Helicon’s Stage 2A Classical Hodgkin’s Lymphoma Story
Helicon was diagnosed with Hodgkin’s lymphoma at 37 years old. Explore his story, including undergoing ABVD chemo, side effects, radiation and the importance of getting support through the experience.

- Name: Helicon K.
- Age when diagnosed: 37
- Diagnosis:
- Hodgkin lymphoma
- Stage 2A
- 1st Symptoms:
- Difficulty breathing led to surgery to remove swollen adenoid tissue
- Found Hodgkin’s lymphoma cells in adenoid tissue
- Tests & Biopsies:
- CT scans
- Echocardiograms (heart)
- PET scans
- Pulmonary function test (lungs)
- Blood work before every treatment
- Treatment:
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Do not lose heart. Fight, and open up and invite others to journey with you through this battle.
Helicon K.
Diagnosis
How did you get diagnosed?
I was planning to go on a mission trip to northern Iraq to minister the Yazidi people, who were being victimized by ISIS. Before I went, I decided to do a procedure to remove a blockage in my nose that was giving me difficulties breathing (swollen adenoid tissue).
I had set an appointment to have some of my adenoid tissue removed, as it was causing that blockage in my nose that was affecting my breathing.
I had an incredible hard time breathing through my nose (near 90 to 100%) blockage, which led me to seek the ear, nose, throat (ENT) doctor to take a look.
As a result, I had the ENT in Santa Barbara diagnose the issue and help by having a simple procedure to remove the tissue. When they removed the tissue, he found some of the tissue suspicious and, as a result, sent it in for a biopsy.
It was through this surgery that they first discovered Hodgkin’s lymphoma cells in the tissue removed from my adenoids. Before that, I had no idea that I had Hodgkin’s lymphoma.

List the tests and biopsies you had to undergo
- CT scans
- Echo cardiograms (heart)
- PET scans
- Pulmonary function test (lungs)
- Blood work before every treatment
How did you decide where to get treatment?
My ENT (ear, nose, throat) doctor that did my surgery/biopsy recommended me immediately to an oncologist.
Did you get a second opinion?
I did not get a second opinion since my ENT was the best in Santa Barbara county and I trusted his assessment, which was then affirmed post-scans by my oncologist.
What did you like about being at a smaller or bigger place for treatment?
I was very fortunate to have been treated in Santa Barbara because the medical facilities are quite well done. Since Santa Barbara is a very affluent place, there was quite great medical care provided in a small city environment.
Any advice to others about where to go for treatment?
I always tell others to never underestimate where you get your treatment and to not be hesitant to spend a little more for the best care you can receive.
I had the best ENT surgeon in Santa Barbara take care of my nose issue, and that helped me find out about my cancer. My oncologist was incredibly talented and helpful.
How was your medical team?
My medical team of ENT, oncologist, primary care physician and radiologist, as well as the physician’s assistants and nurses that cared for me, were great and very helpful. My nuclear medicine techs and nurses were fantastic, too!
Treatment (Chemotherapy)

Describe the port surgery and experience
The port was in my body from my first day of chemo till about early January, when I had it removed.
The surgery putting it in was a simple process where they used local anesthesia to cut a spot on my chest near one of my main veins and install a port that would run the chemo drugs directly into my system.
Early on, having the port was a pain in the butt due to the wound needing healing, but having it was helpful since it meant less invasive vein shots and most of my medication being administered through the port.
I could not do any lifting or sports that could affect or damage the port (which is a bummer), but I felt it was quite unobtrusive after the wound healed.
On a side note, the removal of the port was a bit painful, as my flesh grew around the port and it was pretty secure. It’s all healed now, though sometimes I get very minor irritations or stings randomly.
