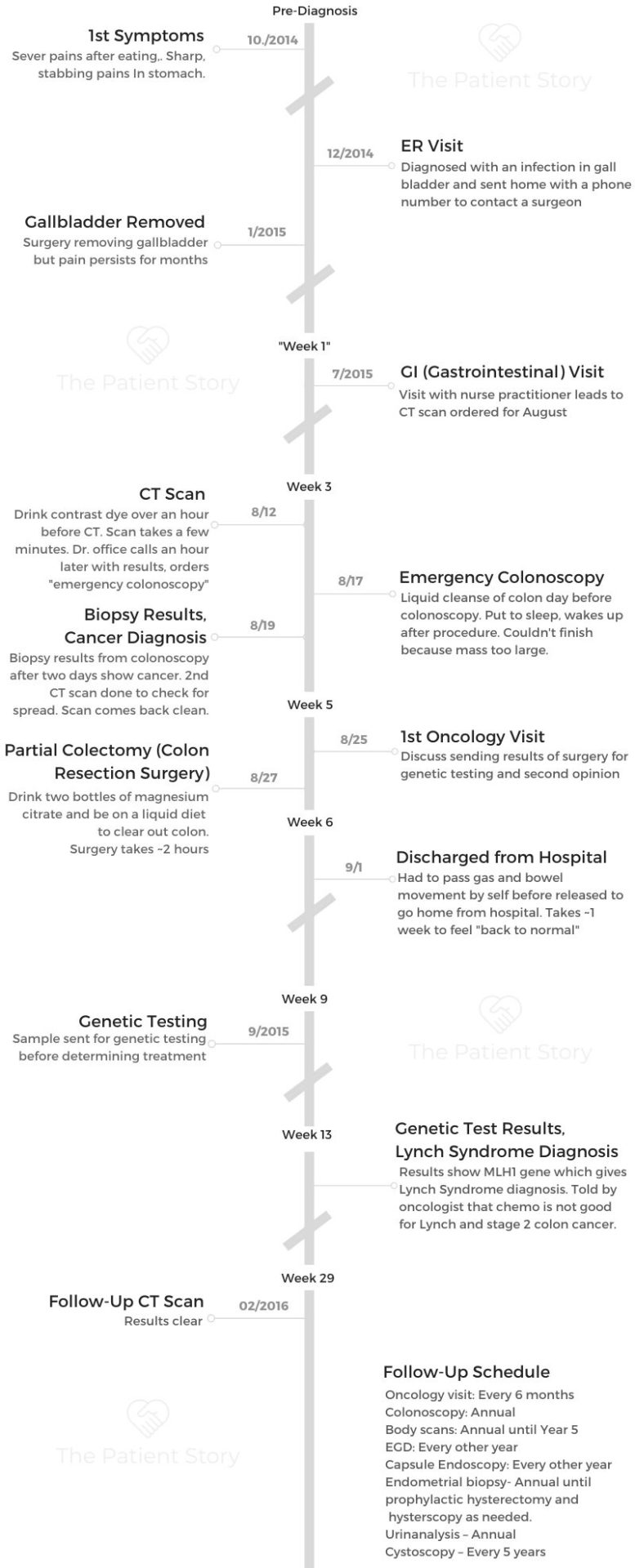
Shannon’s Stage 2A Lynch Syndrome Colon Cancer Story

- Name: Shannon C.
- Diagnosis:
- Colon cancer (1st misdiagnosed as gallbladder issue)
- Lynch syndrome
- Age at diagnosis: 29
- Staging: 2A
- 1st Symptoms:
- Severe pain after eating
- Sharp, stabbing pains in abdomen/stomach area
- Treatment: Partial colectomy (colon resection surgery)
- First Symptoms and Tests
- Colonoscopy
- Colon Cancer Diagnosis
- Describe the meeting with the surgeon
- How did you process the cancer diagnosis?
- Describe the process of setting up the surgery (colectomy)
- How did you tell family and friends about a cancer diagnosis?
- Advice to others on how to conserve energy
- Was there any cancer staging?
- Advice on dealing with scanxiety
- Genetic Testing and Surgery (Partial Colectomy)
- How did you decide to get genetic testing done?
- What are the treatment options?
- What is prep for the partial colectomy like?
- What is an ostomy bag?
- If you needed the ostomy bag, how long would you have worn it?
- What happened at your partial colectomy (colon resection surgery)?
- What do you have to do get discharged from the hospital?
- Recovery and Follow-Up
- Lynch Syndrome Diagnosis
- Mental and Emotional Impacts of Cancer
- What’s the best thing that gets you through the hardest times?
- Best advice you’ve ever gotten
- How did you tell your kids about the cancer diagnosis?
- How does cancer impact your marriage and your husband?
- What do you wish you had known before cancer?
- Perspective on life after cancer
- Where do you find cancer support?
- Survivorship
- Message to people dealing with a new cancer diagnosis
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
You aren’t alone. There’s a world full of wonderful people out there to help you through emotionally, physically.
