Shannon’s Stage 1 Lynch Syndrome Colon Cancer Story
Shannon M., who has Lynch syndrome, shares her stage 1 colon cancer story. Shannon details her experience with surgery (partial colectomy), importance of mental health care, and parenting with cancer.

- Name: Shannon M.
- Diagnosis:
- Colon cancer
- Lynch syndrome
- Staging: 1
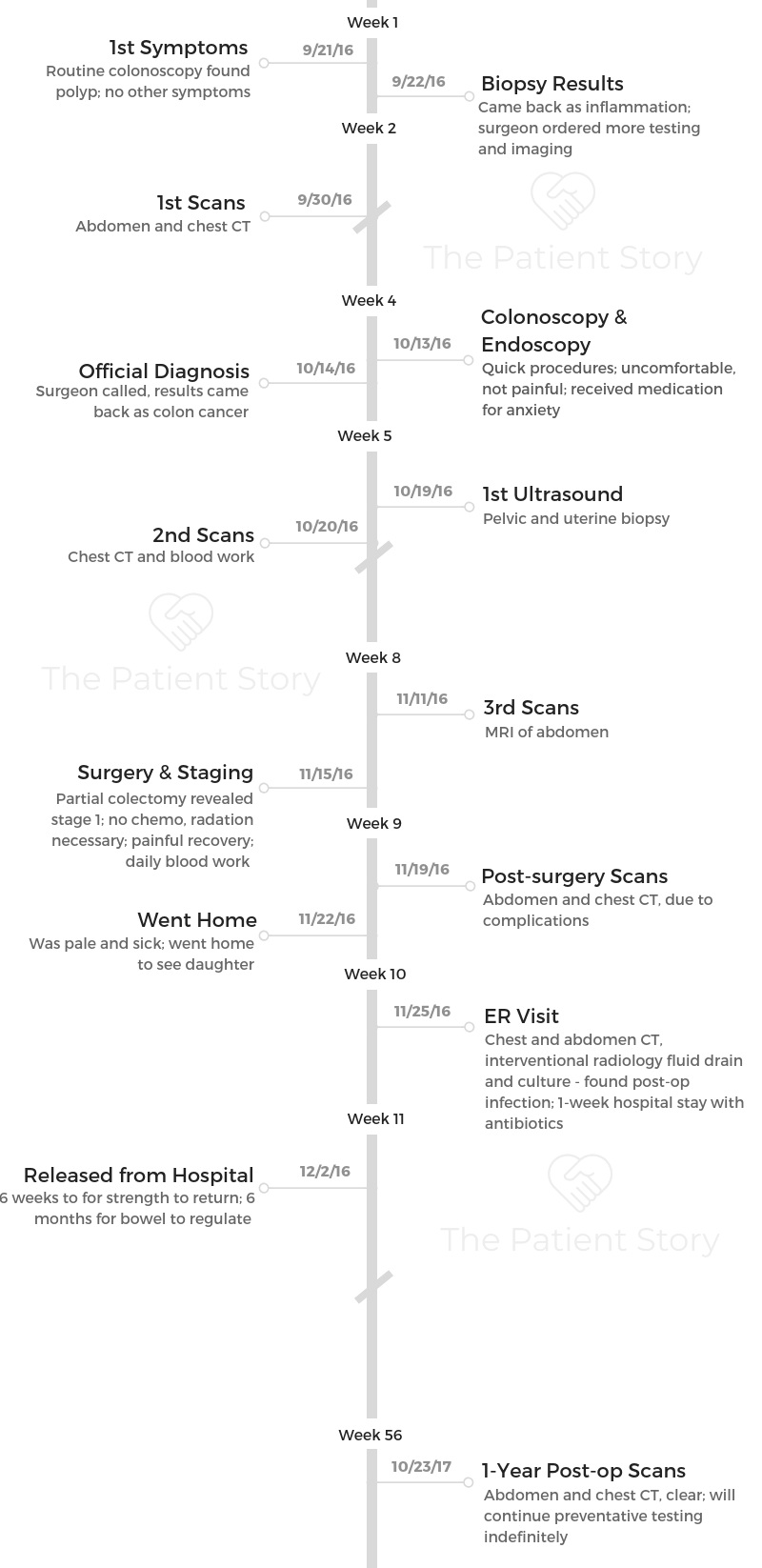
- 1st Symptoms:
- Routine colonoscopy found polyp
- No other symptoms
- Treatment: Partial colectomy
- Diagnosis
- Procedures & Testing
- How do you prepare for a colonoscopy?
