Katee’s Stage 2B Classical Hodgkin’s Lymphoma Story
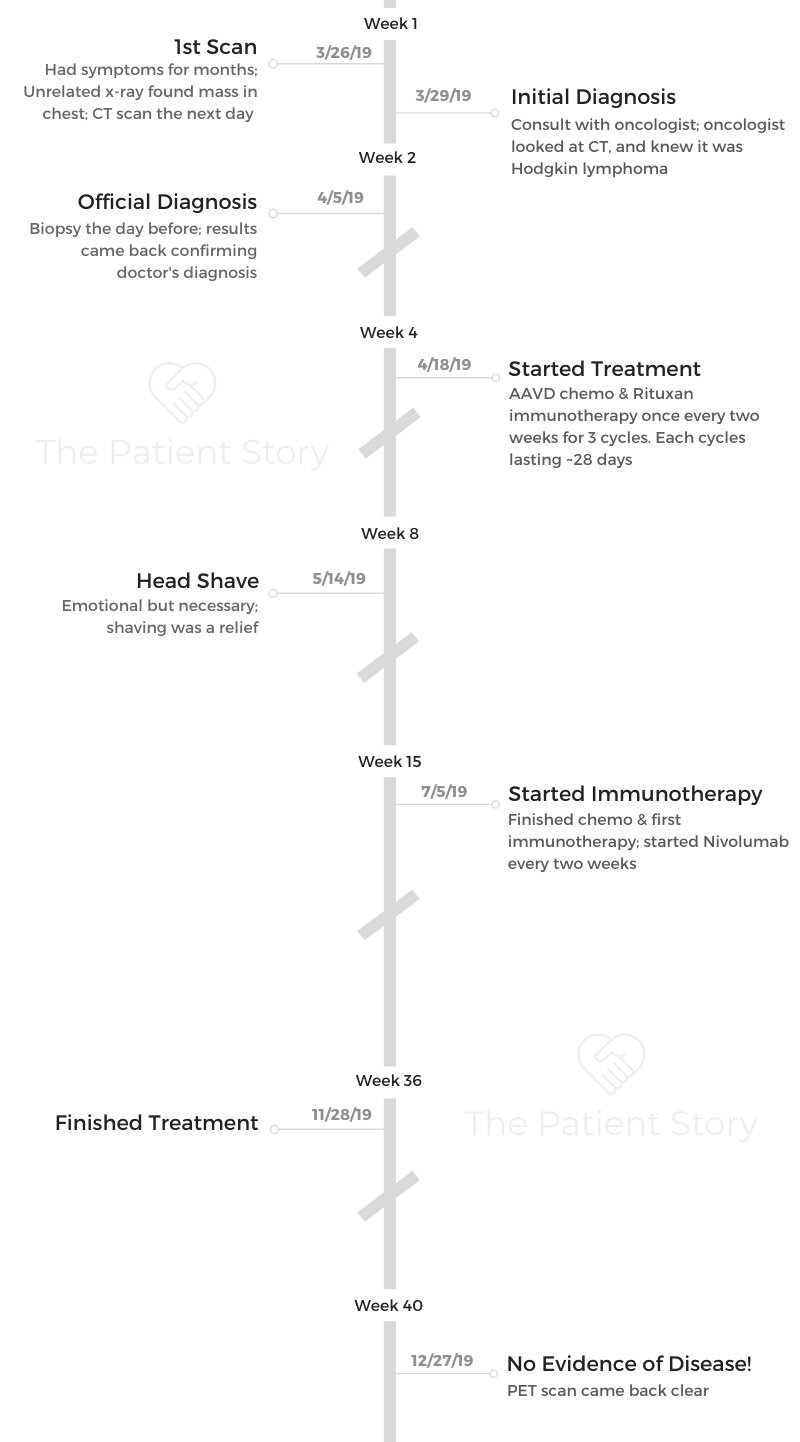
Katee shares her story of stage 2B Hodgkin’s lymphoma, undergoing AAVD chemo under a clinical trial, then immunotherapy until getting results of no evidence of disease (NED).
She also highlights how she got through losing her hair after from chemo, parenting with cancer, and the impact of a diagnosis on her marriage.

