Erika’s BRCA 2 Previvor Breast Cancer Story
Erika didn’t experience any usual first symptoms for breast cancer. She was in college when her mother was diagnosed with breast cancer for her second time, testing positive for a BRCA2 mutation.
This motivated Erika to approach a genetic counselor and get tested. She was positive also for the same BRCA2 mutation. In this story, Erika shares how she decided to undergo a preventative double mastectomy and reconstruction. She also highlights her advocacy work to help others prevent a breast cancer diagnosis.

- Name: Erika S.
- Diagnosis:
- BRCA2 mutation
- High risk for cancer
- Staging: N/A
- 1st Symptoms:
- N/A
- Mother diagnosed with breast cancer twice, tested positive for BRCA2 mutation, motivated Erika to check with genetic counselor for testing
- Treatment:
- Surgery
- Preventative double mastectomy
- Direct implant reconstruction
- Surgery
I think we have a tendency to make everything either all good or all bad, whereas with my mutation, it’s a mixed bag. I’ve seen my mom go through cancer, and I feel really fortunate that I’m able to avoid that outcome.
I do feel very grateful that I was able to have surgery on my own terms and on my own timing.
Erika S.

- Background and Family History
- Genetic Testing
- Making Decisions
- Surgery
- What did you have to do before the mastectomy?
- Was there anything surprising or painful about the whole process?
- What was the preparation before surgery like?
- Describe the arrival at the hospital
- What came right before going into the operating room?
- How long did the surgery take? How did you feel when you woke up?
- How long did you have to wait to shower?
- How long did it take for you to fully recover?
- Reflections & Follow-Up Procedures
- Work With BRCA Awareness
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Background and Family History
How did all of this start to unfold?
My mother is a 2-time breast cancer survivor. She had cancer for the first time when she was 28 years old, back in 1993. This was before doctors knew that there were hereditary mutations, called BRCA mutations, that elevated your risk for breast cancer.

She had stage 1 breast cancer, underwent a lumpectomy, chemotherapy, radiation, and then she was in remission for about 14 to 15 years. She had a second breast cancer diagnosis in 2007, which was my senior year of college.
She’d had 2 breast cancer diagnoses under the age of 50, so one of her doctors at UNC finally recommended that she get tested to see if she had a BRCA mutation. It turned out that she does, which meant that I have a 50/50 chance of carrying it as well.
At the time, I was getting ready to graduate from college and start law school, so I didn’t want to undergo testing at that time. I graduated, moved to New York, and ended up working in a pretty high-pressure, stressful law firm environment.
Finally, a few years later, I decided to undergo genetic counseling and testing because I was getting very close to the age that my mom was when she had had cancer for the first time.
I saw a genetic counselor, Julia Smith, at NYU Langone. Ms. Smith specializes in working with women in their 20s and 30s who are dealing with a hereditary or familial risk of cancer.
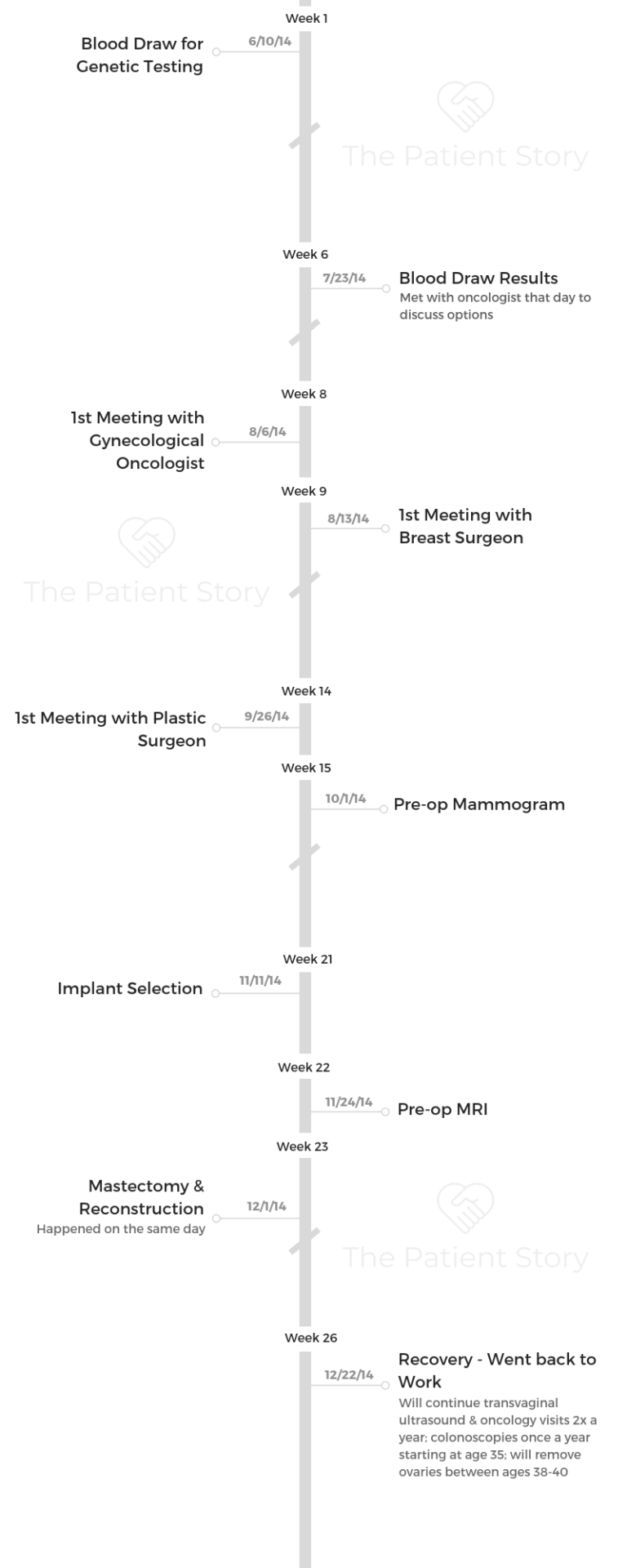
The results came back in 3 weeks. I had inherited my mom’s BRCA2 mutation, and because of our family history, the surgeons that I met with recommended that I undergo a preventative mastectomy as soon as possible.
I interviewed with a few different surgical teams, and I had a preventative mastectomy in December.
Genetic Testing
What did the genetic testing cost?
It’s really interesting because I am sometimes asked about this by people, or people will tell me they don’t get tested because of the expense involved.
However, there’s a criteria for who should be tested for BRCA mutations, and if you meet that criteria, your health insurance company will cover the cost of testing.
In my instance, because I knew that my mom had a BRCA2 mutation, I brought a copy of her test results to my appointment. What they do in genetic counseling is actually sit down and go over your family tree.
They will ask you about cancer diagnoses on both sides of your family, mother and father, because men can carry and pass down BRCA mutations.
After they went through my family history, they took a vial of blood that was shipped off for further testing. Since we knew that my mom had a mutation, they didn’t actually have to test the whole gene for mutation. They only tested to see if I had the same particular mutation that my mom had.
I think with insurance, the cost of my testing was $80 out of pocket.
What did the actual testing process involve?
It’s a blood draw. They took a vial of blood from me [and] sent it off to what I believe is still the biggest BRCA lab.
How long did it take to get the results?
It took somewhere between 3 to 4 weeks. I got tested in June, and I got a phone call to come in for the results in early July.
What were you feeling and thinking while you waited?
I had known for a long time that I needed to get tested. I’d known since 2007. By the time I finally was able to motivate myself to do it, I was just really anxious to know the results and what the outcome was going to be.
For those 3 to 4 weeks in between, I just spent a lot of time thinking to myself, “Okay, well, what’s going to happen if it is positive for a mutation? What am I going to do? What actions am I going to take?”