- Describe the colonoscopy
- How long does it take to get results back after a colonoscopy?
- Describe the wait for results, or "scanxiety"
- Familiarity with Lynch syndrome was critical
- Describe the MRI scan after your biopsy
- Describe the endoscopy
- Did you have any other testing done?
- Treatment Decisions
- What was the biggest decision you had to make?
- That was really one of the biggest decisions with my surgeon: how much colon do we take?
- Did you ask your surgeon about his experience with similar cases?
- Do you have any advice for patients about deciding where to receive care?
- Was there anything unique about your medical team?
- Lynch Syndrome
- Surgery & Recovery
- Preparing for surgery
- What happened on the morning of your surgery?
- What’s a spinal block?
- Were you nervous before surgery?
- Can you describe what the surgery entailed?
- How did the staging happen?
- How did it feel to know you were stage 1?
- How was surgery recovery?
- Do you have any advice about surgery recovery?
- Did you have any follow-up scans?
- Long-term recovery after major surgery
- Was there anything particularly hard about being a mom with a young child after surgery?
- Support & Survivorship
- Did you have to rely on outside help with child care?
- Any advice to parents who are going through cancer treatment?
- Finding a cancer community
- How did cancer affect your relationship with your husband?
- What was the worst part of all of this for you mentally and emotionally?
- Fertility: you had to consider the possibility of a hysterectomy
- What is your advice on being a self-advocate?
- Was there any financial stress from the treatment?
- Do you have a message you would like other patients to hear?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Getting a cancer diagnosis can be overwhelming, scary, and anxious. You can feel like your world is caving in after one phone call.
What I would like you to know is that you are not alone. There are other people that are dealing with all the things that you are.
You are going to get through this. You’re resilient. You’re strong. Rely on other people. When you can’t take one day a time, take one minute at a time, because it will add up. You can get through this.
Shannon M.
Diagnosis
What were your first symptoms?
My story might be a little different in that I didn’t have any symptoms. I didn’t know anything was wrong. I had just turned 36, and my daughter had just turned 1.
I was going in for a routine colonoscopy because I have something called Lynch syndrome, which is a genetic mutation that puts me at really increased risk for a lot of different cancers. Colon cancer is one of them.
I’d just had one a year before, but it was clear. I was pretty shocked to find out the next one wasn’t quite normal. The process went from there.

How did your doctor diagnose the cancer?
I was really lucky to be dealing with a surgeon who was familiar with Lynch syndrome, because I don’t know if other surgeons would’ve caught it. They did a biopsy on a polyp that didn’t look quite right.
The first time, it came back as inflammation, and my surgeon said, “Shannon, it can’t be. It’s not right.”
He said, “I think we should do some more imaging and another colonoscopy so I can get a better biopsy and go from there.”
It was in an early enough stage that nothing showed up on my imaging. I went through the second colonoscopy a couple of weeks later. They did another biopsy, and that biopsy came back clearly as cancerous.
Getting the diagnosis
I don’t think I’ll ever forget it. It was a Friday. My husband, 1-year-old daughter, and I were visiting my parents for the weekend. My husband is a big white water kayaker, so he had just taken off from my parents’ for the next night of racing.
They don’t have cell phone reception at their house, so I wasn’t aware, but my surgeon had been trying to reach me all day. I didn’t receive the call until about 8:00 that night.
For whatever reason, my cell phone finally showed I had a voicemail, and it was from my surgeon. I knew in his voice, even though he didn’t say that the results had come back. He left his cell phone number for me. I called him from my parent’s landline at about 8:30, and he got the message and called me back about 9:00.
We had this brief conversation where he told me the biopsy had come back as colon cancer, and I’ll never forget. He said to me, “Shannon, I will always be honest with you throughout this whole process, and what I do know is that we can fix this. We have steps to take to get there, but we will fix this.”
I cried and told him that I trusted him and was happy that he was my surgeon. We left it at that. We agreed to talk about next steps on Monday.
»MORE: Patients share how they processed a cancer diagnosis
How did you break the news to your loved ones?
My dad had already gone to sleep. My daughter, Hazel, was asleep. My mom was in the kitchen, listening to my end of the phone call, when it came through. She knew.