It may feel like your world’s crashing down, but there’s so much support out there for you. Take it one second at a time until you can make it one minute at a time.
Shannon C.
First Symptoms and Tests
What were your first symptoms?
I was having severe pain after I would eat out. 20 minutes after, it is just excruciating, and I have a very high tolerance for pain. I thought maybe it was something with my diet. Something wasn’t sitting right.
I obviously paid attention to it, tried switching around, and it never really happened or never really fixed it. I went to a doctor in the fall of 2014 in November, and they said I had an ulcer because of the pain, where it was at, and I was eating. He put me on medication and [told me to avoid] caffeine, spicy foods, things like that.
That didn’t help, so I ended up living with it. Then it started getting severely worse, and I was bowled over in pain one night crying.
This is in December, and my husband urged me to go to the ER. “This isn’t like you.” I went, and they brushed it off like, “Why are you here for abdominal pain?”
They ended up doing an ultrasound and found out that I had an inflamed gallbladder, so they thought that was the issue. They gave me a surgeon’s number and told me to take Tylenol and contact the surgeon. That’s how this whole thing started.
I’m a type 1 diabetic, so I try to pay attention to patterns because of my blood sugars. I also had 2 young boys. They were 3 and 1 at the time. That wasn’t really the forefront of my issues. I was just trying to alleviate it by myself. Trying to figure out how I can make this a little better. I didn’t think it was a big issue.

It was stomach pains, and then it started getting worse really quickly. Really bad. I was starting to get very tired, but I wrote that off as having 2 young kids and working full time.
Which medical expert did you call first?
I contacted the surgeon. They ended up having my gallbladder removed because I’m a type 1 diabetic. There were a few potential issues with having an inflamed gallbladder they wanted to take care of. They didn’t think it was something more serious.
I had my gallbladder removed in January of the next year. I was still having this pain but not as bad, so I thought maybe this is part of the healing process. It was still painful into March, and I had started asking other people who had their gallbladder removed. I said, “Was it still painful? How long did it take for this pain to go away?” Everyone I asked was like, “What? You shouldn’t be having pain anymore.”
I blew it off at that point. I continued on with life, but then it started to pick up more and become even more severe after that. I made an appointment with a local GI. I think it’s relevant to say my mom also had colon cancer at 44. I went to go see her doctor that she had. [It] took me a month to get in. My appointment was set for the end of June to see the GI.
I could tolerate this pain at this point, so I ended up cancelling that appointment and moving it another month because I could tolerate it. I could still function. There were pressing matters with my 2 boys, and things were going on in life, so I blew it off for a little bit.

Describe the progression of pain
It was sharp [and] felt like someone was stabbing me in the stomach. Sharp, very sharp. It would only last for so long, and I felt that I could tolerate it for that amount of time. That’s what it was — this pain. All this constant pain and being tired.
Looking back at it, I shouldn’t have written it off. There weren’t any other symptoms that I heard from other people. I didn’t have any change in bowel movements or rectal bleeding. I wasn’t having any of that, so I was trying to figure it out on my own.
What happened at the GI (gastrointestinal) appointment?
At this appointment, we ended up having to see the NP (nurse practitioner) because I canceled the first appointment with the doctor.
I went in and was describing what was happening. She said that because I was a type 1 diabetic, this could be another autoimmune issue. Then she also said that she was going to send me for a CT scan because I had mentioned that my mom had colon cancer at 44.
I said, ‘What are you going to do a CT scan for?’
She said that she wanted to check for colon cancer.
I said, ‘I’m 29. I don’t have colon cancer.’
She shot me down and was going to schedule it anyway.
Describe the first CT scan
That was in the end of July. I had my CT scan August 12 of the following month. She sent me to a different hospital system than what was local because of some type of imaging that they had that was better than around here.
They gave me contrast to drink. [I had] an hour I have to drink it. They do a chest, abdomen, and pelvis CT. You fit in a tube, and it takes about a minute or minute and a half to go through the tube and come back out.
It was 45 minutes away, and before I could even get home, my GI’s office was calling me, saying they needed to schedule an emergency colonoscopy.
I asked why. They couldn’t tell me what it was at that point. This is on a Wednesday. The following Monday, my colonoscopy was scheduled.
What’s going on in your mind at the time?
I’m not a person who gets worked up about a lot of things, so I figured, “Well, at least they’re coming to some sort of conclusion, because I’ve been living with this for a while now.”
Cancer was still not registering in my head whatsoever.
I was thinking maybe the colonoscopy showed an autoimmune issue because the CT tech who scanned me before I left had asked me if there was any irritable bowel syndrome (IBS) that ran in my family. That’s where I was thinking. It wasn’t anything further than that.
Colonoscopy
What happens at the colonoscopy?
They actually have a local surgical center that I went to. Before the colonoscopy, I had the prep, which wasn’t really that bad. I was expecting a lot worse, and it wasn’t. I was actually able to get sleep, because I have 2 boys!