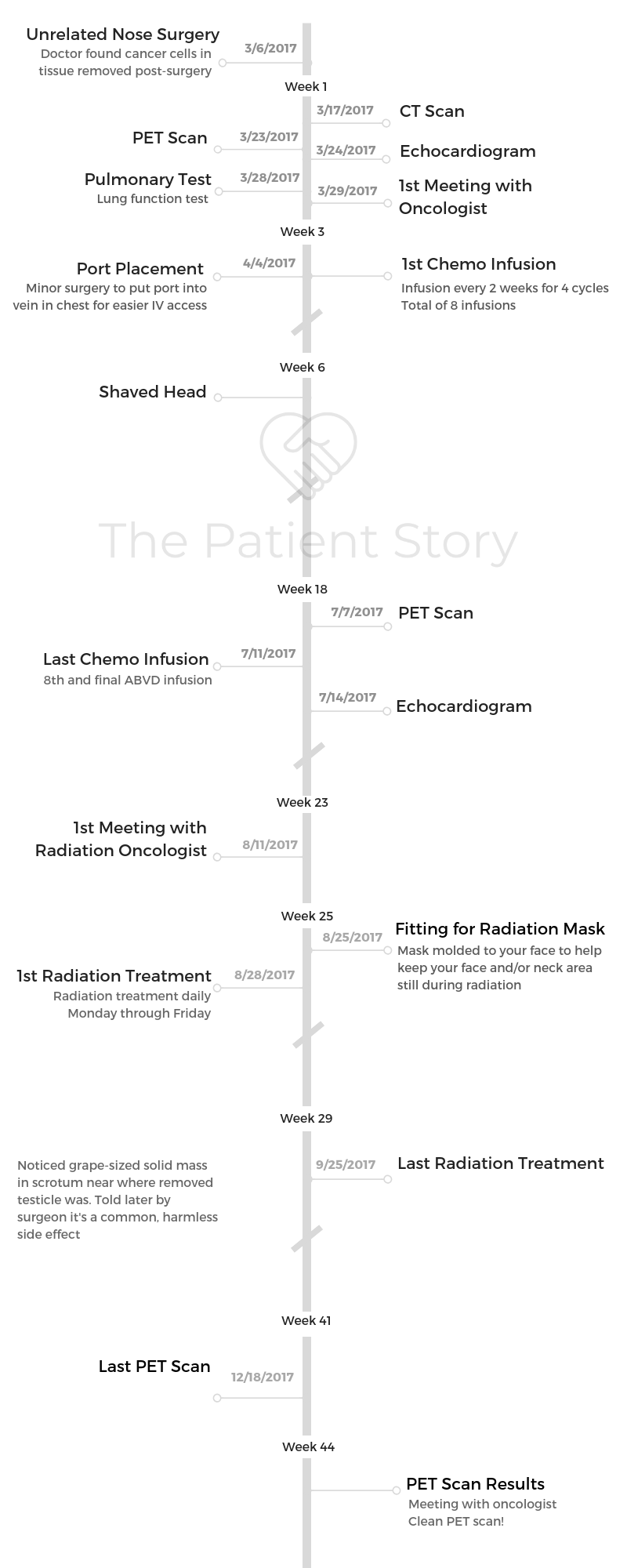
ABVD chemotherapy
I went through a standard ABVD cocktail to treat my Hodgkin’s lymphoma. I did 4 cycles of biweekly (every 2 weeks) treatment, totaling 8.
Describe each chemo cycle
I think how my oncologist planned it was to have one treatment and then to let the chemo run its course for a week, and to give me a week for my body to recover. Then another treatment would be given, and the cycle would be repeated.
At first, there were not many effects except feeling incredibly tired, exhausted, and my body fighting against the treatment with all it had.
After my second to third treatment, I began to lose my hair, which prompted me to shave my head so that I could decide when I lose my hair.
As the cycles progressed, my body took longer to recover, and I found my body getting weaker and weaker after every subsequent treatment.