Looking back, I was still in shock, but I never realized what that must have felt like for her. It’s probably harder than most of us realize to find out your 36-year-old daughter has just been diagnosed with cancer.
I called my husband, who was about 4 hours away, right after my surgeon and I hung up. He got back into his car and rushed to my parents’ [house]. I can laugh at this story now, but he got pulled over by a police officer on his way home for speeding.
He looked the officer in the eye and said, “My wife was just diagnosed with cancer.” The police officer said, “I’m so sorry. Drive safe, and have a good night. I wish you the best.”
We went back to Vermont the next day to process everything.
»MORE: Breaking the news of a diagnosis to loved ones
Did you keep your diagnosis private?
That has been a huge piece of my recovery. I was diagnosed. I don’t know if it was just shock. I don’t know if it was partially denial. Maybe it was me trying to minimize the situation, but we told our immediate family and a few really close friends, but it wasn’t something that I broadcast. I wasn’t ashamed.

It just felt so surreal because I was so healthy. How do you go from, “Hey, what did you do this weekend?” to “Hey, I was diagnosed with cancer”?
I wish I had broadcast it more. What I know now is that people want to support you, people want to help you, and you need it. You need that support.
I think one of the silver linings in this whole thing is connecting with others. It’s this raw level. I’ve been really lucky to be able to do that in the last 2 years since my colon cancer, but it’s not something that I did during the process.
How did you emotionally process the diagnosis?
It’s all a little blurry. That is how you deal with it in some ways. I don’t really remember our drive home. I don’t even remember what we did for the next couple of days. I must have been in shock, because I don’t remember what it was like.
I know we went in and met with my surgeon that next week to discuss the next steps. There were always next steps. There was always more testing. There was never really a stagnant period when we weren’t doing anything. Maybe that helped.
»MORE: Read different experiences of a cancer diagnosis and treatment
Procedures & Testing
How do you prepare for a colonoscopy?
The worst part is the preparation for it. Once you get through that, it’s pretty easy.
The day before, as you’re prepping for a colonoscopy, you are fasting and just on clear liquids. I do a lot of chicken broth, popsicles, clear sodas, and hydrate all day.
That evening, you start your preparation and drink a lot of different solutions that clear out your system. Up until about 11 p.m., you’re having a lot of bowel movements and some cramping. Your body is clearing out your colon so that the next day, when you go in, you’re ready for your scope.
I usually try to schedule my colonoscopies as early as I can in the morning because that way, you’re not having to fast the entire next day, too.
Describe the colonoscopy
When you get to the hospital, they put an IV in and hang some solutions. Once you get into the procedure room, you can decide if you want medication that makes you sleepy and unaware of what’s going on. Once you’re in there, the procedure of the scope usually only takes about 45 minutes.
You lay down on your left side, and everything they do is very gentle. There is only minor discomfort, like a gas cramp. Usually you can put a little bit of pressure on your stomach to help relieve that.
Usually with the medications, you are kind of aware of what’s going on but really don’t have any discomfort. If you do, it’s a small cramp, kind of like a gas cramp.
The use of the scope just takes a turn through your intestines. They back out and take another look as the scope is exiting your colon to make sure they didn’t miss anything.
After that, you’re brought out to the recovery room, and about an hour or so later, you’re putting on your clothes and heading home.
How long does it take to get results back after a colonoscopy?
About a week for the biopsy to come back. If they don’t decide to biopsy any polyps, then you know the same day if things look clear.
It’s either immediate, or they decide to take a biopsy of the polyp they removed. In that case, it’s generally 1 or 2 weeks for those results.
Describe the wait for results, or “scanxiety“
It’s always difficult when you suspect something might be wrong. When I was brought back to meet with my surgeon in his office after the first biopsy was done, he said, “We’ve got another curve ball. It came back as inflammation.”
That was hard to think about later because it had given me a little bit of hope that everything was okay when it really wasn’t.
»MORE: Dealing with scanxiety and waiting for results
Familiarity with Lynch syndrome was critical
I was lucky to be working with a team that was familiar with the risks of Lynch syndrome and understood that I have up to an 80% chance of developing colon cancer.
It wasn’t taken lightly. I didn’t have to push for anything when that came back as inflammation. He already knew it was cancer. He said, “Shannon, you can either take out part of your colon now and schedule that procedure, or we can do more imaging and another biopsy.”
