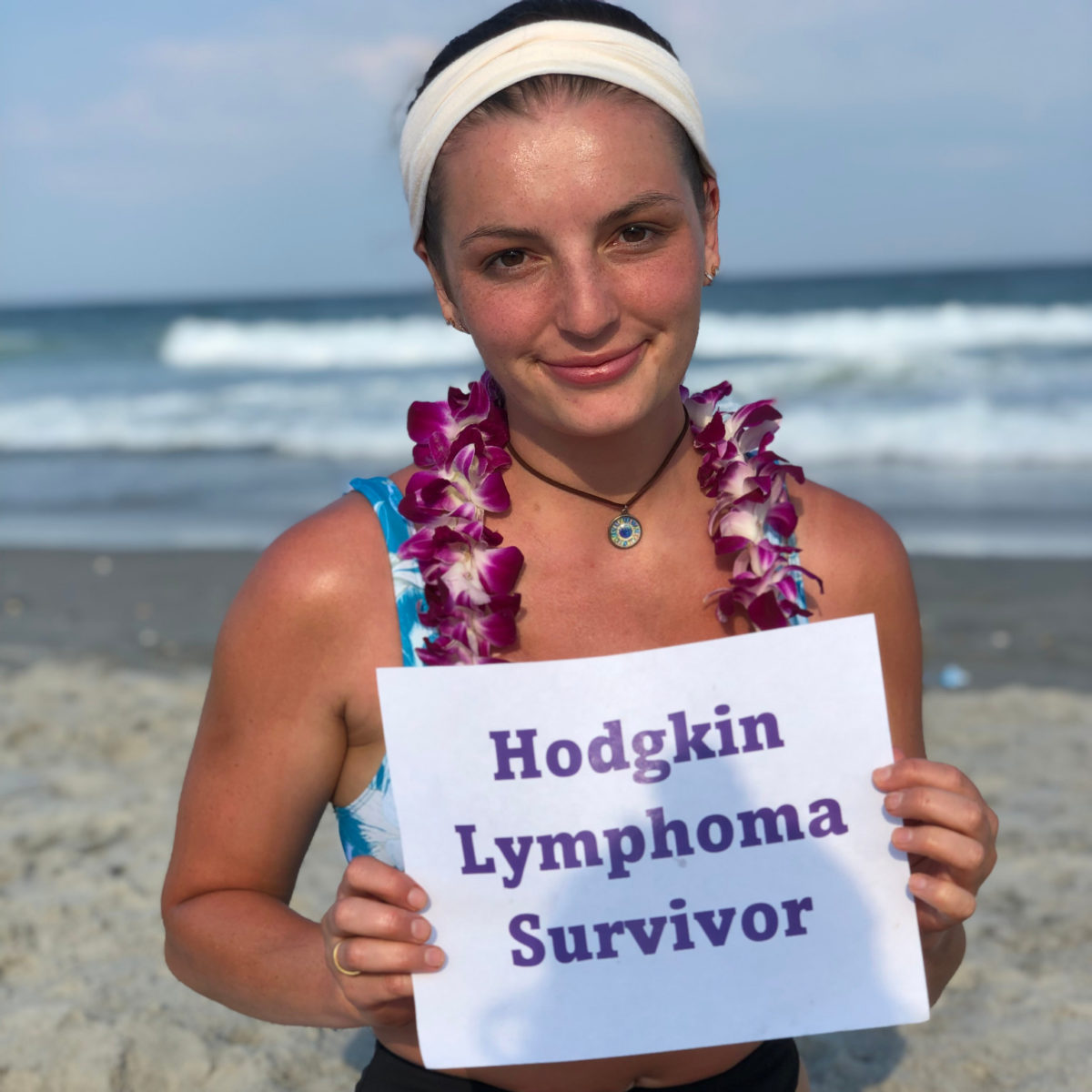
Erica’s Stage 3B Classical Hodgkin’s Lymphoma Story
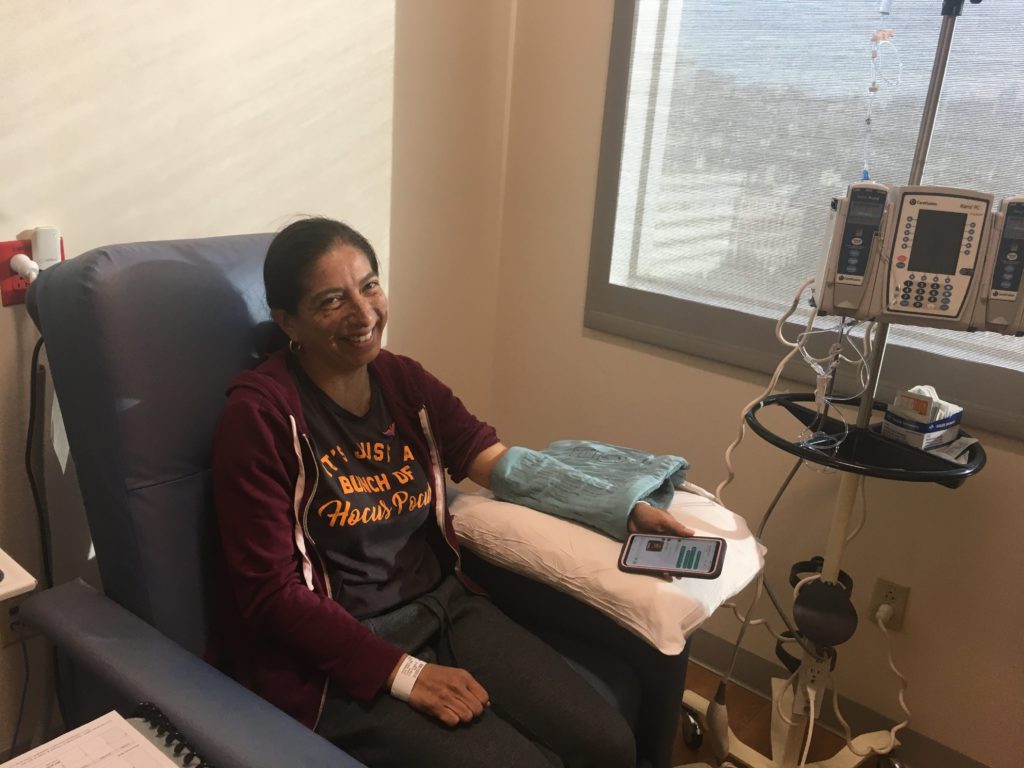
Erica was 36 when she got her stage 3B Hodgkin lymphoma diagnosis. She details her journey through ABVD chemo and hair loss, dealing with financial toxicity and advocating for herself as a patient.