Afterwards, they pulled me out of the operating room and obviously woke me up. They didn’t really say much until I had come to. My husband was right next to me. The doctor comes around, and she says, “We found a mass. We couldn’t finish the colonoscopy.” She said she wasn’t sure what it was.
How long does it take to get the colonoscopy results?
She sent the biopsy of the mass and said it should be returned in 2 days to let us know exactly what it was.
At this point, I think she knew what it was because my husband later Googled the image that we got in the report to get an idea. She was young, she was our age, and I think it hit home to her, so she didn’t want to say what it was — that it was probably cancer. My husband and I went home, and we waited.
That was a very long Tuesday because the results ended up coming in Wednesday. I tried to keep myself busy [and] tried to keep it together for my boys, knowing potentially what was in my future.
Wednesday comes around. My doctor’s office calls me in the morning. My husband had [gone] to work at that point because we weren’t sure how we were going to get the news of what it was. Then they say to me, “We need you to get someone you can trust to come with you to the surgical center as soon as possible.” That’s all they said.
I was a little crazy at this point. I had my 2 boys at home, so trying to keep it together until I could at least leave them somewhere. I had to call my husband to get him to come home so we could go to this meeting.
My mother-in-law came over and watched our boys. My husband came home from work. He and I drove up to the surgical center in silence.
We didn’t know what laid ahead of us.
Colon Cancer Diagnosis
Describe the meeting with the surgeon
We got to the surgical center. They ushered us into a very small conference room. We sat down. The doctor’s not in yet, and we had no words. We didn’t know what to say at this point.
My doctor came in. She looked at us and said, ‘I have never had to tell anyone as young as you are about cancer. Typically, my patients are 70 and older that I have to tell this to, but you have colon cancer.’
I remember a tear coming down on the side of my cheek, and I looked over to my husband. He was crying. At that point, I’m like, “Okay, got to get it together. What do we do next?”
That was how we found out.

How did you process the cancer diagnosis?
I didn’t know anyone who’d even remotely come close to colon cancer. My mom was 44, and I wasn’t even supposed to have a colonoscopy until 34.
It was just, ‘Okay, this is the news.’ I let myself have a moment, and then I’m like, ‘Okay, what are the plans?’
We live around Detroit, Michigan. My husband says, “Well, I have this surprise planned for us to go to Houston, Texas, tomorrow.”
My medical team was wonderful. They had gotten me to have a CT scan that day just to see if they could see if anything had spread or not. That came back clear at that point.
Describe the process of setting up the surgery (colectomy)
They figured that I was just going to go straight to surgery as far as treatment goes. They set me up to see a surgeon that day. We left the surgical institute to my new surgeon’s office. We saw her. She looked at my chart, she looked at everything, and she said, “I think we can do this with just surgery alone.” So we saw her.
I had a few other [tests] done. Then around 7 at night, we got the okay that we could leave for Houston the next day.
We left for Houston. I love baseball. Houston Astros are my favorite team. Our fifth wedding anniversary was that Friday, and we were at the Astros game in Houston. They had a no-hitter that Friday, so it was a wonderful vacation. My family lived in Houston, so I got to spend time with all my relatives.
We came back, and an hour after my plane landed, I had my doctor calling saying, “You need to go here, you need to do this, you need to go to the hospital, and you need to have this done.” They had a surgery set up for me that Thursday.

How did you tell family and friends about a cancer diagnosis?
My husband had that trip planned, and we went from the surgical institute to my surgeon’s office. I realized I was going to have to see my grandfather, aunts, uncles down in Texas. I didn’t want to just show up and be like, “Hey, guess what? I have cancer.”
I couldn’t tell them at this point. I didn’t have the heart to tell them that this was actually happening. We were in my surgeon’s office waiting for my surgeon, and we had an inclination she would [wait] a little bit before she saw us.
In this exam room, I told my husband, ‘I need you to call my family, and I need you to tell them because I can’t right now.’
I was strong and motivated to get everything taken care of, but I wasn’t ready to deal with it on another emotional level. He made the phone call. He let them know. He answered their questions as best as he could. That was one of the harder things to do.
My mom and my sisters live around here, and I called my mom after my appointment and spoke to her. She let my sisters know. I was not ready to deal with it on an extended family level at that point. Thankfully, my husband took care of that for me.
»MORE: Breaking the news of a diagnosis to loved ones
Advice to others on how to conserve energy
Rely on someone else to help you if you feel you cannot do it.
Was there any cancer staging?
She couldn’t stage the cancer at that point. She said they couldn’t finish my colonoscopy because my mass was large. She just took a biopsy of it, and it came back as cancer.
I wasn’t even sure what the next steps were. I didn’t even know what doctors I had to see.
I asked her about stage, and she said she wasn’t sure yet, but I’d have to see a surgeon and have a few other tests beforehand. Looking back to it, the mass had grown outside the colon walls. That’s why they couldn’t get through my colonoscopy.