I was lucky not to have to advocate for myself.

Describe the MRI scan after your biopsy
That was more anxiety-ridden than the colonoscopy. You’re put on a table and very slowly moved into a circular magnetic machine.
Lots of imaging takes place, and that procedure lasts about 30 minutes. I felt like I was in a tomb. It ended up being okay. The nurses checked on me in between the images to make sure that I was okay.
I had that test done and then came back shortly for the second colonoscopy. The results for that took about a week.
Describe the endoscopy
The endoscopy is an upper scope. It was done the same day as my second colonoscopy, so I didn’t have to fast twice.
They go down with a tube in your throat all the way to your small intestine and stomach. That took about 20 minutes, and I was heavily sedated for that. I didn’t have anesthetic spray; it was all IV push medications.
I know I had some Lorazepam for anxiety. They were ruling out any other cancers in my small intestines or stomach. It took about 2 weeks for those results.
Did you have any other testing done?
I also had a chest X-ray done — that was the last test before surgery — after the endoscopy. It was to check my upper chest to make sure there was no spread to my lungs.
Treatment Decisions
What was the biggest decision you had to make?
I have had a good relationship with my surgeon because he had been doing my colonoscopies for years prior to the diagnosis. There was some comfort in that. This wasn’t our first episode together.
Some of the decisions that I had to make were more around my Lynch syndrome. The gold standard if you have colon cancer as a Lynch syndrome patient is to take out the entire colon because that obviously cuts down your risk of having colon cancer again.
That was really one of the biggest decisions with my surgeon: how much colon do we take?
We weighed the pros and cons. That was a decision we made together with my husband. My surgeon always offered for me to have a second opinion, but it wasn’t something that I felt like I needed to do.
As a nurse, I always recommend people get a second opinion. In my case, though, I went with my gut and my heart, and I felt like he was the right surgeon for me.
Did you ask your surgeon about his experience with similar cases?
We certainly did. We talked about his experience with other Lynch syndrome patients, how many surgeries he’d done like this, the different types of surgeries he’d done to remove colon cancer, how many years he’d been in practice, and the fact that he works at a teaching hospital — all of those things.
Do you have any advice for patients about deciding where to receive care?
Smaller, rural hospitals have an absolutely amazing place in the health care system and are needed, but when you’re dealing with something that’s complicated, going to a bigger hospital or getting that second opinion would be worth it.

The main consideration, though, is whether or not you feel comfortable. You should feel good about your medical provider.
If there’s an inkling doubt inside of you that something that doesn’t feel right, you’re not being listened to, or your opinions don’t seem to matter, go seek other treatment teams.
You know your body, and you know how to listen to it. It’s important to be heard.
Was there anything unique about your medical team?
I have a naturopath who is certified in oncology and acts as an amazing addition to the traditional treatment team. She helped in treating side effects, prepping for surgery, and helped take care of you after.
She’s someone I still work with in combination with all the other normal screening and treatments.
Lynch Syndrome
When did you find out you had Lynch syndrome?
Most of the males on my dad’s side of the family have died at a really early age. My grandfather died of colon cancer and when my dad was in his mid 40s. He followed the same trend and was diagnosed with colon cancer.
This was long before genetic testing had become such a big deal. He had colon cancer, and luckily it was diagnosed early. He had part of his colon removed, but then about 10 years later, he had colon cancer again, totally unrelated to the first diagnosis.
Still, no one had suggested genetic testing. He went on to later have prostate cancer and finally stage 4 kidney cancer, but he’s still alive. He’s amazing!
It wasn’t until the fourth battle with cancer that my good friend from high school was finishing a degree in genetic counseling. He said, “Shannon, your family has to get testing. This isn’t normal.”
There was a piece of me that just didn’t want to know.
Eventually, I talked to my dad, and he very willingly went in and had genetic testing done. It was just blood work, but they ran all sorts of tests on his DNA.
It came back that he in fact had Lynch syndrome. If you have it, you have a 50% chance of passing it on to your offspring. I got tested and found out I had it, too.
That was about 10 years ago. As of right now, it’s pretty rare to know you have Lynch syndrome, even though the estimates suggest 1 in 279 have it. It’s not rare, but it’s very under-diagnosed.
