a marathoner; I ate the healthiest. This was the worst news anyone could have received.
»MORE: Breaking the news of a diagnosis to loved ones
Describe that first meeting with the oncologist
My first meeting with my oncologist was difficult. It occurred a few days before Thanksgiving. He quickly ordered a PET scan and ordered a port placement.
The visit made my diagnosis real.
He explained to me that without treatment I would only live 2 months and would pass in my sleep because the tumors were engulfing my my trachea and lungs. It was hard hearing this. I decided that I couldn’t be with a doctor who was so cold and had a poor prognosis.
Getting a second opinion
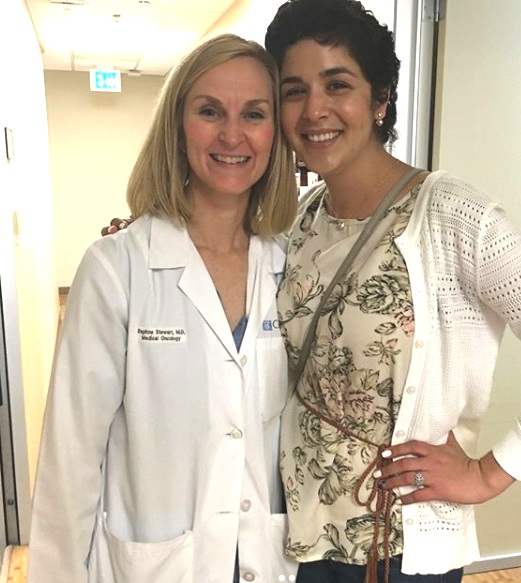
I decided to get a second opinion from Dr. Stewart at City of Hope. On December 26, I met with her, and she changed my whole perspective about my disease.
She reassured me. She gave me so much hope and allowed me to believe that I would be okay.
What did you like about being at a smaller or bigger place for treatment?
With my initial treatment, which consisted of 6 months of ABVD chemo treatment, the facility was small. It was 4 floors, and the infusion room had about 18 chemo chairs.
I loved being here. It felt like family. I went in for chemo every other week for 8 hours, and the nurses always provided me with comfort.
When I relapsed, I was inpatient at a large facility. With my first admission, I was overwhelmed, nervous and scared. I had never been hospitalized.
How was your medical team?
My entire healthcare team was extraordinary!
The volunteers guided me through the facility. My doctor was my greatest cheerleader. She kept pushing me, believing in me, and always encouraged me when I was down.
She wanted me to stop going to school, but when I refused, she always kept pushing me to do better and feel better.
Because of my oncologist, I was able to graduate college. I really believe it was my doctor who encouraged me and was there for me the most.
But I did have an entire healthcare team that always provided me with reassurance, love and comfort.
1st-Line Treatment & Side Effects
1st ABVD chemo cycle
With my initial treatment, I underwent 6 months of ABVD chemotherapy, which was done biweekly and took about 6 to 8 hours.
»MORE: Read our comprehensive ABVD chemotherapy info page
ABVD chemo side effects
The side effects of ABVD were tolerable. Reglan and Zofran (anti-nausea medication) allowed me to eat. Reglan was my best friend. Zofran helped, but it gave me headaches. However, the steroids made me gain about 20 pounds.
Recovering from ABVD chemo
After chemo was over, I was overwhelmed with emotions. I was so happy but also so nervous that the cancer would come back. I struggled emotionally to return to a “normal state.”
Your hair loss
Hair loss was hard. For so long I pretended I was not sick, but the hair loss made me feel so vulnerable, and it broke me.
I felt like the cancer had stripped away my dignity and took away my identity and life.
Were you surprised by your reaction to losing hair?
I was at a restaurant, where I felt my hair just fall. When I removed my hair tie, about 90% of my hair fell out. It was painful and hard. There are no words to describe the way I felt about this.
»MORE: Dealing with hair loss during cancer treatment
What helped with the hair loss?
I only wore cotton beanies. It kept my head warm, protected me from the sun and made me feel better. I hated wigs.
»VIDEO: The Patient Story Video: How to Cope with Hair Loss
Describe the first follow-up scan
I had several follow-up scans during my chemotherapies, which all showed stable disease or slight reduction. In July 2014, I was told I was in complete remission.
Temporary remission
This remission lasted 6 months. I went in for a follow-up scan and blood work 2 days after my graduation that showed new tumors in my body.
This follow-up was hard. I could not believe it. I continued working until we had more answers about my scan.
How did you approach the issue of fertility preservation?
Before starting high-dose chemo, my oncologist scheduled several biopsies and lung function tests. She also sent me to a fertility clinic because I would (likely) become infertile with these lines of treatments.
She called her friend who was a fertility specialist, and within a few weeks we began the egg retrieval process. I could not have survived all of this without the support of my doctor.
»MORE: Fertility preservation and cancer treatment