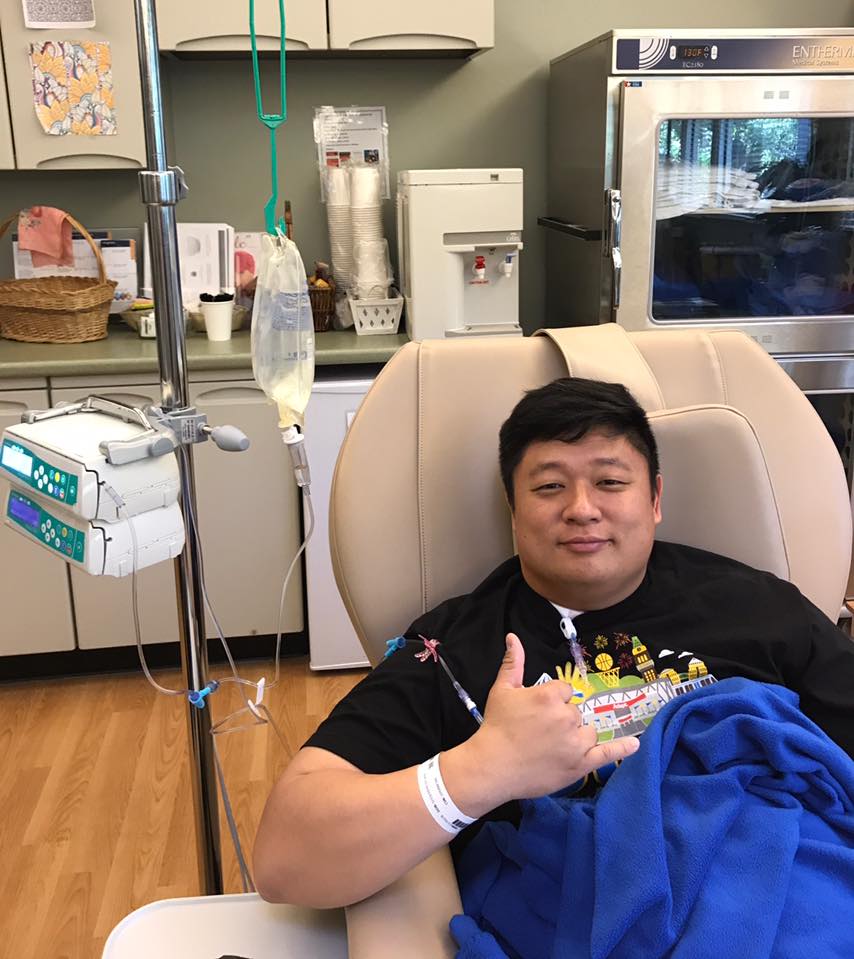
I also started to experience tingling at the fingertips, sensitivity on my nerve endings (neuropathy), and my nails getting darker as the treatments progressed.
My thought is that my body was fighting every time, and as time passed, the subsequent results were a heightened sense of potential for nausea and definitely lack of energy.
What was Cycle 1 like?
Cycle 1 was not too bad, because I think it just felt like getting sick, and I was in pretty good shape when I started treatment.
It was only hard since I was not sure what each step would require. The onset of being tired and needing a lot of rest threw me off a ton.
What were the side effects of chemo?
- Hair loss: I shaved my head before I lost all my hair. I’m guessing I’d probably have thinned out but not lost all my hair, but I did not want my cancer to determine that.
- Neuropathy: Mostly just my fingertips felt a bit of tingling.
- Fatigue: I slept a lot 2 to 3 days after treatment.
- Black-spotting: Spots of black showing up on the bottom of my feet and even in my nails.
- Heightened sense of smell: My sense of smell was exceptionally heightened, and I would be grossed out by certain smells that had a “metallic” hint to them. I joked I was Wolverine during those times.
- Nausea
- Some chemo brain
What helped you avoid or get rid of those side effects?
Overall, my family support, my church community support. Very clean eating of simple foods and just being mindful of not being around sick people and or just following every recommendation of my oncologist.
For nausea, an amazing new FDA-approved drug called Varubi (rolapitant) that helped suppress much of my nausea. This drug was used by our cancer center, and it was one of the best things because it probably kept my nausea suppressed to 10 to 20%, though I got nauseous at the end of 2 weeks.
This drug was very expensive, but I was sponsored by the company that makes it, and my cancer center was willing to give me samples if needed to cover it.
Also, avoiding things that the moment I noticed getting nauseous, I would steer away or stop using those things.
»MORE: Cancer patients share their treatment side effects
Were you surprised by your reaction to losing hair?
No, I expected it, but I was hoping it wouldn’t be lost so quickly. I used to make jokes about balding people, but the moment it started happening to me, I realized how painful it was to lose it against my will.
I did not realize how heartbreaking it was to lose my hair till I started to lose it.
The only thing that helped me was I saw a clip of a young girl going through cancer treatment where she had her hair shaved before she lost her hair.
I thought it was a great thought to not let cancer decide when my hair is lost, but for me to shave my head on my time.
F*** cancer. It does not get to determine my hair loss; I do!


What helped with the hair loss?
Many friends sent me caps, and now I have over 20 to 25 baseball caps and hats of all kinds.