I feel really fortunate. I didn’t at the time I was diagnosed, but that knowledge I received was absolute power and to this day probably saved my life.
Had I not known I had Lynch syndrome, I wouldn’t have received that colonoscopy until I had symptoms. At that point, it probably would have been a pretty late stage diagnosis of colon cancer.
Does Lynch syndrome put you at a higher risk for cancers other than colon cancer?
I’m also at high risk for uterine and ovarian cancers. I do routine testing for those as well. My colorectal surgeon strongly encouraged me to go have my testing for those done, even though it was early. They wanted to know if there were any other concerns before they opened me up.
I met with my gynecologist, and I had thickening around my uterine lining show up on the ultrasound. That resulted in a biopsy of my uterus.
Those results took another week, and that was really hard. I already knew I had colon cancer, so going from a healthy, fulfilling life to the reality that I might be dealing with 2 cancers was scary.
There are a couple of different types of Lynch syndromes. Mine has the biggest risks of colon cancer, uterine cancer, ovarian cancer, small intestine, and a slight chance for brain tumors and urinary tract cancers.
How did you adapt after you were diagnosed?
The recommendation is a colonoscopy every year and an endoscopy every 1 to 3 years. I do a uterine ultrasound every 6 months and a uterine biopsy about every year.
That ultrasound also looks at my ovaries. I also do a urine cytology once a year just to make sure there’s no abnormal cells growing in my urine.

Surgery & Recovery
Preparing for surgery
Most of the testing procedures were done during my diagnosis stage. Other than having some of the female organs checked out after I was diagnosed with colon cancer, pretty much everything had been done at that point.
I was scheduled for surgery almost exactly a month after my diagnosis. Unfortunately, I had a stomach bug right before I was supposed to have surgery. It was postponed for a week, and then I went in.
My pre-surgery looked almost identical to my colonoscopy preparation. I did the normal colonoscopy prep, but in addition to that, I took a bunch of medications prophylactically.
They had me on a couple of different antibiotics before surgery. There was a vitamin mixture. I was on a nerve medication to try and prepare for surgery and nerve pain.
What happened on the morning of your surgery?
I got there really early in the morning. First, a couple of IVs were placed. Some fluids were hung. They did a spinal block on me prior to surgery in hopes that it would put me ahead of the pain game after surgery.
My surgeon poked his head in a few times to check on me. There were some urine tests and another antibiotic hung in my IV. I was anxious, but I was there with my husband.
Eventually, after what felt like forever even though it was only a few hours, I went into surgery. I very clearly remember being wheeled back into the OR and suddenly feeling really emotional about things.

What’s a spinal block?
I have never had an epidural, but from my understanding, it’s pretty similar. They put a needle in my back and put in a pain medication. That procedure probably took them about 20 to 25 minutes to do.
They used a little bit of numbing agent before they went in with the needle. It was a little painful and uncomfortable but not unbearable by any means. It felt like there was a lot of bleeding before surgery.
Were you nervous before surgery?
When you go into surgery, it’s bright and cold, and it all hits you. There were a lot of people in the OR, and the anesthesiologist was telling me the plan and realized I was anxious.
I got a little bit of Lorazepam to make me feel more at ease. I could see my surgeon come in across the room, and I looked over at him and said, “You’ve got this. I know you’ve got this.”
He came over, and he took my hand and said, “We’ve got this. We’ve got you.” At that point, I got anxious. I shed a tear or two, and that’s all I remember until after surgery.
I tried to do a lot of preparation because I knew that that moment was going to be difficult, and I wanted to do everything in my power to go into that OR feeling confident and relaxed.
I remember I did some visualizations of going into the OR and having all of these people who had my best interests in their hands helping me. I knew there would be a guiding light and that it was all going to be okay.
Can you describe what the surgery entailed?
My surgeon felt confident enough to give me the option of doing open surgery, where they would use a big incision to cut open my intestinal area, or go in laparoscopically.
Going in laparoscopically was supposed to be a better option for me because it would make further surgeries easier. That’s what we decided on. They went in and used 5 little incision marks in my abdominal area.
They filled me up with air so they could get their instruments in to do everything they needed to. I had about 3/4s of my colon removed, and they used a little incision around my belly button to remove that.
Then they stitched me back up in the 5 different spots. There was a little cut on my liver they had to suture, but luckily that was not a big deal, and that was the end.
How did the staging happen?