- Name: Katee P.
- Diagnosis:
- Staging: 2B
- 1st Symptoms:
- Night sweats
- Extreme itchiness
- Persistent cough
- Fatigue
- Treatment:
- Clinical trial:
- Targeted Therapy + Chemotherapy
- 3 cycles = 6 infusions of A+AVD
- Adcetris (brentuximab vedotin) – targeted therapy
+ - Adriamycin (doxorubicin)
- Vinblastine
- Dacarbazine
- Adcetris (brentuximab vedotin) – targeted therapy
- 3 cycles = 6 infusions of A+AVD
- Targeted therapy
- Brentuximab concurrently with chemo
- 8 cycles of nivolumab, doses every 2 weeks
- Targeted Therapy + Chemotherapy
- Clinical trial:
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Emotionally, you’re going to be all over the place. You just have to deal with 1 day at a time. When you have a good day, enjoy the whole day.
The number 1 thing is to stay hydrated. It sounds so silly, but I learned the hard way. Stay hydrated!
Katee P.
Diagnosis
What were your 1st symptoms?
I had symptoms for probably more than a year before I found out what it was. I own a business with 36 employees and have 3 children, so every symptom had an excuse.
I thought the night sweats were perimenopause. I had extreme itching to the point where I would bruise my legs.
I did go to the doctor, but the doctor thought it was just a laundry detergent change or something like that. I started rubbing Benadryl cream all over my legs like it was lotion one night, and I looked at my husband. I said, “I know what this is. It’s anxiety.”
I had a constant, persistent cough as well. I thought it was allergies. I had an excuse for everything. I went to the hospital twice.
The first time, they didn’t even test me for the flu. It was going around, and they said that’s what it was. The second time, they told me I had viral meningitis.
I have to believe everything happens for a reason, though, because had I gotten diagnosed when I went to the hospital the first 2 times, I wouldn’t have ended up in the clinical trial I got into.
»MORE: Hodgkin’s lymphoma patients share common first symptoms

How did you get diagnosed?
I got diagnosed because my husband and I were at a bat mitzvah for one of our friend’s daughters. The DJ had us doing a dance that 40- or 50-year-olds should not be doing ever! We all fell on the floor. Every one of us.
When I fell, my husband dove across the floor to catch my head because he thought I was going to hit my head.
He ended up accidentally kneeing me in the ribs. It knocked the wind out of me. I was like, “You just broke my ribs.” He was like, “I did not!”
I had to take a trip the next day. I had to fly right out to Georgia to teach a class and come right back. I couldn’t pull my suitcase through the airport because my ribs hurt so bad.
Then I got home, and I was at work. I was like, “I have pilates class later. If I have broken ribs, I probably shouldn’t do that.” I ran down to a MinuteClinic down the street from my salon.
The doctor said, “You need to go for a CT scan.” I was like, “How bad are my ribs broken?” He said, “Well, we can’t really tell because there appears to be a mass, but it’s an X-ray, so you need a CT scan.”
I had the scan the next day. I knew something was really wrong when I left the CT scan.
In another life, I worked at Memorial Sloan Kettering. I know what a CT scan isn’t supposed to look like.
That was on a Tuesday. By Friday, I already had my biopsy done, and we knew it was Hodgkin lymphoma.
Processing news of the diagnosis
I had known something was very wrong after the CT, but I didn’t know what it was. I thought it was in my lungs.
I called my old boss at Sloan. I asked him where I was going. He told me to come to Hackensack Medical Center, so I went there.
They got my scans done. The doctor there was so brilliant. He held up the scan and he said, ‘You have Hodgkin lymphoma.’
He didn’t even need a biopsy to know. We still did the biopsy the next day. He was right. It was Hodgkin’s lymphoma.
»MORE: Patients share how they processed a cancer diagnosis
Describe the fine needle aspiration biopsy
I was awake. It didn’t hurt. I heard it hurts, but I just felt pressure. They numbed it, and it really wasn’t bad.
What was your treatment plan?
I was supposed to start chemo the next day. I went in all ready for it. Then they said they were going to put me in a clinical trial instead.
Because my mass was in my chest and up in my neck, they were worried about me needing radiation afterwards.
There was a 25-times-higher chance that I would develop breast or lung cancer with that. The clinical trial allowed me to do chemo and immunotherapy, which prevented me from needing radiation.
Clinical Trial (Different Chemo Regimen)
Did you get a port?
Chemo was horrific for the first infusion. I didn’t have a port. One of the chemo drugs burned when it was going in.
I had the most incredible nurse. This woman wrapped my arm in heating pads, sat next to me the whole time, rubbed my arm and my leg, and cheered me on. I can’t say enough about her. She was amazing.
I insisted on a port after the first infusion. It was like night and day after that. I still have the port. I’m hoping to get it removed soon, but yeah, it helped so much.
What was your clinical trial?
The clinical trial was A+AVD chemo, brentuximab, and nivolumab.
I had 3 cycles of chemo and then 8 cycles of nivolumab. They gave me the brentuximab (targeted therapy)with the chemo.
I got nivolumab once every 2 weeks. That was an infusion as well. I still had to spend all day at the infusion center, though, because you have to wait for the doctor and get your labs and all that.
The way the trial was set up was for me to do the 3 months. At the end of that, I’d have a PET scan. If that came back clear, we would go right to the 8 cycles of nivolumab. If it wasn’t, you had to do 4 more cycles of brentuximab.
Fortunately, I came back from the PET scan as no evidence of disease.