- Name: Erica H.
- Age when diagnosed: 36
- Diagnosis:
- Hodgkin’s lymphoma
- Stage 3B
- 1st Symptoms:
- Growing lump on side of neck
- Itchiness
- Severe night sweats
- Weight loss
- Tests & Biopsies:
- Needle biopsy (fine needle aspiration, or FNA)
- Excisional biopsy
- CT scan
- PET scan
- Blood work before every treatment
- Treatment:
- ABVD chemotherapy regimen
- 6 cycles
- Each cycle = 1 month, biweekly
- Total: 12 infusions
- 6 cycles
- ABVD chemotherapy regimen
- Tests and Scans
- What were your 1st symptoms?
- What was the series of tests and biopsies you had to undergo?
- Describe the fine needle aspiration (FNA)
- When did you get the FNA results?
- Describe the surgical biopsy procedure
- What were the surgical biopsy results?
- How was the CT scan?
- Warning: you’ll feel like you’re going to the bathroom with the contrast dye!
- How long did it take to get the CT scan results?
- Pushing for the PET scan (self-advocacy)
- Describe the PET scan
- How long did it take to get the PET scan results?
- Diagnosis
- Treatment Decisions
- Chemotherapy
- Quality of Life
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I know a lot of people I met didn’t want to talk about it, and when they didn’t, it left me feeling isolated. As a result, I just want people to know that people do want to help.
It is a traumatizing experience to think back and live through, but I also found a lot of people who were willing to help.
The community I surrounded myself with, whom I trusted, was also willing to help me find those things when it was hard.
Erica H.

Tests and Scans
What were your 1st symptoms?
Initially, physically, I noticed a change in my neck. My mom had thyroid cancer 2 years ago. She was able to have surgery. She recovered within a couple of months.
When I found a lump right here on my neck, I didn’t worry too quickly. I knew to schedule an appointment, which I did.
Then I talked to my primary doctor, who right away showed some concern and started to schedule me a series of tests.
Initially, it was a physical lump, but after that physical appointment with my doctor, I did start to have more symptoms, some of them a lot more challenging.
The itchiness is one. It was in a sensitive area, where the itchiness just got worse and worse. I started to have severe night sweats, where I lost a lot of sleep and lost a lot of weight because I wasn’t able to eat full meals.
In July, when that physical lump hadn’t worried me, a week after that physical and the few weeks after, I started to experience some of the more severe pain and symptoms.
What was the series of tests and biopsies you had to undergo?
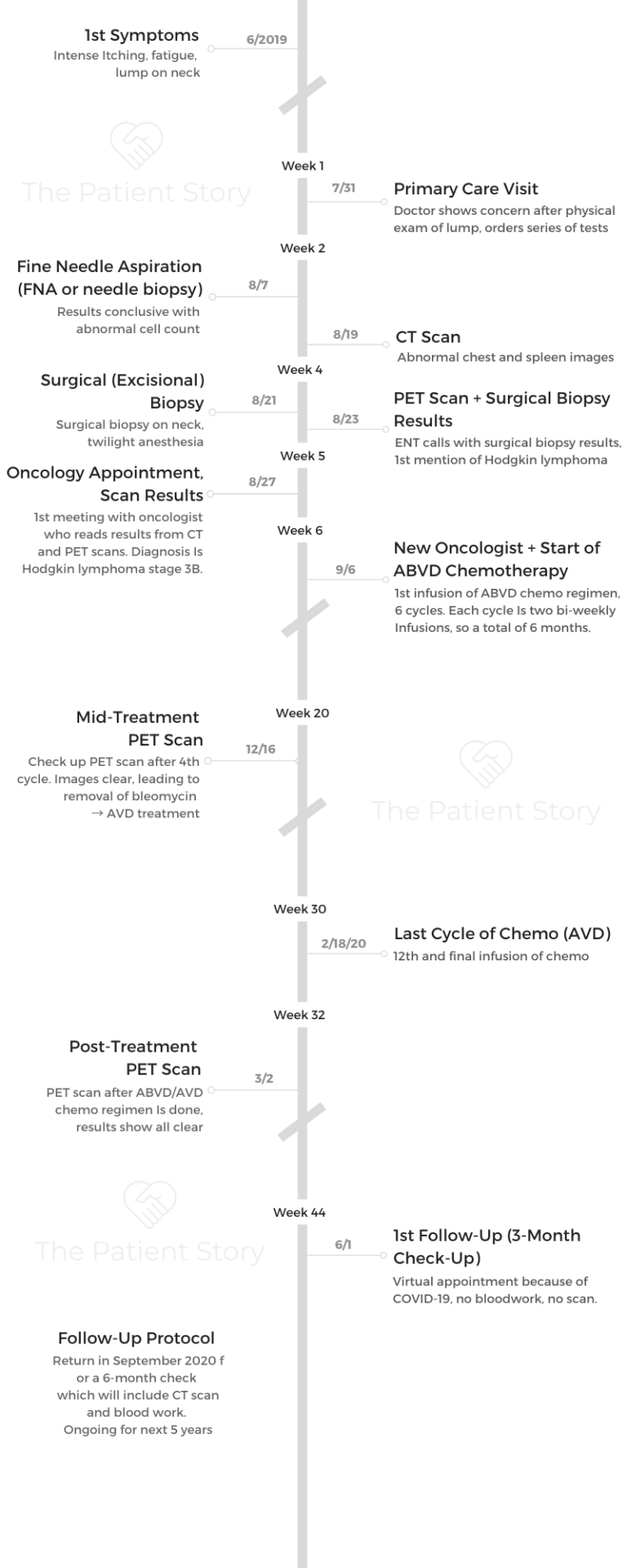
The first appointment happened at the end of July of 2019. Then because she was concerned that it might be something more serious, she scheduled an ultrasound a week after, maybe 5 days after. Then she scheduled the biopsy 2 or 3 weeks later.