They were not able to stage it until after they had taken a bunch of lymph nodes during surgery.
They biopsied those while I was recovering in the hospital, and I found out it had not spread to my lymph nodes. They diagnosed me as stage 1 colon cancer. That biopsy only took about 48 hours.
How did it feel to know you were stage 1?
Even though I was blurry on pain medication at the time and feeling bad after surgery, I felt like a weight had been lifted off my shoulders.
That news meant that I likely would not need chemotherapy or radiation. That felt like a huge gift had been given to me. My surgeon said, “This is really good news, Shannon. This is really good news.”
How was surgery recovery?
The spinal block didn’t really work, so I woke up frantically as they were wheeling me out of surgery in what felt like pretty uncontrollable pain. It was really uncomfortable in my stomach, and the gas that they had filled my belly up with had this radiating pain all over my shoulders and neck.
I was incredibly uncomfortable. I was receiving quite a bit of pain medication that made me really nauseous. We did eventually get my pain better controlled, and I was wheeled up to the surgery floor, which is where the nurses took over through my recovery.

Do you have any advice about surgery recovery?
I went in with certain expectations. I expected that even though I might be weak and recovering, I’d be home with my daughter.
Try not to have expectations. Try and go into this knowing there might be a few curve balls. Put all of your positive vibes and energy into the fact that it’s going to go well, but be ready to accept that things might change.
Things might be a little bit different than you were told, and unfortunately, we have no choice but to accept that.
Did you have any follow-up scans?
I had a lot of scans while I was in the hospital after surgery because they were concerned that something was going on.
I had 2 MRIs while I was still in the hospital. I saw my surgeon a lot in the hospital. I saw him the week after I had finally been discharged. Then I was seeing him about every 2 weeks to run blood work and have him check my abdomen.
Once I didn’t have symptoms from the post-surgery fluid, I was meeting with him once every 3 months.
At the 1-year mark, I had more imaging done. I was having blood work done to look at my colon markers every 3 months.
That all stayed the same until the 2-year mark, then it switched to blood work every 6 months. At year 3, I’ll be going back to a colonoscopy each year and blood work.

Long-term recovery after major surgery
It took me about 6 weeks to feel like I had as much strength as I wanted to for short hikes, to lift up my 1-year-old daughter, and to return to work part-time.
It took closer to 6 months to really start feeling like myself again. I was having abdominal pain [and] nerve pain from surgery for a while.
I’d like to say my bowels have regulated, but I think they’ll always be a little bit off when you’re dealing with less colon than most people.
I went from someone who had a normal bowel movement once every day. After surgery, I was having 5 to 10 loose stools per day
Around 6 months, that started to even out a little more to 2 or 3 times a day. I had full control thankfully, but certainly with a little more urgency when I do have to go.
My naturopath has really helped me with recovery. She’s really made a big difference. She helped me to get on some probiotics, natural anti-inflammatory medications, and fish oil, a couple different things that have seemed to really make a difference for my system. Now, unless I eat foods that are upsetting to me, I’m having 1 or 2 bowel movements a day.
Was there anything particularly hard about being a mom with a young child after surgery?
I came out of surgery needing nurses to find me a breast pump from the maternity floor, so I could try to pump breast milk because I was engorged. It was one of the biggest challenges that I faced.
It was extremely challenging to have all these fears with a recent cancer diagnosis when you just gave birth a year ago to a little human who has become your world.
The physical aspect of still breastfeeding and having to figure out how to pump at the hospital was so hard. Figuring out who’s going to be helping take care of your child when you have 2 weeks of unexpected hospital stays is really challenging.
Support & Survivorship
Did you have to rely on outside help with child care?
My husband and I are really lucky to both have wonderful families. Even though they’re not local, they’re both within about 3 hours. There was a lot of coordinated care when I was in the hospital.
My husband was spending really long days with me there, running home to relieve one of our parents, and trying to create some normalcy for our child. Thank goodness our parents were willing to help, and my husband, Matt, was just a hero when it came to juggling everything.
Any advice to parents who are going through cancer treatment?
Ask for every piece of advice and resources that the hospital can give you.
It’s so overwhelming to receive a cancer diagnosis; it feels like your world just stops. It’s easy to overlook the fact that there might be resources to help with childcare, support, and counseling that we might not be aware of. Be open to connecting with other people.