How were you feeling going into your first chemo?
The trauma of having cancer didn’t really hit me until very recently because when I was diagnosed, I went into survival mode.
I have 3 kids. I was like, “We have this. We’re going to be okay.” I was in a battle. I didn’t really process the emotional part until later, and I’m still working through some of that now.
When I went into chemo the first time, I was just ready to do it. The hardest moment was going to meet my doctor for the first time.
I saw the scan, but I still had a small part of me that thought, “Maybe I have pneumonia. Maybe it’s phlegm.” That’s not what it was. He diagnosed me then.
They wanted me to go back downstairs to get my labs. All these people I was walking by looked so sick. I went in, and I started to panic.
I said, “I’m not ready to feel sick right now. I need a few weeks to process this. I feel fine right now.” My friend that I used to work for at Sloan calmed me down. From then on, it was just time to get going.
What side effects did you experience?
The first thing I did was join a support group on Facebook. The responses were so varying. Some people in the group were saying they worked through it, and some were saying they were hospitalized for chemo.
I didn’t take chemo very well. It knocked me off my feet.
- I could get up and walk around the house around Day 6.
- By Day 8, I’d start to feel a little better but dizzy all the time.
- On Day 13, I’d feel great, but then it was time to go back in the next day.
The first side effect came when I woke up 2 days after my first infusion. I woke up, and I felt fine. I was like, ‘Okay, I can do this.’
That was great, but then the next day, I woke up, and I felt awful. I was dizzy, light-headed and nauseous.
I felt like I got hit by a bus. I was in the bathroom because I felt like I might throw up. My husband ran out to get a trash can, and when he came back, he found me on the ground unresponsive. From what he says, he was shaking me and slapping me, and I wasn’t responding.
I don’t really know what happened, but I think it was a combination of dehydration and low blood pressure. The chemo was a little too much for me, so they did have to adjust my dose a bit. That’s how I learned I absolutely had to stay hydrated.
Everybody tells you to stay hydrated. I don’t think I knew what that meant. Drink your 6 to 8 glasses of water. It will make a tremendous difference.

When did you find out you were NED?
I had a scan on December 26th. On the 27th, they confirmed I was still in remission, which was great.
I had a cough again, so I was getting nervous. I had prepared myself for the news. I would be lying if I said I didn’t spend the holiday season thinking that it was back.
When I went back for my scans, I was prepared and okay, but the thought of having to sit my kids down and tell them it wasn’t really over yet was horrifying.
A year and a half before I was diagnosed, my daughter, who was 11 at the time, had a best friend who died by suicide.
My kids’ childhood has been interrupted enough times already. I’d like them to be able to finish their childhoods without any more trauma.
That was really killing me through the holidays. I didn’t want to take away more of their innocence. That was the best part of finding out the news on the 27th.
Family & Support
How did you talk to your kids about your cancer diagnosis?
They were 12, 10 and 8. Our kids hate when we have to sit and have a conversation because it’s usually bad news. That’s what we did. We may have gotten them out of school early.
We sat them on the couch. We just said, “This happened. This is the prognosis. It’s going to be hard, but everything is going to be okay.”
We basically told them that Mom was going to get sick for a while, but that it was okay because I had to get sick to get better.
Managing cancer while parenting
I checked out for those 8 months. I did as best as I could, but thank God for my in-laws. If they hadn’t been here, I don’t know what we would’ve done. I could not be present.
I’m a beach girl. I’m outside all summer. My kids are beach kids. I went to the beach twice. I had to hide under an umbrella the whole time. It was awful. I didn’t get to experience things like that with them for that time.
We just took a trip to the Keys, and it was so great. I was in the sun all day for days, and I wasn’t sick.
Cancer didn’t take that from me.
I tried to be present for them, but I think I checked out. My kids may feel like I was there, but I don’t know. This experience forced them to slow down, so in some ways it was cool. I couldn’t get off the couch, so they would come lay on the couch with me.
I was there, but I do feel like I missed out. I couldn’t be there for my son’s last day of elementary school because I was getting chemo. That’s rough, but I hope they look back and understand.
»MORE: Parents describe how they handled cancer with their kids