All the series of tests took a little over a month, and no one was able to tell me anything. There was the stress of that unknown. It was really starting to preoccupy me and make me much more aware of the symptoms.
I think I tolerate physical symptoms pretty well. The anxiety caused me to get more nervous and feel everything much more intense as I went through the series of tests, waiting for an answer.
I went go get a CT scan, and I had to go get a PET scan. I had to go to an ear, neck and throat doctor, who was a quick moment in time. She was really caring and led me through the biopsy test.
I had a needle biopsy and then a surgical biopsy. She walked me through, but she was such a quick moment that I don’t remember her name.
She’s the one who made the call to me to let me know the results of the surgical biopsy. She said over the phone, “I’m pretty sure it’s cancer, but I’m not an oncologist.” That’s how she ended the conversation. I was like, “What! What will make it more conclusive?”

Describe the fine needle aspiration (FNA)
I ended up going by myself because it was going to be a quick test. I’m very scared of needles. I never dared to have lab results done unless told by my doctor, because needles scare me. It’s part of the fear and reason that I never gave blood. I never was a blood donor because of the needle.
Going into that appointment, I knew what was going to happen, but actually seeing how big the needle was really freaked me out. I was by myself because I was like, “I can do it.”
The doctor I had was understanding, and she said to me that a lot of patients actually have a fear of needles. She walked me step by step through what was going to happen, how they were going to numb the area so that I wouldn’t feel it.
[They stuck the needle into the area of the lump with a long, thin needle.] It was a quick prick. The numbing sensation was much harder to deal with. It was so quick.
And I wanted the answers, so I pushed all my fears aside because I needed to get this done to get answers for myself.
It was a very, very quick process. I don’t know if I was there more than 20 to 25 minutes.
When did you get the FNA results?
It was a Friday afternoon, and I was fishing to have answers right away. I think I got the results back on a Monday or Tuesday of the following week.
The ENT was the one who gave me the results. She said it was inconclusive. She said there was still concern and wanted to do the surgical biopsy.
Describe the surgical biopsy procedure
I walked into it not doing a lot of research. I’m really good about doing research, but I figured they’ll me when I get there, just like they did the needle (biopsy).
When I got there, I got nervous when I had to sign some release papers because I didn’t realize it was a surgery since over the phone they said, “You’ll be out within an hour.”
When I signed the release papers, that’s when I started asking the questions of what exactly I was going to go through, because being unaware of that for myself got me nervous. I realized they’re probably going to use some anesthesia, and I’m going to be out for the count.
That was not the case at all. It is surgery because they did have to have it open where I had found my lump. They numbed it, but I wasn’t under, so I was aware of what was happening, but I couldn’t feel anything.
They took a piece of what was there out and were going to send it to the labs, which is why I had to have surgery — so they could cut open and take a piece.
Because I was aware of what was being said, I remember the doctor who was doing the surgery say something like, “This feels like…”
When he was done, I brought up that conversation I had overheard. He said, “I can’t say anything conclusive now, because nothing’s conclusive unless it’s in the lab and we can study it, but it feels like what most cells under certain cancers feel like.”
It was making me more aware that it was a high possibility, but because nobody could be 100% conclusive, I still sided with hope that this was nothing.

What were the surgical biopsy results?
After that, they gave me the results back that Friday when the ENT doctor called me. That’s when I knew it was something serious, and I would have to go through treatment.
I didn’t have the idea of cancer, not being familiar with any other type of cancers, only those exposed from the media and with some family, who didn’t have a pleasant experience.
She called me on that Friday, and she said, “This is serious. I can’t tell you everything about what it is, but it’s very likely a Hodgkin lymphoma.” That was the first time [I heard of Hodgkin lymphoma].
What she did do was say, “You have to schedule an appointment with an oncologist.”
I was like, “I don’t have that readily available.”
Immediately after that, I sent my primary care doctor an email because I was getting frustrated with so many people not wanting to be 100% conclusive about what was happening.
Knowing there was something there, but they weren’t fully telling me what that was. Maybe it was a point of caution, protecting me from going down a path by myself or whatever. I just wanted it to be conclusive, so I called my primary care doctor.
How was the CT scan?
It was my first time. I knew they had to put some dye, and there are so many different variations of how CT scans [are done]. That is something I did Google: “What is a CT scan?”
Before the appointment there, I called and asked, “What kind of CT scan is this? Should I not eat anything?”
The person who made the appointment didn’t tell me everything I should do prior to the appointment. They said, “No, just come in.” At my hospital, it’s in a trailer. I noticed that a lot after that appointment. I noticed a lot of hospitals are putting their CT and PET scans in trailers because of the radiation and outside the facility. So that was a different experience, getting walked from the waiting room into a trailer.
It was quick. They put a needle in you to put the [contrast] dye in, and you lie on this bed. Then you go inside a half-tube, so it’s not an MRI where you go in fully. It’s a half tube. You lie there as still as you can until they have enough images of you for themselves.
I’m not nervous, not claustrophobic, and because I’ve learned to meditate over the years, I found myself meditating as I went to do that.
They walked me through it, saying, “Hold your breath. Now release your breath. Hold your breath. Now release your breath.”
This may sound weird, but because I don’t like needles, I appreciated this kind of test, when I wasn’t exposed to long needles or anything.
It’s just a little prick on the arm to get the dye in me, feel a little heat sensation and be done with it. I didn’t find it as scary as some of the others.
Warning: you’ll feel like you’re going to the bathroom with the contrast dye!
It’s a weird sensation! They warn you. The technician administering it will say, “You’re going to feel this sensation. Don’t be alarmed.”
How long did it take to get the CT scan results?
It took them a week. I didn’t even get to see the results until the oncologist appointment. It was very surreal because I was going through one test after the other. I don’t remember exactly when they talked to me about that, but I do remember them bringing it out for my oncologist appointment.