»MORE: Dealing with hair loss during cancer treatment
Radiation
Describe your radiation cycle
I did radiation for 20 treatments: Monday through Friday for 4 weeks. I had a half-dose of it since I was so early stage and chemo had basically taken all my cancer.
Radiation side effects
I did get a little nauseous, but mostly I was fatigued. The worst was losing my sense of taste for over a month. I also got very little saliva output, and I know long-term there will be teeth and mouth issues due to the radiation’s effects on my bones around my neck’s lymph nodes.
How did you deal with the radiation side effects?
I didn’t eat a lot; I just ate to live. But it felt like losing the color of my life. I was scared I’d lose it permanently.

»MORE: Read other patient experiences with radiation therapy
What scans did you undergo, and how frequently?
I did a CT scan before with iodine, some sort of radioactive isotope before radiation and after chemo, and after my radiation treatment to check to see if there was any more cancer (there wasn’t!).
How long did you have to wait for results?
To me, the waiting can be so maddening. Fortunately, my oncologist was always willing to schedule me in as soon as possible.
Still, the weeks of waiting could be incredibly stressful and discouraging. I also had a great community and my family to support me through these times, and definitely a huge part was played in trusting God.
»MORE: Patients describe dealing with scanxiety and waiting for results
Finances
Could you work through treatment?
I worked through treatment at a diminished capacity. I’ve always been a workaholic in ministry, 60 to 80 hours average, but during my cancer I was down to 10 to 30 hours, depending on the week.
If I was on cancer treatment, then I would only work as much as my body allowed, but when I could, I would work.
I was not going to let cancer f***ing decide my life. It was my way to say f*** you to cancer.
Come to think of it, I’m very fortunate to be in a job as a pastor that allowed me much flexibility in my time. I was also fortunate that I had allowed myself an out by preparing and having so many capable people around me that took on my slack during that time.
»MORE: Working during cancer treatment
Financial toxicity: paying for cancer treatment
It was scary, but I come from a family that is financially secure. During this time, my church actually covered most of my out-of-pocket expenses, and my insurance covered the main portion.
I took on some debt, too, but I felt it was right to pay some of it myself, especially as a poor pastor (laughs).
I also had a great financial person from the cancer center that championed for me for whatever discounts or grants that would diminish the cost.
Did you have help?
Yes, I had a ton of help. Church, friends, and family — every area of my life, I tapped and sought help. It really mattered.
What do you wish you had known to help with the financial process?
I am grateful that treatment is possible. We should always have a good insurance plan to help.
Emotional & Mental Support
Were there any big surprises during treatment?
I didn’t realize I would make such great friends among the fellow patients being treated and how dark our humor could be — how we could laugh so much in the face of discomfort and the painful effects of treatment.
What was the worst part of treatment?
The toughest times were always right after the treatments and not knowing how much worse the body would be.
This was scary, and the fear of having permanent “chemo brain” damage to my brain. Another very tough time was when my physician’s assistant misread my results of my CT scan and thought I had to go through another 2 months of treatment. This almost broke me. I think that was horrible.
I think during the radiation, what was worst was the bolting down of my head so that my head was immovable. This sense of claustrophobia and immobility was incredibly scary, and I often would just pray and hum in my head during the 10 to 15 minutes of radiation.
The mental and emotional was worse than the physical.
The unknown, the waiting, the unsureness of the future were all moments of maddening frustration, but it was also lessons in prayerfulness and patience.
What got you through the toughest times?
What got me through these times again was mostly my faith in God. For me, as a Christian, I always tell people that your faith is all a theory till it is tested in the crucible of life and suffering.
For me in the midst of my suffering, my faith really boiled down to two options. Do I believe in God and his enoughness in my life? Or do I believe that I just got a horrible misfortune in my life?
In the midst of it, I found a God that brought a community of amazing people from my family, to my friends, to my church community, to the fellow cancer patients, to the medical care staff. Every step of the way, I felt I was never alone.
It made my suffering comforting as I spent much of my time in prayer and in reading the Bible. Many places, it became very real to understand the suffering and pain in the stories, too.
There’s more to say, but I also realized that we are never meant to be alone on these journeys and that we are not meant to be isolated or on an island.
It really takes a community and others to help us heal and recover, and that was something that I found great peace in.
What were the moments you felt the most sense of community?
Yes, I wrote for others to share what God was teaching me, but also to document the ups and downs and my struggles with faith and belief through the process. I felt that if this was gonna be a moment that changed my life, then I would want others to walk with me through it.