We weren’t sure about the staging. After the CT came back from later on that day, we had a good idea that it hadn’t yet spread, at least into different organs. That was a positive aspect in the whole scheme of things that day.
Advice on dealing with scanxiety
I’ve had a few scares of other cancers, and the scanxiety is very hard to deal with sometimes. I find if I refocus and recenter myself on what’s at hand — that what’s going to happen is going to happen. I can’t control it by worrying. It helps me.
It’s different for different people, but if I realize that this whole entire situation is not entirely in my hands and allow myself to feel negative about it, it’s not going to change the result.
»MORE: Dealing with scanxiety and waiting for results
Genetic Testing and Surgery (Partial Colectomy)
How did you decide to get genetic testing done?
I actually did. I had my colon resection moved. They took 29 lymph nodes from my ascending colon. One was inflamed, but they all came back fine.
They staged me as 2A. My doctor had sent my tumor out for genetic testing because you can personalize some of the treatments for how that comes back.
My oncologist had never seen anyone my age with colon cancer, nor do I think she had many Lynch syndrome patients, if any at all. My oncologist recommended me for genetic testing, which I drug my feet about at first, because for a while, I didn’t even want to know if I had a risk for something else at that point. It was hard for me to work through initially. She was waiting on my genetic testing and tumor to come back.
I was diagnosed in the middle of August. I had genetic testing in September, the following month. The genetics of my tumor didn’t come back until September. It came back that my tumor is MSI-high, which was probably Lynch (syndrome).
»MORE: Read our interview with a genetic counselor

What are the treatment options?
My oncologist was up in the air whether to do maintenance chemo or not. She wanted to do it because of my age. I was also type 1 diabetic, and she wasn’t sure how the MSI-high was going to play into chemo.
Turns out that it can be detrimental to Lynch patients for chemotherapy for stage 2.
She brought my tumor to a tumor board and sent me to another doctor, whom I got another 2nd opinion with in October.
At the colon resection, I saw the oncologist. I had blood work done. They were monitoring me at this point. My pathology came back, and they staged me. My oncologist sent me to genetic testing and sent me to second opinion.
My Lynch diagnosis came back in October, and I saw the second opinion the day before my Lynch diagnosis came back.
That second opinion doctor said he agreed with what the tumor board had told her — that I would not be a good candidate for chemo because it was detrimental for a stage 2 Lynch patient.
At that point, they decided I was most likely cancer-free and that I needed to be monitored strictly from that point on.
The next day, I got a phone call from the genetics department at the University of Michigan letting me know I had a Lynch diagnosis. That was a slap in the face.
What is prep for the partial colectomy like?
The prep was actually like the prep for colonoscopy, except I just had to drink 2 bottles of magnesium citrate and be on a liquid diet. It was pretty much the colonoscopy process to get the colon cleared.
I went in early in the morning, around 5 o’clock. I’m a type 1 diabetic, so they always see me first. I think the surgery lasted 2 hours. It wasn’t very long, as opposed to a lot of them. We weren’t sure when I went in for the surgery if I was going to wake up with an ostomy or not.
What is an ostomy bag?
It’s a bag where they have to put your colon through your skin in order to relieve yourself of your stool. They weren’t sure if they were going to be able to reconnect my colon at that time and said that I may have to have an ostomy.
As the surgery went, they were able to reconnect it without any tissues dying or anything, so I didn’t have a bag when I woke up. At that point, I didn’t even really care if I had one or not.
When you have to worry about things like surviving cancer, it didn’t bother me if I would have woken up with one, to be honest.
If you needed the ostomy bag, how long would you have worn it?
My doctor said I’d probably have it for about 3 months, and then I’d come in. They’d do another surgery where they tried to reattach my colon and would no longer have a bag.
That was the only concern my surgeon had. I didn’t care.
What happened at your partial colectomy (colon resection surgery)?
They took out my ascending colon and reattached my colon together, so I just have that part missing. I was in the hospital for 4 days. It was going to be between 4 and 5 days, but I’m the type of person who likes to do as much as I can to get out early. I was up and walking around 2 days later. That was it for the surgery for that.
»MORE: Read more patient experiences with surgery

What do you have to do get discharged from the hospital?
I had to have a bowel movement, and I had to fart before I could leave [the hospital].The gas can build up, and they need to make sure you can push it through your system.
I had to stay one additional night from when they were going to let me go home because I had bloody diarrhea. To make sure that my bowels are still functioning well, they had to make sure everything was mostly returning to normal.
Obviously, it’s not going to turn normal right after a major surgery immediately, but they had to make sure my systems were working correctly and everything was under control.
I had rectal bleeding with diarrhea, so they kept me for one more night just to make sure it wasn’t a bigger issue than it could’ve been. They never really said what it was.
I’m assuming it was just the surgery internally healing. They kept me one more night, and then it went away, so they let me go home.