Pushing for the PET scan (self-advocacy)
I pushed for that to happen more quickly. What I’ve learned about PET scans is that they’re very hard to administer because there are so few of them in hospitals. Looking back, I would recommend for a person advocating for themselves to push to see if a PET scan is needed and to make sure it happens.
A CT scan happened for me, and then when I was told I should get a PET scan, I asked a lot about why I didn’t have the PET scan right away. When I was trying to schedule it for myself, nobody was scheduling it for me. It seemed like it was going to be months out.
They were like, “You can’t have a PET scan until September.” I was like, “No, no.” I think what helped me get it earlier was I had said from the beginning that my husband and me had a vacation planned, and I needed to know whether or not to take that trip because I was starting to get worried. When they said September, I said, “That’s in the middle of the vacation.”
Putting that urgency in them helped them find a hospital that did have a PET scan earlier than what they were offering me. I actually had to drive about an hour and a half away from where I live to go to that hospital facility to get the PET scan.
I was exhausted from all of the tests, and they assured me that this would be the last test, where they’d be able to be more conclusive about what I had.
So I went with my husband, and we made a trip out of it. We went with enough time. I met this wonderful woman in the waiting room, who saw how anxious I was and just sat with me. That was one of the most soothing, most calming conversations I’ve had.
I was like, ‘An hour and a half drive to have this conversation is probably my destiny.’ When I went into the PET scan, I felt almost relieved that this might be the last test so that they could just conclude what was happening.
Describe the PET scan
The technician was wonderful. They put a sugar substance (glucose) in (through IV), and you have to wait an hour before you go in to get a PET scan. When he put it in, the technician told me to just take a nap for an hour.
Similar (to the CT), but different because of the hour-waiting period beforehand. [With the] CT scan, you go straight in, they put the IV in and scan you. The PET scan, they put it in, and you wait an hour for (the glucose) to go through your entire body before they do the scan.
The PET scan only took about 20 minutes. So it was waiting an hour, 20 minutes for the full scan, 5 minutes to close out.
How long did it take to get the PET scan results?
Because I had pushed all these conversations, I had my first oncologist appointment the following Tuesday, which is when the PET, CT and all other tests were put in front of me.
Diagnosis
Trying to get answers from the beginning
I was at Kaiser South San Francisco. I only say that because South San Francisco doesn’t have all of the tests (and equipment) you need. They don’t have a lot of doctors to administer these tests, so it was taking them a long time to coordinate.
With so many patients, I found myself needing to prioritize myself.

It’s like the doctor wants to help you, but there’s a line that you’re in. I was not willing to wait in line, for better or worse, because I had this trip, and I needed to know whether or not to take it.
I sort of aggressively said, “I get there’s a waiting period, but I need to have some of these tests done faster, or I needed the results faster.”
I just really wanted to know. I had planned a vacation with my husband. I was pushing for more answers so that we could decide whether or not we were going to go on that trip. When she said, “I’m pretty sure, but it’s not conclusive,” that’s when I pushed my primary doctor to coordinate all the pieces together for me.
In late July when I had met with my primary care doctor, the medical system had pushed me to do all these tests with other people, and now I was hearing from the ENT, “I’m pretty sure, but…”
So I went back to my primary care doctor and said, ‘I really need an answer. If this is something that looks like cancer, I need to know.’
That’s when they finally scheduled me with an oncologist at the medical facility, and I finally heard about a month and some weeks later, yes, 100%, this is what they had now diagnosed as Hodgkin’s lymphoma.
The diagnosis at the oncologist appointment
I’m with my husband. I knew at this point, and I wanted to be with someone. I had felt pretty sure that I had Hodgkin’s lymphoma because so many people had said it was likely. My husband, I think, did not have that full understanding yet.
I bring him up because my doctor came in the room, he walked me in, and he said pretty matter-of-fact, “You have Hodgkin lymphoma. Stages don’t matter, but we name it because of where it’s located in the body. For you, it’s in the spleen, so it’s stage 3B. Based on your symptoms and where it’s located, that’s how we can understand what treatment to give.”
Processing the diagnosis
My husband went white pale. He was so pale compared to the wall. The doctor didn’t recognize at all. He just kept going through the motion and diagnosing me, telling me the next steps.
I had to ask my husband if he was okay, which gave him permission to leave the room really quickly to catch his breath.
It was really upsetting because I wanted the doctor to acknowledge that it’s not just me getting the diagnosis. It’s both of us. We’re going to have to both go through this.
I obviously have to go through the treatment. But I remember just losing focus a little for the rest of the conversation and not necessarily processing all the other details.
He gave me a handout to say, “This is the standard treatment that you’re going to have, ABVD. This is what it is.” We concluded the appointment with him walking me through the infusion center because it’s right next door.
We walked through. He introduced me to a nurse and said, “Okay, we’re going to get started as soon as possible.”
I just remember walking out, and I was angry that I had to wait again, because I thought getting the diagnosis was great. At least I had some clarity in it, because then I could move forward. But again, that weighed on me knowing that this could possibly be the doctor I worked with. I wasn’t going to have that. It wasn’t a great first appointment with them.
It was a relief to finally receive the diagnosis, when for the past month I had only heard, “I’m pretty sure,” or, “I think it is,” or, “Maybe.” When you hear the, “Yes, it is, 100-percent sure and this is the treatment that is given,” it was that weight that lifted from me.
»MORE: Processing a cancer diagnosis

How did you get through the 6 weeks of waiting for answers?
I call myself a lifetime runner, and any challenge that I’ve ever experienced in life, I would run. I would run around my neighborhood. I would take different trips around the Bay Area to different hiking trails to go on a run with my brother. I’m still amazed at what the mentality of how you handle certain anxiety can get you through.
I was having very severe symptoms at that point. I was having night sweats, maybe getting 3 to 4 hours of interrupted sleep, and yet I was still running because I needed that for my mental state.
It wasn’t fast running. I noticed I was slowing down, but I would push myself to go outside and think of what my body’s capable of, despite the stresses of what was happening.