I did not want to walk through it alone, and I felt others could relate (if not then, maybe one day in the future). As a result of some of my writing (via Facebook page), some Chinese people translated it into Mandarin. It was shared with many Chinese people in China through a church setting.
I have heard that it brought many others comfort and courage to face their own treatment to hear my thoughts and insights. I also saw a few of my friends come to a personal faith in Jesus Christ during this time as they were experiencing suffering. My sharing with them and experience really challenged them to consider their lives and existence.
I was also able to partner with Adapt Clothing and (founder) Evan Lessler to release the “Heliconquer” shirt to fundraise for the blood cancer non-profit Leukemia & Lymphoma Society. We were able to raise thousands of dollars for cancer research to LLS.org, and I have become a person that loves to talk to others that are going through cancer or illness.
»MORE: Cancer organizations and nonprofits

Advice to others on how to get support
I encourage people to allow others in to their fears and anxieties, and to not have to be stoic or strong.
It’s okay to need help and to be weak. It doesn’t mean you are weak. It just means you need people to help you. That’s not a bad thing. It allows them to come alongside and journey with you through a time. This is what friends are for, right?
They are there for the tough times, so it’s important to be patient and gracious to their ignorance and even sometimes insensitivities, because I think it meant so much more that they were trying than anything.
How important is it to have caregivers?
This is one thing that I wish I had more of.
My mom was with me for the first time, but this was the hardest part: living on my own. Fortunately, my church often had a meal train going for the week after chemo to help me with my dietary needs in the week right after treatment, so I did not have to cook on my own.
Message to other patients
To not lose heart. To fight, and to open up and invite others to journey with you through this battle.
If they want to ask me more, I’d love to share more in person. I can share even all my writing from my time during cancer.

Inspired by Helicon's story?
Share your story, too!
Hodgkin’s Lymphoma Stories
Madi J., Hodgkin's, Stage 1B
Cancer details: Most common and most treatable form of Hodgkin lymphoma
1st Symptoms: Shortness of breath
Treatment: 3 rounds (6 infusions) of ABVD chemo
Danielle D., Hodgkin's, Stage 2
Cancer details: Diagnosed at age 25
1st Symptoms: Swollen lump on right side of neck/chest area, continued to grow
Treatment: ABVD chemotherapy (3 cycles = 6 infusions)
Lani S., Hodgkin's, Stage 2
Cancer details: Tumor pressing on heart
1st Symptoms: Appendicitis led to CT scan that found tumor
Treatment: ABVD chemotherapy, 7 cycles
Jason F., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 39
1st Symptoms: Itchy legs, bloated face and “upper trunk,” slow-healing wounds, asthma worsened
Treatment: 6 cycles (12 infusion) ABVD chemo, 18 radiation therapy sessions
Logan A., Hodgkin's, Stage 2A
Cancer details: Diagnosed at age 15
1st Symptoms: Lump in neck & fatigue
Treatment: 4 cycles of ABVE-PC chemo
Helicon K., Hodgkin's, Stage 2A
Cancer details: Found lymphoma cells in adenoid tissue
1st Symptoms: Difficulty breathing with blockage in nose, surgery to remove tissue resulted in discovery of Hodgkin lymphoma cells
Treatment: ABVD chemotherapy (4 cycles), radiation (20 sessions)
Lauren C., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 23 years old with nodular sclerosis, relapsed after 6 months of 1st-line treatment
1st Symptoms: Itchy body, enlarged lymph node over collar bone
Treatment: ABVD chemotherapy and ICE, radiation, and stem cell transplant for relapse
Wade W., Hodgkin's, Stage 2A
Cancer details: Diagnosed at 18 years old
1st Symptoms: Enlarged lymph nodes (around neck), diagnosed at 18 years old
Treatment: ABVD chemotherapy (2 cycles), AVD chemotherapy (4 cycles)