Recovery and Follow-Up
Describe the recovery process
As far as recovery time, I think it was about a week. I’m one who likes to push my limits, and sometimes it’s not a good thing. My husband was very like, “You need to lay down on the couch and not do anything.” He set up for people to come over and help with the boys during the day while I recovered.
When do you feel more fully recovered?
After about a week, I was able to really get up and start doing things. I would get up for a little bit, but I was really tired after the surgery. I think that’s a really good point to make. You need to let yourself heal sometimes, even though your mind may be saying, “You’ve got to get back to normal; you’ve got to do this.”
But sometimes it’s good to just give your mind a rest and just relax.
What are the follow-up scans?
They did a body scan 6 months later just to make sure that nothing had started again. That came back with a spot on my liver. I had the body scan, and then I had a doctor appointment. My husband wasn’t going to come with me to the doctor appointment.
He was just going to stay at work, but he ended up surprising me at the doctor appointment, thank the lord. My doctor walked in, looked at me, and said, “Well, we found something on your liver.”
I didn’t think I was ready to do this again. They ended up doing another MRI and found it was a benign mass that they saw on my liver. That was my first real anxiety!
My oncologist makes sure she has an answer for everything that could potentially be an issue. She scanned me from head to toe, sent me back for an MRI, looked at the area, and it came back benign.
In terms of PET scans, she said something about how what she needed to see in my tissues wouldn’t show up on a PET scan. She always sends me for CTs.
How do you mentally manage the scans?
There’s nothing you can do to make the outcome any different. If you waste negative energy on crying and worrying about it, it might even make it worse because sometimes it’s not anything to worry about.
What is the overall follow-up plan?
They were planning on watching me closely and developing a plan according to how my genetics came back.
You have an annual colonoscopy now
I have them the rest of my life. They put me under, so I don’t feel anything. I just sleep and wake up, and they let me know if they found anything.
I also have to do EGD every year, so they do that at the same time as well. They stick a tube down your throat to see into your stomach and your esophagus because I have risk of gastric cancer. They do the colonoscopy and EGD at the same time.
They put you under, so I don’t feel anything. I just sleep and then wake up. Sometimes it’s a good break, having boys! I always joke and say it’s the best 45 minutes of sleep I get.
Lynch Syndrome Diagnosis
Describe when you learned your Lynch syndrome diagnosis
I think there are 5 different mutations attributed to Lynch. I’d just seen the second opinion the day before and was pretty happy thinking I was cancer-free.
I wasn’t going to have to hear the word “cancer” again, and the next day I got a phone call from the genetics department saying I had tested positive for the MLH1 mutation, which opened up a whole entire category of risk for cancers. I’d have to be monitored.
I was so elated one day, and the next day, it was like someone pulled the rug from my feet and smacked me in the face, because I’m never going to escape the cancer world. I had a really hard time with that one.
I was mad about it, actually, at first. We went through colon cancer. It turned out very positive for us, and then we found out that I had Lynch. Not only that, now my sons have a 50% chance of having Lynch. That was a big pill to swallow for me.
What’s the follow-up because of Lynch syndrome?
I’d have to have a yearly colonoscopy because I have a higher risk of occurrence now. On top of that, I have a higher risk of developing a second cancer within 15 years of my first diagnosis.
That raised my original risks a little bit higher now. I’m monitored all the time for them.
The colon cancers grow very fast. My GI said I probably had cancer for 1 to 2 years before they found it at stage 2. It just started, as opposed to 5 or 10 years for the general population without Lynch.
Yearly body scans until year 5. CT scans until 5 [years]. For different medical professionals, they have different opinions on how monitoring Lynch should be. [My oncologist] and I are in talks of maybe having a yearly MRI after the body scans, because I’m going on year 5 right now.
We’re figuring it out as we go when it comes to Lynch. There’s a lot of additional monitoring on top of colonoscopies and things like that.
Is there family history of colon cancer or Lynch syndrome?
She was 44. She was diagnosed in the early 2000s, and I don’t think anyone brought up any genetic issues because I think she was so close to 50 that her doctors didn’t really think anything of it. That’s what I’m assuming. My mom has passed, so I can’t really ask her.

She was stage 1. She was pretty much like me. She had surgery, and then she was okay. For some reason, it didn’t raise a red flag.
My great-grandfather on her side passed away from colon cancer when he was 35, so we don’t have any records of that side of the family.
My great-grandmother also had Lynch, but she had skin cancer. She never had colon cancer. My mom was the only one with colon cancer. We didn’t have a really heavy family history of cancer that we knew of.
How do you tell family after a positive Lynch syndrome result?
They gave me a letter that the genetic counselor had already written up for anyone who has Lynch to give to relevant family members. My mother’s siblings, my siblings, and my sons obviously will have to be tested as well.
Michigan won’t test them until they’re 18 years old. Not sure if it’s different in other states. It goes differently for ethical reasons. We have to wait until they’re 18 to figure out if they have it or not.