Looking back on it now, there’s a race I did with a runner’s club I’m part of here, and it was a 3-mile run. At the time, I’m like, “Definitely, I could do 3 miles.” But it was a lot of hills I wasn’t expecting. I still did it.
[At] the race, they took pictures of you, and there’s a picture of me at the finish line. As I look at that picture, I think, “Whoa, I was going through all of these unknowns, and my body was inflamed and feeling hot, uncomfortable. Yet I’m there, finishing.”
It was finding those moments to be really proud and amazed at what my body could handle, which got me through the waiting period.
Even when I received the diagnosis, I’m like, ‘This body is really strong, and whatever treatment I have to go through, I trust that it’s going to be strong enough to handle.’ At least that was my hope.
I was also amazed with the community I had surrounded myself with. I’m spiritual and religious. I found myself going back to praying devoutly and with my father, who I hadn’t prayed with in a really long time.
He lives close by, fortunately for me, so I stopped by my parents’ and said, “I’m going through this and need us to pray.” So praying with my parents and my husband really helped me mentally know I have this community of people who are going to care for me as well.
And I have myself. As strange as that sounds, it was like I have my community that’s going to support me, and I have myself. Those 2 things really helped me get through this really stressful waiting period.
Treatment Decisions
Getting a second opinion and more information
It prompted me to look at a second opinion and talk to other people. I do appreciate you putting this together, because I did go online to look for other support organizations with Hodgkin lymphoma to gather all my facts for myself, rather than one doctor telling me this was it.
I was looking for people who’d been diagnosed with Hodgkin lymphoma, trying to find out if it was the standard, because hearing that it’s the only option was annoying to me. I wanted to know, is this treatment it?
I wanted to talk about nutrition because I’d read that nutrition helps with treatments. I also wanted to explore that, but the first oncologist was unwilling to talk to me about that. He said, “This is it. This is what you have to do, and it will go away.”
I refused to believe that, so I did seek a second opinion at Stanford. It was an online doctor, I later found out. I thought I was going to have an appointment. Being vulnerable in that moment, I saw Stanford’s online second opinion.
I thought I was going to meet a doctor there, and it wasn’t that at all. It was me submitting my results for a doctor to look at and having one of their nurse practitioners call me to make the same conclusion.
Looking back on it, it was helpful for me personally, but I don’t think I would have needed that if I had heard it differently the first time.
Getting another doctor
I talked to my primary care doctor because at the end of the day, she was my coordinator. I’d seen her for years, and she’s the one who prompted the tests.
I asked her if there was another oncologist on site because I didn’t feel comfortable. Her answer was a quick no. There’s no one else. This is all she knew of. I think she even ended the conversation with, “Good luck.”
But I know Kaiser is a big operation, and there are other hospitals. Because I live in San Francisco, I was encouraged by a friend to look at Kaiser San Francisco. Even while I was waiting for my second opinion, I had reached out to them.
I’m so glad I did because it was such a different world there.
I was able to almost back-to-back get the Stanford second opinion, and at the same time get a call from Kaiser San Francisco letting me know that one of the doctors were available and was able to see more patients. So they partnered me with him.
My first appointment with him was a little more than an hour. To be transparent, he was a fellow in the hospital. I didn’t care because I figured he’s working with other oncologists who had been there for over 30 years, so in fact, having a fellow partnered me with 2 other long-time, experienced doctors.
My first appointment, Dr. Neeman (the fellow) and Dr. Lopez (who is the overseeing doctor) came in and gave me a hug.
They said, “We’re sorry you’re going through this. You must be really stressed out.”
I remember starting to tear up a little bit because that’s all I had wanted — the acknowledgement that this was scary. They noted that.
Then they went through the logistics. They also told me about all the resources that are available at Kaiser San Francisco that I didn’t even think to ask, even through all my research, even in the initial appointment.
They let me know there’s a social worker on site, a nutritionist that’s available to help me with the eating piece, [and] a chemotherapy orientation available to answer all my questions about what that would look and feel like.
At the end, they left and said I was going to be fine. It was just a weight off my shoulders. Yes, this is all I wanted.
That acknowledgement, the support, and the other pieces of information, not just about the cancer but how to deal with it, which was really helpful.
Relationship with doctors
What has helped me with working with the doctors, because it is a community of people wanting to help you. I would have never said that had I gone through this, but I only say that because doctors don’t want to give you information that might not necessarily be true.
In the world of science, everyone needs 100% assurance before they move forward with treatment or interrupt your life. What helped me was just asking a lot of questions.
It wasn’t until that test (surgical biopsy) that I started, for unhealthy reasons, Googling a lot. But I wasn’t Googling, “possible diagnosis.” I was Googling, “questions I should ask my doctor” and reaching out to friends who work in the health field on what questions I should be asking.
As a patient, they don’t want to alarm you, but they also want you to take caution that this is something serious and you should move forward, especially as people have so many of their own myths and ideas of what cancer and treatment are.
Guidance on top questions for patients and caregivers to ask doctors
The important questions are letting them know everything you’re going through. Not just related to the physical, but sometimes where we go to.
I know when I would go to the doctor, I would only talk about the physical, but also the emotional piece and other pieces you’re concerned about.
Friends and family have always told me I’m a workaholic, so this interruption was obviously going to interrupt that. I told the doctors at that appointment, “What about work, and how am I going to deal with that?”
That’s when they brought up the social workers. They said they’re going to be available to you to help you through that. They’re the expert in it. I’m the doctor and I’m the expert in a, b, and c, which is really helpful because in organizing all of the things that you’re going through, it was easier for me to hear people say what they’re the expert in.
So, I’m the doctor, I’m the expert in treatment. This is how I’m going to work with you the next few months. I was able to put that in a notebook and say this is what I go to this doctor for, what I go to the social worker for, and whom I go to for what I eat. I used all of those resources.
When I didn’t find them, I would ask and the social worker became a huge part of my journey because she was so knowledgeable in everything else. She was someone who introduced me to the Leukemia and Lymphoma Society, which I had signed up for already just because they sent me a bag with a bunch of information. She was the additional push I had to attend some of their support groups.