»MORE: Parents describe how they handled cancer with their kids
Finding a cancer community
One of the biggest pieces of this cancer journey has been allowing myself to connect with other young people who have had cancer. For me, that meant attending some different cancer workshops, weekends of hope, and informative conferences about Lynch syndrome.
I went to women’s health and cancer conferences. I got involved in a young survivor group in a nearby city, and that has been such a huge piece of my healing. I don’t think you ever want to normalize cancer, but when you’re diagnosed, I know I felt like I was alone.
There’s so many other people who have been through something so similar to what I have been through, and connecting with them has made me feel like it’s going to be okay.
Other people have gotten through this, and I will continue to get better. On the days I feel like I can’t get through it, there’s others there that I can lean on to support me. When I am feeling really strong, then I can support them.
That is part of this beautiful picture. We are all in this together.
In the last year, I started an Instagram page with the sole purpose of trying to connect with other young cancer survivors, especially people my age with Lynch syndrome. Instagram and social media have been a really amazing platform for me.
Ironically, it’s made me feel like I’m able to live a more authentic, honest life. It’s given me an outlet and a way to hopefully help support some other people.
How did cancer affect your relationship with your husband?
It brought out some of the best in us, and it brought out some of the worst in us as well. When you go through a cancer diagnosis, all of a sudden, you have these emotional needs that you didn’t know existed.
Your partner doesn’t necessarily know what they look like. In a moment, life has changed, and your partner is dealing with this new fear and diagnosis just as much as you are.
For us, there were a lot of stressful times. The first year of cancer allowed my husband and I to realize where our weaknesses in our relationship were.
We realized how much communication we both needed. The positive is that it really allowed us to grow and to continue to do so, because Lynch syndrome is a lifelong thing for me.
Once I finally reached the healing process of cancer, we were able to take an honest look and say, “Okay, we want to be there for each other more, and these are the ways that we need to grow to do so.”
We’re all different, but what helps me is to remind myself every once in a while that we both have the best of intentions. Our goals are the same.
We want to be there for and comfort and support each other. Some days it comes out just perfectly, and other days, for whatever reason, it doesn’t. At the end of the day, we both love each other, and we both support each other.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer

What was the worst part of all of this for you mentally and emotionally?
The worst part for me was having Lynch syndrome. I always knew that there was probably a good chance that at some point in my life, I would have cancer. I did not expect to have cancer at 36.
The hardest thing was thinking, “Wow, I’m getting this first cancer diagnosis at 36. What does that mean for the rest of my life?” That took me a while to process.
It’s an ongoing process, and it probably will be the rest of my life. What I try to remind myself every day is that I’m living a full life, and I love my life.
I have to trust that even if I do get another cancer diagnosis, it’s going to be okay. We’re going to work through that as well.
There’s a huge silver lining when you have been diagnosed with cancer or are living with Lynch syndrome. You don’t take a day for granted. It puts a whole new spin and perspective on your life.
Suddenly, some of the things that used to be a big deal aren’t anymore. What you really want and things that really matter have this way of becoming so clear.
Fertility: you had to consider the possibility of a hysterectomy
I’ve had a lot of conversations with my husband about timing. It’s going to happen at some point; it’s important to talk about. We feel really happy to have this one seemingly healthy, wonderful child, so we’re done having children.
The second piece of the puzzle is weighing the benefit-to-risk ratio of being so young and having a full hysterectomy. We have to consider what going through menopause looks like long-term for my health.
We revisit those conversations when I need to talk about them during my appointments. For now, as long as everything looks okay, I have decided with her recommendations to wait closer until I’m 40.



What is your advice on being a self-advocate?
Self-advocacy is so important. As a nurse and someone who’s connected with a lot of young people who have had cancer, I see young people having symptoms that aren’t normal, but they’re being ignored by doctors.
Listening to your body is so important. You know it best.
When you know that something’s not right, it’s been more than 2 weeks, and you’re having the same symptoms, advocate for yourself until you feel like the right tests have been run.
»MORE: How to be a self-advocate as a patient
Was there any financial stress from the treatment?
I was really lucky because we have a really good insurance that covered almost all of our costs. The challenge came when I wasn’t working and wasn’t covered. That put some financial stresses on us. We focused on what needed to happen for me, and we went through it and worried about the rest later.