Keeping up with the Lynch syndrome screenings
It’s very important to keep up with your Lynch screenings. There are a lot of screenings, and sometimes it feels like a full-time job. I have it now where they’re scheduled at the same time during the year. If you don’t keep up with them, the chances of developing a cancer are [up there].
Cancers grow fast. It’s good to have knowledge to stay on top of it. The one thing that helped me digest having Lynch was now that I know that I have this, it means I know I can use what knowledge I have to stay ahead of the curve. Hopefully, stay ahead of anything developing and staying on top of screenings.
It does get tiresome. I did try talking my GI into switching my colonoscopies from a year to 18 months. When I asked her that, she said no. I was bogged down with all of these tests, and I was so sick of it, I said, “Can’t we just scoot it back 6 months, wait 6 months, have a little break, and then we can have a colonoscopy?”
My GI told me to hold on and sit down. She looked up and found statistics on cancers developing in Lynch patients who’ve already had colon cancer. She said, “No, I think we’re going to keep it at 12 months.”
Then I had my colonoscopy a month later, and she found a polyp that wasn’t there the year before. She comes in and says, “See you in a year! You’re not getting out of this one.”
When it comes to Lynch, stay on top of your screenings, listen to your body, and advocate for yourself.
»MORE: How to be a self-advocate as a patient
Mental and Emotional Impacts of Cancer
What’s the best thing that gets you through the hardest times?
When I was diagnosed with cancer, a lot of people who were cancer survivors — some I knew and some I didn’t know — gave me some advice. One of them really stuck with me through cancer and through other things that I’ve gone through since then.

Best advice you’ve ever gotten
One of them was, ‘Take everything one second by one second. Then when you can move to a minute, take everything by a minute. Then 5 minutes. Then move onto an hour. You’ll eventually get through and it’ll be easier for you to deal with.’
At first I was just overwhelmed with not just the cancer, but all this knowledge that was being thrown about what I should do, what I might not be able to do as far as treatments go.
It was a whole entire other world that blindsided me. I didn’t even know it existed at that point. I just would relax, take whatever I knew that minute, hold that for a minute, then to the next minute.
These little segments of time ended up being longer and longer and longer. I found myself like, “Okay, I can get through this. I went through this the day before.”
Between my colon resection decision and chemo, it was about a month, and my doctor would say, “Well, I’m waiting for the test. We need to get you in chemo right now. You have to be in it. You have to be on chemo by a certain time, or else it’ll be ineffective.”
Every week she would call me saying she didn’t have these tests or these tests, so my anxiety was building inside.
Am I going to be on chemo?
Do I need chemo?
Is the cancer spreading right now?
As advice, it helped me through that part right there. Okay, I don’t have the answers. There’s nothing I can do about it until she has answers, so look to the next hour and see what happens after that. That’s the best advice that I was given during all of this.
How did you tell your kids about the cancer diagnosis?
My youngest son was 1 at the time, so he had no clue. By the time I was diagnosed, my oldest was 4. He was 3 when everything started. He was kind of grasping that something was going on because I was gone for a week, and then I was at home, sitting on the couch, not doing anything. He knew something was up.
I don’t really sugarcoat with anything, and he wouldn’t understand what cancer was. I told him, “Mommy’s kind of sick right now. The doctors are taking care of it. I’m not going to be around you for a little bit right now, but I’ll be better soon.” That’s something he could understand at that point.
I was working through the entire month, wondering if I was going to do chemo or not, working out a way to explain that to him. That never came to pass, so I didn’t have to explain that to him.
That was one of the hardest things was trying to come up with a way to explain what as going on to my sons, to one who could understand something wasn’t right.
Not to sugarcoat, but just say, ‘I understand things aren’t right and that things don’t look right to you, but this is what’s going to happen. This is how we’re going to get through it.’
How does cancer impact your marriage and your husband?
That was something we never saw coming, but he turned out to be very supportive, very helpful. He was working 12 hours a day at that time. As I’m recovering, he would get home and would pick up the slack that I had from going through all this stuff right now. He was wonderful, so I’m very thankful for that.
I think it impacted him in a way that made him realize that life is really fragile, more so than he thought.
Growing up, my father passed away when I was 16. My mom had a progressive form of MS, so I was used to hardships and life not being super easy.
He didn’t have that. When I was diagnosed with cancer, it hit him to where, “Wow, I need to be grateful for things.”
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
What do you wish you had known before cancer?
I wish I had known more about the whole thing. You obviously can’t. I was so overwhelmed with all this information that I had no idea about.
If you’re about to go through surgery or diagnosis, learn everything you can so you understand what the doctors are trying to tell you.

My doctors are brilliant. They’re wonderful people, but sometimes we weren’t on the same level because I had no idea. I was in flux with all this crazy information. I was in this whirlwind that I couldn’t focus.