2nd-Line Treatment & Side Effects
Describe the 2nd-line chemo (IGEV)
When I relapsed, I received high-dose chemotherapy that was done inpatient. This treatment was called IGEV and was done 4 times over the course of 3 months.
I received this from July 2015 to September 2015. Each hospitalization was 4 days, and each day included a mixture of the chemotherapies. IGEV chemotherapy was hard. My hemoglobin fell to 5.0 (normal is 12 to 14), so I was fatigued, had weakness, and was unable to eat at times.
What were the side effects?
- Severe nausea
- Fatigue
- Loss of appetite
- Weakness
- Low blood counts. I had to inject myself every day for a week with Neupogen to make sure my white blood cell counts (WBC) were high and I was not at risk for infections.
What helped prevent the side effects?
I ate small meals and always made sure I was not in crowded places when my blood counts were low.
Recovering from IGEV chemo
During this chemo, I knew I still had a long process to go. I just wanted to rest before the “real fight” began.
Bone Marrow Transplant
When did your oncologist talk about the bone marrow transplant (BMT)?
My oncologist knew right away after I relapsed that I would need to do a bone marrow transplant. She told me that without a transplant, I had a 95% chance of relapsing. With a bone marrow transplant, my chances of a relapse decreased to 50%.
A bone marrow transplant was my real chance at a cure.

Describe the preparation before the bone marrow transplant (BMT)
After completing IGEV, I was sent to the bone marrow transplant team, where I received cyclophosphamide chemotherapy prior to stem cell collection.
Because I had received so much chemotherapy, stem cell collection took very long. I was only able to collect 2.7 million over a week. Typically people take 2 days to collect that amount.
I had to have Mozobil, which is an injection to stimulate your bone marrow to produce stem cells, every night before I went in for collections. These injections cause severe bone pain.
After collecting enough stem cells, I had to receive the okay from the cardiology, respiratory, nephrology team to ensure my vital organs were healthy enough for the transplant.
»MORE: Hear from a Bone Marrow Transplant specialist
What additional chemo did you have to undergo?
I was admitted on November 22, two days before Thanksgiving, where I began BEAM chemotherapy.
Describe the high-dose BEAM chemotherapy
BEAM chemotherapy was done for 7 days. Sometimes I received chemotherapy 3 times a day. This was emotionally and physically hard.
I remember telling my nurse, “You are hanging another bag of chemo? Why?” When my nurse left, I could not stop crying.
The chemo made me feel so sick. I had never experienced such high levels of pain when I swallowed, when I moved, and the exhaustion is indescribable.
I remember I had to shower every day, and it felt like I had run a marathon. My muscles were sore, my legs felt weak, and oftentimes I had to sit on the restroom floor to change because standing up was too difficult.

How was the brentuximab (immunotherapy) infusion?
Brentuximab was the “easiest” treatment. It was done within an hour infusion and 30 minutes of pre-medications. I received this treatment every 3 weeks for a year, for a total of 18 rounds.
Brentuximab side effects
There was no hair loss. My hair actually grew. Slowly, but it grew.
I had severe muscle pains, and a year later, I still have peripheral neuropathy that the treatment caused. My walking is a lot better, but for over a year I walked with a limp.
What helped you prevent the side effects?
I was on Reglan for nausea and took gabapentin every day for almost 2 years to improve my nerve damage that the drug caused.
After the Transplant
When did you learn you were in complete remission?
I was told I was in complete remission on October 15th. I was so happy and overwhelmed with emotions. I returned to work and continued school; I graduated May 2nd the next year!
How often do you have follow-up appointments and scans?
After finishing my treatments, I now see my oncologist every 3 months, where she does blood work. Every 6 months, we do a PET scan to ensure the cancer is still in remission.
Advice on “scanxiety”
Scanxiety is the worst experience anyone can have. I have been in remission for 2 years, and the weeks leading up to a scan paralyze me.
I become so scared because I do not want to fight this disease a third time. I fear losing my job, my hair, my school. I fear losing the sense of control. Scanxiety has become better over the years, but after relapsing they are hard.
I now run. I remind myself that I have enough strength to keep going even if the results are not what we hope. That has empowered me to face scans head-on.
»MORE: Dealing with scanxiety and waiting for results
Finances & Support
Financial toxicity: paying for cancer treatment
The financial aspect was difficult. I had to stop working, and school was expensive. I was fortunate to have some support from my sister.
I was very fortunate to be covered under my dad’s health plan, which covered every treatment, biopsy, surgery and scan.
Could you study or work through treatment?
I was able to study, although my doctor was reluctant to the idea until I told her I couldn’t lose another thing. She agreed and realized how strong school kept me.