Moe C., Hodgkin's, 2B, Relapse
Cancer details: Diagnosed at 19, relapsed before remission
1st Symptoms: Fatigue, weight loss, night sweats
Treatment: ABVD chemo, DHAP chemo, MINE-R chemo, splenectomy, autologous bone marrow transplant
Fabiola L., Hodgkin's, Stage 2BX
Cancer details: Stage 2 with bulky disease, relapsed after 1st chemo. Remission after 2nd chemo & bone marrow transplant
1st Symptoms: Shortness of breath, dry cough, fatigue
Treatment: ABVD chemo (6 cycles), IGEV chemo, bone marrow transplant, BEAM chemo, brentuximab
Stephanie O., Hodgkin's, Stage 2B
Cancer details: Stage 2 with bulky disease
1st Symptoms: Shortness of breath, dry cough
Treatment: Stanford V chemotherapy (12 weeks, 1 infusion each week), radiation (20 days)
Chelsea B., Hodgkin's, Stage 2B
Cancer details: Diagnosed at 32
1st Symptoms: Lump in neck
Treatment: ABVD chemotherapy
Katee P., Hodgkin, Stage 2B
Cancer details: Accidentally found in x-ray after months of symptoms
1st Symptoms: Night sweats, fatigue, extreme itchiness, persistent cough
Treatment: AAVD chemo, clinical trial w/brentuximab (Adcetris) + nivolumab (Opdivo) immunotherapy
Mara T., Stage 2BX (Bulky)
1st Symptoms: Shortness of breath, back pains, daily migraines
Treatment: 3 rounds of ABVD, 3 rounds AVD, Radiation
Topics: Self-advocacy, mental health
Jade B., Hodgkin, Stage 2X
Cancer details: Diagnosed at 21 years old
1st Symptoms: Itchy legs and feet
Treatment: ABVD chemotherapy (4 treatments), AVD (remaining treatments)
Tylere P., Hodgkin, Stage 3
Cancer details: Mother is a nurse practitioner; suspected cancer
1st Symptoms: Swollen lymph nodes in neck
Treatment: Clinical trial; Chemotherapy, BMT
Kayla T., Hodgkin's, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
1st Symptoms: Pulled muscle in chest
Treatment: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Erica H., Hodgkin's, Stage 3B
Cancer details: Staged at 3B
1st Symptoms: Intense itchiness, fatigue, night sweats, weight loss
Treatment:ABVD chemotherapy, 6 cycles (12 infusions)
Nicole M., Hodgkin's, Stage 4
Cancer details: Staged 2 then 4 after second opinion
1st Symptoms: Extreme fatigue, persistent itching on lower half of legs
Treatment: 6 cycles (12 infusions) chemo, ABVD then AVD (dropped bleomycin)
CC W., Hodgkin's, Stage 4
Cancer details: Diagnosed at 29, misdiagnosed as mono
1st Symptoms: Achiness, extreme fatigue, reactive rash on chest and neck. Later: chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
Lia S., Nodular Sclerosis, Stage 4A
Cancer details: Most common and most treatable form of Hodgkin's lymphoma
1st Symptoms: Extreme lower back pain
Treatment: ABVD chemotherapy
Ava O., Stage 4B
1st Symptoms: Trouble digesting, weak immune system, raised glands, night sweats, chest pain, extreme fatigue
Treatment: 6 cycles of ABVD chemotherapy
Topics: Emotional grieving, mental health, letting go
Delishea A., Hodgkin's, Stage 4B
1st Symptoms: Extreme itchiness and dry cough
Treatment: 6 cycles of chemo, radiation, immunotherapy (Adcetris)
Topics: Finding community & support, self-advocacy
Emmanuel S., Relapsed Hodgkin’s
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: ABVD, ICE; autologous stem cell transplant; Targeted therapy: Brentuximab
Kelsey R., Hodgkin’s, Stage 2A
Symptoms: Bad leg itching with no rash, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation
Manda M., Relapsed Hodgkin’s, Stage 2B
Symptoms: Loss of menstrual cycles, iron deficiency, itching, night sweats, tiredness, night terrors, trouble breathing, difficulty concentrating, enlarged lymph nodes
Treatment: ABVD chemotherapy, radiation, ICE chemotherapy, bone marrow transplant
Samantha S., Relapsed Hodgkin’s
Symptoms: Fatigue, cough, enlarged lymph node
Treatment: ABVD chemotherapy (later changed to AVD), Brentuximab, Cyclophosphamide, BEAM chemotherapy, autologous bone marrow transplant
Patrick C., Hodgkin’s Lymphoma, Stage 2B
Initial Symptom: Dry cough, difficulty breathing
Treatment: Chemotherapy (ABVD)