I had a family member come with me to one of my appointments, and I had them take notes. That really helped out a little bit further on because I could look up what was said and see where my doctor was coming from.
Sometimes it wasn’t clicking because I didn’t know anyone who had dealt with this, especially my age who had dealt with this. That was another thing to realize.
There are people who are out there who understand and people who go through it at young ages and can relate. That was another thing where I felt emotionally very alone, because everyone I had known who had dealt with colon cancer was much older.
We didn’t have the same problems. Their kids were grown; their kids were off to school, off living their own lives. I had these 2 young boys at home. Things are just different, trying to associate myself with someone much older having the same form of cancer.
Perspective on life after cancer
Even now, I’m 4 years out — fingers crossed, going on 5 — I was able to be happier more easily. I tell people as bad as cancer is and as horrible and tragic as the cancer world is, there is some good.
It gives you wonderful perspective on life. I’m so much more grateful. I laugh so much more. I feel things differently than what I did prior.
Where do you find cancer support?
Through social media. I had no clue about colon cancer, so I just started sharing what information I could about colon cancer and risks, and Lynch syndrome on top of that. I eventually started meeting all these people who are my age — some of them are even younger — who had colon cancer or dealt with colon cancer.
It made the very lonesome island that I thought I was on much more friendly and filled it with love. As bad as the circumstance was, you aren’t alone.
It’s a good thing to remember. You aren’t alone if you’re going through this right now.
Survivorship
People are like, “Oh, you’ve been through colon cancer. You don’t have to worry about anything else.” But no. I try not to let it affect me. I try not to let it bother me or detour any of my goals in life. I try to only acknowledge when I’m having my testing done, because otherwise it would bring me down.
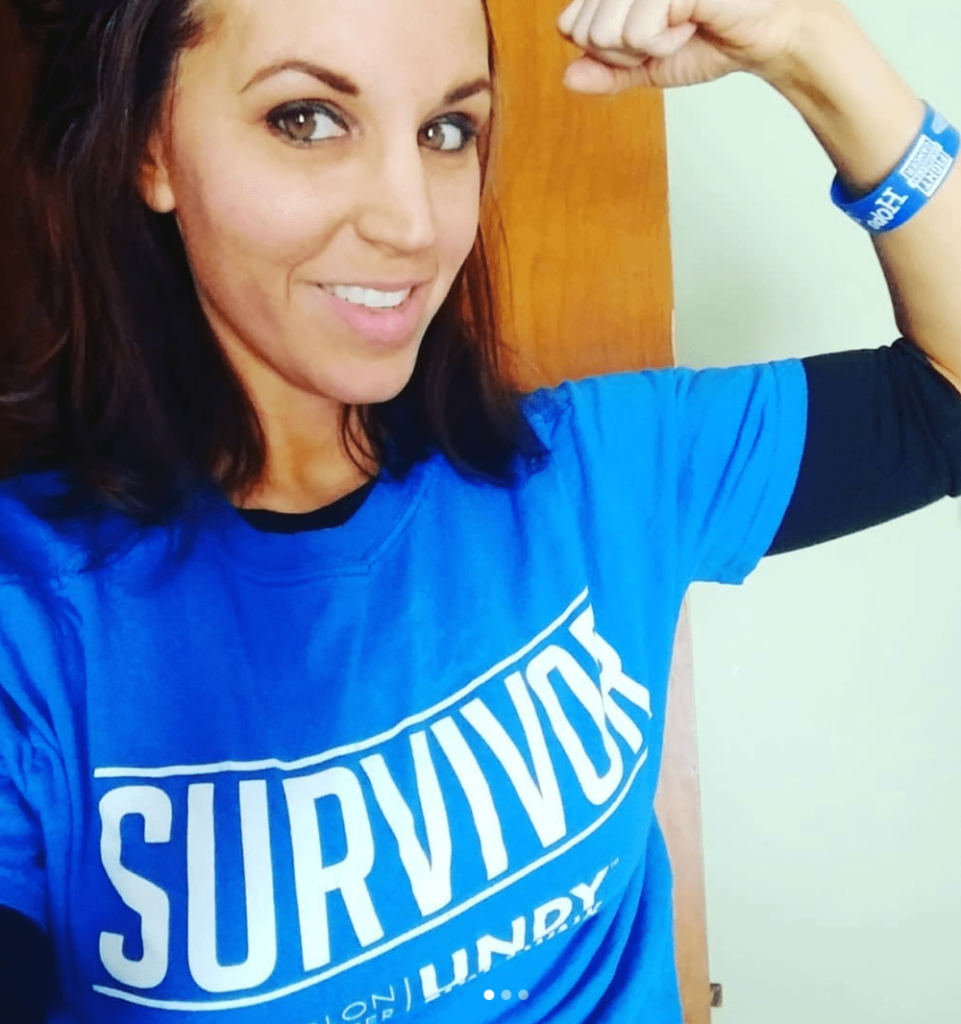
Cancer is never not going to be a part of my life. I participate in a lot of advocacy now for Lynch syndrome and younger-onset colorectal cancer. I try to take what I’ve learned and help other people. It helps me cope with Lynch and with colon cancer. Just trying to use what I went through to help someone else. I think that’s a benefit we can all take from something like this.