What do you wish you had known to help with the financial process?
I was able to get unemployment. When I relapsed and required a bone marrow transplant, my doctor suggested disability for me.
I had no idea I was eligible for disability until I was undergoing the bone marrow transplant process.
My boss never explained to me what I was eligible for. She just signed the paperwork stating my leave of absence had been approved.
Did you have help in preparing for issues outside of treatment?
My family took care of me. My sisters brought groceries over. My dad made sure I had the best health insurance through his employer. Eating was difficult, so my mom made simple soups or salads (if I was not neutropenic).
What type of support was most helpful?
The best support I had was friends just listening to me — not saying anything, just listening. I had so many friends who left my side because it became overwhelming.
I had friends tell me I was not the picture of cancer. I have to say I just needed someone by my side not saying anything, just being fully present.
»MORE: What kind of support cancer patients say helped the most
How important is it to have caregivers?
Caregivers get the cancer, too. They suffer so much because they want to take away the pain, and they want to do everything to ensure we are okay.
Caregivers are the heart. They keep us going, they fight for us when we are too weak to fight, they advocate for us, and they mend our brokenness.
Reflections
What surprised you most about the experience?
What surprised me the most was the inner strength that I discovered in myself. Cancer is such a scary and lonesome disease, but through social media, I was able to find a support system of survivors that empowered me to move forward every day.
When I thought I would be unable to move forward, I kept going. When my cancer came back, I felt robbed and couldn’t breathe.
But when I got into my car after being told it had returned, I drove to the mountains and did a 10-mile hike to remind myself that there was more life to me, that I was more than just cancer.

What helped you manage your emotions and thoughts?
Running helped. Being busy with schoolwork. Going to Disneyland every Friday with my little sister, running half marathons, and listening to music that inspired me.
What got you through the toughest times?
My sister decided to sign me up for a marathon that I did 2 months after my transplant. The transplant was hard. I would pray because I wanted to die. The pain was unbearable. The nausea was draining, and the constant throwing up brought me to my knees.
My sister believing in me, believing that I would make it, kept me going. My doctor telling me, ‘Your glass is half full. Keep going.’ My hero. That pushed me when I wanted to give up.
Did you use alternative or holistic medicine?
Yes, we tried alkaline water, expensive juices. The cancer never improved, so I stopped spending the money. I put all my trust in my chemo and my doctors.

Were there moments you had to advocate for yourself in and out of treatment?
My doctors did not want me to go to school. I advocated for myself. I told them that school was all I had, and I couldn’t lose something else because of cancer.
I asked them to let me walk around the units because I felt isolated and depressed when I did my transplant.
»MORE: How to be a self-advocate as a patient
Navigating survivorship
It has been a couple years since my last treatment, and there are certain days when things are just hard. I just want to break down and cry. Some days I just want to lie down.
Life after cancer is a roller coaster of emotions. You just have to buckle in and ride it out. Most days are good. I am able to see beauty in everything and wake up feeling fortunate to be alive.
I do believe cancer survivors suffer from PTSD. To this day, my heart races when I drive past my hospital. So many things trigger such vivid memories.
How do you handle the anxiety around follow-up scans and your health?
Running is my escape. It allows me to believe that I can overcome the fear because I know that I will continue to place one foot in front of the other.
I also try to schedule next-day appointments so that I am not waiting to see if I get calls from my oncologist.

Message to other patients
I know they feel alone and scared. I felt the same way. When I was diagnosed, my whole world fell apart.
I would tell them that they are not alone, that so many of us have survived and are thriving after our battle.
I would tell them to make goals for themselves, to plan something so that they can have something to look forward to, to believe they are much stronger than this disease [and] they are not defined by this disease.
To not feel betrayed when friends walk away, to advocate for themselves, but most importantly to fight like hell, to believe in themselves.
And to never, ever give up on hope.

Inspired by Fabiola's story?
Share your story, too!
Hodgkin’s Lymphoma Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)