Chemotherapy
Describe the ABVD chemo regimen
I had ABVD chemo administered to me every other week. The math is a little challenging but they consider two treatments one cycle, so I knew that I needed six cycles. I would have that spread over about six months so every other week.
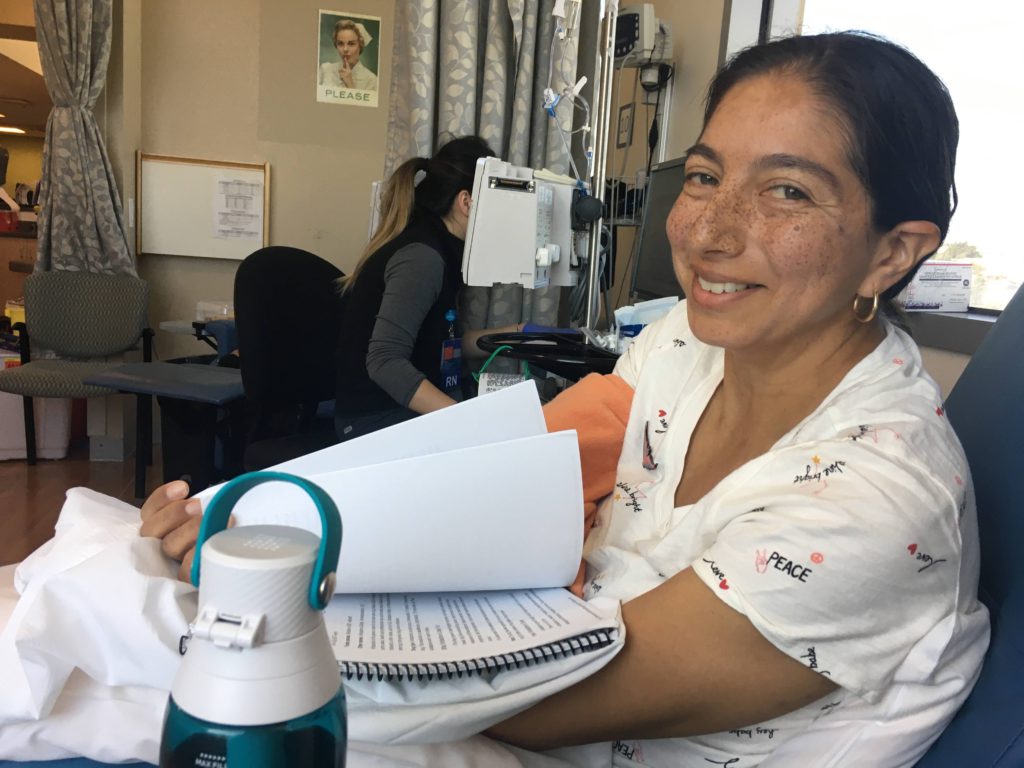
After four cycles, they would do a check for me. ABVD that first appointment, I was going to receive it every other week, and I didn’t know what to expect. It turned out to be only a two- to three-hour appointment.

Deciding to use IV in veins (instead of port, PICC line)
I didn’t choose to get a port, which is when they put in an incision to make it easier for doctors to [administer chemo]. If you don’t have a port or a PICC line, they would have to use the IV on your veins on your arms.
That was a question I immediately asked Dr. Neeman about that option. He did his research for me and said it was recommended that I don’t because they were feeling confident.
If I would end up needing more treatment than what was originally recommended, then we could talk about it. But because he said no, I decided to go through the pain of them trying to find [a vein] each time.
I think out of every appointment, getting the chemo was pretty easy. But it was finding the IV [vein] that always caused a lot of pain. It would cause the most stress at any of those appointments. But getting the chemo itself, no, because they had already found the [vein].
The nurses would administer each of the medicines. They double- and triple-check before they put any medicine in you. Definitely finding the [vein] sometimes would take up to half an hour.
I would have to put a heating pad on my arm, drink lots of water as recommended by the nurses, and do arm weights throughout the week to make it easier for them.
I would joke, “Oh these are bad [veins],” and they would say, “No, it’s just a sign your body doesn’t like what it’s receiving. But it will all be healed!” I trusted them, so I would do anything in my power to make that IV vein find easier.
How long were the infusions?
The infusions were every other week. It would take maybe 2 to 2.5 hours. For the first 2 to 4 cycles, they were going to administer ABVD.
Then they did a second series of tests to see if it was working. They had let me know that it was successful, so they actually removed the bleomycin, the B, from my regimen.
The appointments lessened to no more than 2 hours. Maybe some of the wait made it a little longer, but 2 hours because then I would only need 3 of the chemicals.
ABVD chemo side effects
Summary: fatigue, burst of energy → insomnia, constipation, acid reflux
My first few cycles, it was right away because I would feel extremely tired. The steroids they give you before you take the chemotherapy are to lessen the side effects, to avoid the nausea, some of the really strong reactions that we so often see in movies.
After appointments, those steroids would kick in, because I would have this burst of energy. When I say the side effects hit, it was actually this burst of energy that prevented me from falling asleep. If I had my appointment later in the day, I wouldn’t get much sleep just because of the wiring.

After the third day is when I would feel a little bit of minor side effects of constipation, which is always the worst one, or acid reflux. I would try to avoid those foods that would increase those sensations.
What helped prevent or lessen those side effects?
[For] the constipation, I did reach out to my nutritionist, who gave me some snack ideas. I actually still eat a lot of those snacks now because they’re delicious. I’ve introduced flax seeds into shakes, started drinking a lot more vegetable shakes or fruit shakes.
I also made sure to drink a gallon of water. As disgusting as the taste of water became because of the saline, I still pushed myself to drink water or sparkling water because that would flush everything out.
That was some of the more important things I had to concentrate on to get my body ready for each treatment. Just to make sure all the waste is out of my body from the constipation. Am I drinking enough water to make me feel strong and my veins available?
Describe the hair loss
Summary: When I attended the chemo orientation, I remember the nurse speaking directly to this. She said, “You may not all lose your hair. You’re already going through something traumatic, so don’t feel like you have to shave your head, which is a very traumatic experience for a lot of women.”