Advice for other parents dealing with cancer
Use your village. Take care of yourself, because otherwise you’re going to be useless to everyone.
If you have a support system, use them. I had friends set up a meal train. I didn’t cook for months. It was so much help. Plus, if I was well enough to sit up at the table, it allowed us quality time as a family.
What were some ways that people helped you?
I am 1 of 5 siblings. My family was great. My husband was superman. I expected nothing less of him.
My kids are athletic, so having people to drive them to their stuff was huge. My in-laws and friends and everybody just stepped up so much.
The kids’ lives went on just about like normal because of that. Of course, the meal train was helpful. Things like that really do make a difference. Little things add up. You don’t have to do anything huge.

Cancer’s impact on your relationship with your husband
We’ve known each other since we were 12. We’ve always gravitated back to each other. We finally got it right when we were in our 30s.
Emotionally, I think it brought us closer than any 2 people could be. We hung onto each other for dear life.
Physically, it took a while because he thought he was going to hurt me, and I had to convince him that I wasn’t going to break.
Also, him seeing me unresponsive traumatized him. He thought I died. That took him months to get through.
On an emotional level, nothing could’ve connected us more.
Everyone says, “In sickness and in health,” when they get married, but we lived that out. He rose above and beyond.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
Reflections
Describe the hair loss
The hair loss is such a huge thing. I’m a hairdresser. I’ve done it for 24 years. It was ironic for me to be the one to lose it.
Well-meaning people, and I think I was one of them before this, say really stupid things — mainly, “It’s just hair.”
It’s not just hair. What a horrible, insensitive thing to say to somebody. It’s a part of you.
As a hairdresser, I tell people all the time, ‘You don’t realize, but if your hair looks amazing, you feel great.’
I actually felt more comfortable being bald than I do with a pixie cut as it grows back out. When I was bald, people looked at me and knew I was going through cancer. With this pixie cut I have, it looks like a choice.
It was not a choice. When a woman chooses this, it’s empowering. I would not choose this, though. It’s just hair? Really? Let me grab your head and just cut all yours off.

It’s hard to walk by a mirror and not recognize yourself. I’m still having a really hard time with that, and I’m sure people around me are like, “Get over it,” but it’s hard.
I was prepared for it to fall out. What I wasn’t prepared for was waking up with hair in my mouth and my eyes because it was falling out in my sleep. Then I’d go brush my teeth, and it’s all in the sink when you spit.
I let it go for 4 days, and finally, I had my business partner shave it.
I went into my salon, and my hair was hurting. It feels so heavy on your head, and I was ready to just get rid of it. Everyone was trying not to cry, but when she started shaving, I felt relieved.
That was a liberating moment. It was harder for the people around me than it was for me. Being bald wasn’t as bad as I thought it would be. Growing it out again is what’s tough.

How has cancer changed your perspective?
You have to change something about your life. During treatment, your main goal is to go back to your life.
When you’re done with treatment, you realize that something has to give.
For me, I have a very stressful, busy life. I’m a lot more selfish now, but I feel like I have more empathy and compassion than before.
I’ve learned that sometimes even if it’s painful, you have to cut the negativity out of your life. I really believe it will make you sick if you don’t.
We all think we’re going to make it to 80 or 90, but you could get sick well before then. If you have a crappy job, get a new one. Life is too short to stay in stressful situations and situations that are making you unhappy.
I don’t stress about finances as much anymore. I’m not gonna go up to my ears in debt, but if I want to take the trip, I’m taking the trip. I have 6 trips planned in the next 6 months.
Message for someone who’s just been diagnosed
Get as much education for yourself as you can.
Join an online support group.
Try to take things one day at a time.
Emotionally, you’re going to be all over the place. You just have to deal with one day at a time. When you have a good day, enjoy the whole day.
The number one thing is to stay hydrated. It sounds so silly, but I learned the hard way. Stay hydrated!

Inspired by Katee's story?
Share your story, too!
Hodgkin’s Lymphoma Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)