As far as cancer and myself go, it’s always going to be a part of my life, whether I have it or don’t have it, because I’m always going to be monitored for it. That’s something many people don’t realize. I just try not to let it bring me down. I try to turn it into something positive.
I had never heard of Lynch, nor did I hear of younger-onset colon cancer when I was diagnosed. I try to take what information I have and spread the word about it, so hopefully if it happens to someone, they won’t be like, “I don’t know anything about it.”
Message to people dealing with a new cancer diagnosis
You aren’t alone. There’s a world full of wonderful people out there to help you through emotionally, physically. It may feel like your world’s crashing down, but there’s so much support out there for you. Take it one second at a time until you can make it one minute at a time. There’s so much love.
Cancer world is horrible. A diagnosis is horrible, but there’s so much love out there and so much support out there.

Inspired by Shannon's story?
Share your story, too!
Colon Cancer Stories
Shannon M., Colon Cancer, Stage 1
Cancer Details: Found the cancer as a result of her Lynch Syndrome
1st Symptoms: Routine colonoscopy found polyp
Treatment: Partial colectomy
Hugo T., Colon Cancer, Stage 1
Cancer Details: Diagnosed 2 weeks after 5 years remission from testicular cancer
1st Symptoms: Inflamed bowel
Treatment: Subtotal colectomy, immunotherapy
Rachel B., Sigmoid Colon Cancer, Stage 1
Cancer Details: The sigmoid colon (or pelvic colon) is the part of the large intestine that is closest to the rectum
1st Symptoms: Stomach discomfort, nausea, bloating, blood in stool
Treatment: Colectomy
Chris T., Colon Cancer, Stage 2
Cancer Details: Discovered Lynch Syndrome after genetic testing
1st Symptoms: Found the cancer as a result of family history, early colonoscopy
Treatment: Partial colectomy
Shannon C., Colon Cancer, Stage 2A
Cancer Details: Diagnosed at 29, tested positive for Lynch Syndrome
1st Symptoms: Severe pains after eating
Treatment: Partial colectomy
Barbara M., Colon Cancer, Stage 3
Cancer Details: Family history wasn’t flagged, should have had colonoscopy earlier
1st Symptoms: Stomach discomfort, difficult to process food
Treatment: Colectomy, Chemo (FOLFOX, CAPOX)
Shelley B., Colon Cancer, Stage 3B
Cancer Details: Had no usual first symptoms, found as a result of routine colonoscopy and endoscopy
1st Symptoms: None
Treatment:Partial colectomy, chemotherapy (FOLFOX)
Lindsay D., Colon Cancer, Stage 4
Cancer Details: Diagnosed at 32, cancer spread to ovary and lung
1st Symptoms: Lump in pelvic area, funny-smelling food, weight loss
Treatment: Chemotherapy, colectomy (surgery)
Lee J., Colon Cancer, Stage 4, Recurrence
Cancer Details: Recurrence then remission
1st Symptoms: Discovered stage 4 cancer from unrelated CT scan
Treatment: Neoadjuvant chemo (FOLFOX), hemicolectomy (partial colon surgery), adjuvant chemo (FOLFOX), chemo post-recurrence (FOLFIRI), liver surgery
JJ S., Colorectal Cancer, Stage 4
Age at Diagnosis: 27l
1st Symptoms: Abdominal pain, blood in stool
Treatment: Surgery to remove tumor, chemotherapy, clinical trial of Keytruda (pembrolizumab)
Haley P., Colon Cancer, Stage 3C
Symptoms: Constipation, fatigue, shortness of breath
Treatment: Surgery, chemotherapy
Amanda G., Colon Cancer, Stage 2A
Symptoms: Gurgly stomach, blood in stool, chronic constipation
Treatment: Surgery (hemicolectomy), chemotherapy (CAPOX), Zarxio
Symptoms: Fatigue, anemia, irregular bowel movements, loss of appetite, heavy periods Treatment: Laparoscopy, chemotherapy, partial hysterectomy
Dania M., Colon Cancer, Stage 4, with Liver and Peritoneal Carcinomatosis
Symptoms: Constipation, diarrhea, terrible bloating, swollen belly, as if pregnant
Treatment: Surgery, immunotherapy (KEYTRUDA)
Stephanie K., Colon Cancer, Stage 3
Symptoms: Very bad cramps, bloating, indigestion, burping
Treatment: Surgery, chemotherapy (CAPOX)
Jason A., Colon Cancer, Stage 3B
Symptoms: Abdominal pressure, fatigue, small amounts of blood in stool
Treatment: Surgery (colon resection), chemotherapy (FOLFOX: folinic acid, fluorouracil, and oxaliplatin)