My hair has always been something I knew I could easily lose. A lot of people said, “Oh, it’ll grow back.” But it was more than that to me, so I didn’t feel ready, after hearing her say that, to cut my hair. I told myself when and if I feel ready, I’ll shave my head.
One side effect of chemotherapy is loss of hair. Given my limited experience with people who have undergone this treatment, I assumed I would need to shave my head. However, thanks to Kaiser SF providing a chemotherapy orientation class, I learned that that is not always the case.
Unfortunately, I am blank on the name of the nurse leading the orientation class, but I remember her compassion and patience with all of us anxiously awaiting the grim details of treatment during orientation.
It’s all yin and yang. When the topic of hair arose, she let us know that a side effect is losing the hair of our nose, legs, arms, eyelashes and of course head. Basically, any place on our body with hair.
However, she indicated that some of us may not lose as much as others. When I asked her about whether or not I should shave, her response surprised me.
“Some choose to, but if you are worried, why put yourself through more trauma? You’ll know if and when you are ready to shave your head, if that’s what you choose ultimately to do.”
A huge sigh of relief released from me. I had read through blogs that many individuals choose to shave because they felt the need to control, but my initial response is that I needed time.
Part of my identity always included having thick, long and straight brown hair. Over the years, I would find myself losing clumps of hair during moments of stress or for other unbeknownst reasons. But with such thick hair, no one noticed except for myself and my close circle.
Losing hair because of chemotherapy made sense. Losing hair for unknown reasons did not. And given that I chose to treat chemotherapy as a day to day process, I would not rush into shaving my head.
This did not keep me away from the blogs, though. Through FB support groups I belonged to, many would write that they were choosing to shave after the third or fourth treatment, given the amount of hair they were losing.
»MORE: Dealing with hair loss during cancer treatment
Deciding not to shave your head
It never presented itself, but I was losing a lot of hair, and I was okay with that. A week after my appointment, a clump of hair would fall out. But from my experience, it was never traumatic enough to want to shave it.
I had really thick hair. I’d say I lost 80% of it. I felt like it was therapeutic for me to be going through that experience. It was weird, but I didn’t have an issue with the hair coming down.
I strategized a timeline that in the likelihood of losing hair, I would probably need to shave within a month or 2 of treatment. I assumed that my Halloween costume should incorporate a bald character. Thus, my costume of Mr. Potato Head.

Tips for dealing with the hair loss
Looking back, a piece of advice: As it grows back, I’m wearing this (beanie) only because it’s just out of control the way it’s growing back. With the pandemic, I can’t go to a hairdresser, so I do with I had cut or shaved my head so it could grow out more evenly.
But it is what it is, and I chose not to do anything with it.
When Halloween passed, I still had hair on my head and only a few head wraps. I knew I was losing a lot of hair because as the cold rainy season approached, my head became cold more easily. I began purchasing more wraps and styles.
At this point, I still had no desire to shave. The transition between October and November went from baseball and running caps to wraps and beanies. I noticed that I often went with comfort over style with my choices of head wraps for that day.
In 2019 I have made many realizations, and in 2020 I will aim to understand them. My diagnosis has given me the opportunity to take time to reflect and make changes, and more importantly to take the process one day at a time.
»MORE: Read Erica’s blog
Quality of Life
Financial toxicity: paying for cancer treatment
I’m fortunate my husband didn’t need me to work, and I’m fortunate also in looking at short-term disability options. For whatever reason, I had started to invest in my short-term disability insurance a year before.
Dealing with HR was a headache, and I found someone on their side of the customer service. When she heard me be open and honest about what I was going through, she acknowledged that and gave me a lot of resources and information on how to move forward financially with not working. She gave me some tips that were really helpful, even now.
I thought I needed every dollar because I was worried. I was told by my doctor, ‘You’re not going to work.’ I don’t think it’s recommended. They ask if you’re able to afford the cost of not working because they want you to be okay.
I said, “I’m married.” They said, “Good.” My work even acknowledged it. They said, “Okay, good, because we can only cover your health insurance for so long,” which is sad and frustrating in itself.

For myself, I was okay. The HR woman who I caught said, “I’m sorry you’re experiencing that, but I would recommend that you don’t pull out of your short-term disability insurance until the very end, after you’ve exhausted your California disability.”
That’s because they don’t question how you’re going to use your insurance, these private institutions. She said, “They just want you to know it’s okay. Since you do want this vacation with your husband after all of this experience, it would be nice to be able to take vacation and have some means to do it.”
I remember her saying. “Your work’s not going to give you vacation for having gone through this. So this is your vacation. This insurance money is how you’ll be able to afford rent and other pieces that your work won’t do for you.”
I just remember hearing that and being like, “Oh, that’s right. I might have to use vacation from all of this in order to cover myself through appointments, or I’m not going to have any sick time after this.”
She was thinking well in advance for me that I almost sometimes wish I had her name and email to send her a thank you after.
What was the hardest part of the cancer treatment?
There are so many pieces. It’s actually moved me to think more deeply about systems in place for everyone. I was really lucky to have a husband who was able to help me with health insurance. Those pieces matter to bring a sense of security.
I will say there are a lot of resources that I have found in dealing with this that are available to everyone. Resources like the Women’s Cancer Resource Center, which is an agency to help when things start to fall apart.
Not everyone’s going to have every answer for you. It’s important, at least it was for me, to be open and talking about it.
Getting support
I know a lot of people I met didn’t want to talk about it, and when they didn’t, it left me feeling isolated. As a result, I just want people to know that people do want to help.
It is a traumatizing experience to think back and live through, but I also found a lot of people who were willing to help. The community I surrounded myself with, whom I trusted, was also willing to help me find those things when it was hard.

Advice on how to best get support
I got a lot of prayers, and I’m only starting with that because I felt like that wasn’t helpful at times. I remember saying that out loud in the support group I was participating in. I said, “I don’t need prayers.” At that point, I think I needed support in figuring out how to deal with the work situation.
I remember a woman stopping me mid-conversation and saying, “Take the prayers and take any graces from anyone willing to support you, because you never know when you’re going to need it.” I asked her because she was a survivor, “How do I ask?”