I wish I had met with a social worker, who could have better explained all the financial stuff to me, since I didn’t have the time to look into that myself.

Do you have a message you would like other patients to hear?
Getting a cancer diagnosis can be overwhelming, scary, and anxious. You can feel like your world is caving in after one phone call.
What I would like you to know is that you are not alone. There are other people that are dealing with all the things that you are.
You are going to get through this. You’re resilient. You’re strong. Rely on other people. When you can’t take one day a time, take one minute at a time, because it will add up. You can get through this.

Inspired by Shannon's story?
Share your story, too!
Colon Cancer Stories
Shannon M., Colon Cancer, Stage 1
Cancer Details: Found the cancer as a result of her Lynch Syndrome
1st Symptoms: Routine colonoscopy found polyp
Treatment: Partial colectomy
Hugo T., Colon Cancer, Stage 1
Cancer Details: Diagnosed 2 weeks after 5 years remission from testicular cancer
1st Symptoms: Inflamed bowel
Treatment: Subtotal colectomy, immunotherapy
Rachel B., Sigmoid Colon Cancer, Stage 1
Cancer Details: The sigmoid colon (or pelvic colon) is the part of the large intestine that is closest to the rectum
1st Symptoms: Stomach discomfort, nausea, bloating, blood in stool
Treatment: Colectomy
Chris T., Colon Cancer, Stage 2
Cancer Details: Discovered Lynch Syndrome after genetic testing
1st Symptoms: Found the cancer as a result of family history, early colonoscopy
Treatment: Partial colectomy
Shannon C., Colon Cancer, Stage 2A
Cancer Details: Diagnosed at 29, tested positive for Lynch Syndrome
1st Symptoms: Severe pains after eating
Treatment: Partial colectomy
Barbara M., Colon Cancer, Stage 3
Cancer Details: Family history wasn’t flagged, should have had colonoscopy earlier
1st Symptoms: Stomach discomfort, difficult to process food
Treatment: Colectomy, Chemo (FOLFOX, CAPOX)
Shelley B., Colon Cancer, Stage 3B
Cancer Details: Had no usual first symptoms, found as a result of routine colonoscopy and endoscopy
1st Symptoms: None
Treatment:Partial colectomy, chemotherapy (FOLFOX)
Lindsay D., Colon Cancer, Stage 4
Cancer Details: Diagnosed at 32, cancer spread to ovary and lung
1st Symptoms: Lump in pelvic area, funny-smelling food, weight loss
Treatment: Chemotherapy, colectomy (surgery)
Lee J., Colon Cancer, Stage 4, Recurrence
Cancer Details: Recurrence then remission
1st Symptoms: Discovered stage 4 cancer from unrelated CT scan
Treatment: Neoadjuvant chemo (FOLFOX), hemicolectomy (partial colon surgery), adjuvant chemo (FOLFOX), chemo post-recurrence (FOLFIRI), liver surgery
JJ S., Colorectal Cancer, Stage 4
Age at Diagnosis: 27l
1st Symptoms: Abdominal pain, blood in stool
Treatment: Surgery to remove tumor, chemotherapy, clinical trial of Keytruda (pembrolizumab)
Haley P., Colon Cancer, Stage 3C
Symptoms: Constipation, fatigue, shortness of breath
Treatment: Surgery, chemotherapy
Amanda G., Colon Cancer, Stage 2A
Symptoms: Gurgly stomach, blood in stool, chronic constipation
Treatment: Surgery (hemicolectomy), chemotherapy (CAPOX), Zarxio
Symptoms: Fatigue, anemia, irregular bowel movements, loss of appetite, heavy periods Treatment: Laparoscopy, chemotherapy, partial hysterectomy
Dania M., Colon Cancer, Stage 4, with Liver and Peritoneal Carcinomatosis
Symptoms: Constipation, diarrhea, terrible bloating, swollen belly, as if pregnant
Treatment: Surgery, immunotherapy (KEYTRUDA)
Stephanie K., Colon Cancer, Stage 3
Symptoms: Very bad cramps, bloating, indigestion, burping
Treatment: Surgery, chemotherapy (CAPOX)
Jason A., Colon Cancer, Stage 3B
Symptoms: Abdominal pressure, fatigue, small amounts of blood in stool
Treatment: Surgery (colon resection), chemotherapy (FOLFOX: folinic acid, fluorouracil, and oxaliplatin)