She said, ‘People want to help, but they don’t know how so be specific in how you ask, if you can. Ask your husband or whoever is in your very close circle to help you through that.’
So I made my mom and husband — I called them captains of my support group. When I was unable to ask for it, I would talk either one of them through what I was trying to figure out what to ask.
They helped me figure out how to do that and sometimes just did the ask for me, or pushed people away if I didn’t want to be around anyone.
Having captains of a support group is just helpful because they can become your go-to. It’s all about delegating, and initially it’s hard do.
You want to do for yourself, but you start to realize it’s hard to do things for myself, and I do need support.
Final push: self-advocacy is key
I think as women, we assume that we can handle the process on our own, but when dealing with our health, we need someone to walk alongside with us.
It could be a spouse, relative, primary doctor or an organization that can advocate for you when the process becomes stressful. This trusted companion ensures that you are able to ask the questions we may easily ignore or miss because we are processing our own emotions.
During the process of waiting, I immediately sought resources and people and did not completely depend on the internet. I knew that the internet would send me down the rabbit hole.
Instead, I asked questions like, “What is the purpose of this test? Who else has gone through similar experiences that I can openly discuss this with?”
And I took notes. These notes played an important role in how I told my story and conveyed my needs to others. When I went through treatment, I knew that I could easily share my notes with my advocates.
I trusted them to ensure that they would speak on my behalf if I could not with my own voice!
»MORE: How to be a self-advocate as a patient
Last message to other patients and caregivers
I purposefully wore this shirt and this pin. This is how I wanted to end. Sharing that I knew that I was really upset initially with how my case was being handled or how I felt it was being handled, how I had to coordinate everything.
For me, getting angry was making me physically hurt more.
I remember I started to change my mindset, and even if I didn’t feel it, I would pretend to understand with caring and kindness and empathy. I started wearing things that would remind me. A shirt I wore to some of my first chemotherapy appointments says, “Shine bright, love, peace.”
I also wore this pin from the movie “Coco” just so I knew that there are good people out there, that there are graces. That will help me get through it even when sometimes I wasn’t believing. What ended up happening was a lot of the nurses would [say], “Hey, I love your shirt or your message!”
And they would be that person for me on that day. Or someone else, if I was going on an errand, would be that person to stop and say, “I really like your smile” because I found myself smiling more.

Even though I never cried before, now I say I cry all the time because it’s important to allow yourself to feel whatever emotion you feel.
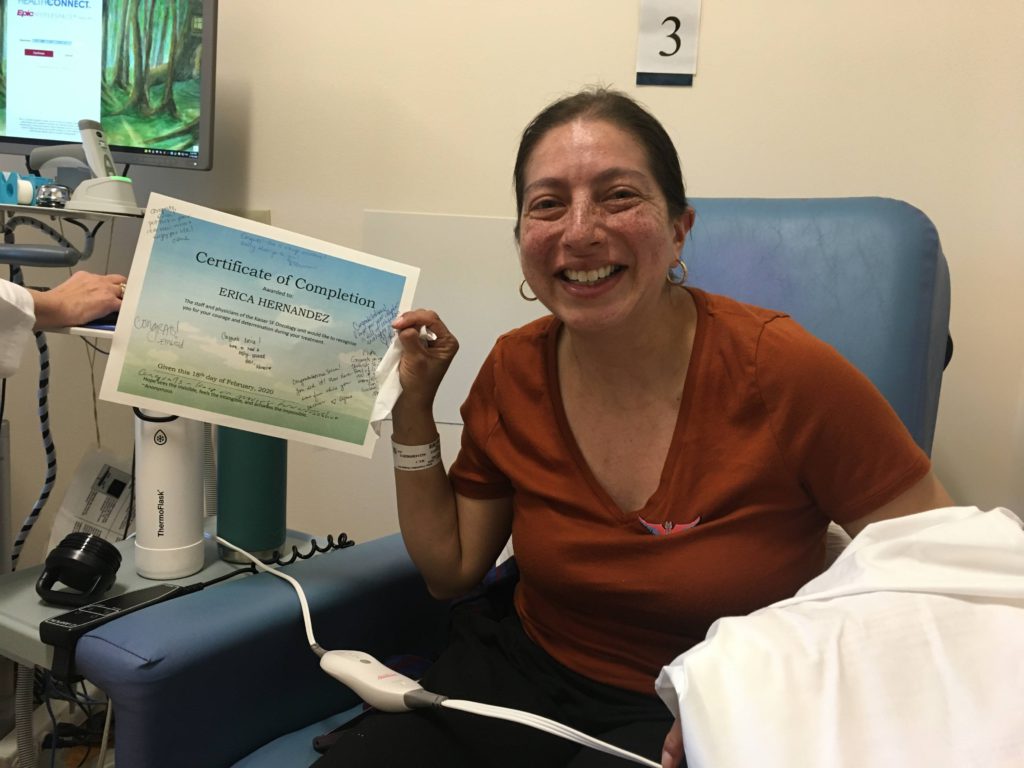
I received the news of remission on March 2nd, which is the time the pandemic hit. The moment I thought I was going to go out to “seem normal again,” I was asked to stay inside and shelter in place. [That] has been my existence since September.
When you go through chemotherapy, you’re asked to be careful about where you go and how you take care. I have cried a lot, and I’m accepting of those tears. I realize that when I cried, it was the realization I had to stop and acknowledge that. Sometimes those around me don’t understand, but I know I’m okay.
I write, and because of the other support groups and other people I have found, I now have a larger community that I can go to. Hodgkin lymphoma was so unknown to me. I knew nothing about it.
Google did nothing for me. It only threw a lot of information at me, but it was only when I started to talk to people or write down questions and ask my doctor that I really started understanding that it’s very treatable. It’s still cancer, but it’s very treatable. There’s a lot of advanced treatment and a lot of hope in this field.
I’m hopeful in the next 5 years the treatment’s going to look very different from what I went through, so we have to continue supporting these places that have been able to advance this.

Inspired by Erica's story?
Share your story, too!
Classical Hodgkin’s Lymphoma Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)