I definitely spent a lot of time researching online about options for BRCA carriers. I’m really fortunate. My college roommate is a doctor. She’s a pediatrician and her husband is a cancer researcher, so I spent a lot of time talking with them about what all the latest science was.
I think the best way to describe it is that there was just this low level of anxiety in the background while I was waiting for the test results.
Making Decisions
Can you describe how you felt when you got the call to go in?
It was just a call to come back and meet with the genetic counselor who would give me my results. I was dating someone at the time, who came to the appointment with me. It was a very somber, serious meeting.
When I had come in to do the blood work, Dr. Smith had said to me, “Well, even if it’s positive, we have all these options. We can do surveillance; you can take tamoxifen. It’s nothing to panic about since we just have so many different treatment options.”
When she came in with the actual test results, it became much more real. She was like, “Look, it’s your life, and we will give you all the different options that you can pursue.” Then she told me that I could opt for what’s known as “enhanced surveillance.”
That’s where you have an MRI and a mammogram every 6 months. Some people also take tamoxifen, which is a drug that’s normally given to people who have been diagnosed with breast cancer, to keep it from coming back.
It has been shown to have possibly some preventative benefits in BRCA mutation carriers. There’s also the preventative mastectomy, which is the option that people are most familiar with.
Dr. Smith said to me, ‘Look, given the fact that your mom has had cancer twice’ — she had triple-negative cancer, which is a more aggressive type of breast cancer — ‘we just really think that you should pursue a preventative mastectomy option.’
She gave me a list of people to reach out to. When people think about BRCA, they don’t think about the fact that it also impacts your risk for ovarian cancer, melanoma, pancreatic cancer, and colon cancer.
I left the appointment when I got the results with this whole list of doctors that I needed to speak to in order to start getting screenings for other things.
How did you process all the information?
It’s interesting because I always had a feeling that because of my mom’s history, I would be positive for a mutation. I think there was a part of me that thought, “Okay, well, this is sort of inevitable. This is what we’ve thought about and planned for.”
I was very caught between sometimes just trying to dive in and just become kind of like a machine, thinking, “Okay, I’ll just make this appointment, this other appointment, and that appointment.” Then I’d just look for some research and so on.
There were definitely some times where I just thought about how overwhelming it all was.
At that point, I was going to the doctor all the time, having to take time off work, and paying to see specialists. lt was not what I thought my 29th year on this planet was going to be like.
I definitely bounced between just being extremely focused and having these very anxious and depressive moments.
Did you have to see specialists?
Julia Smith is an oncologist, but she is certified to do genetic counseling and testing. She referred me to a few different people.
This included an obstetrician-gynecologist who works with BRCA carriers, because of the enhanced ovarian cancer risk. She also referred me to a team consisting of a breast cancer surgeon and a plastic surgeon.
With the preventative mastectomy, there will be 2 surgeons working together to come up with the surgical and reconstruction plan. Dr. Acharad, who is a cancer oncologist and breast surgeon, did my surgery along with Dr. Choi, who is a plastic surgeon. They’re both affiliated with NYU. They do the surgery together.
In my instance, I was able to have a surgery that’s referred to as a direct implant, which means that the breast removal and the reconstruction implants were all done in one complete surgery.
That’s not the case for all patients. Some have to go through what’s known as the expander process. That’s when they put in a temporary implant under the skin in order to stretch the skin out to accommodate the implant down the road.
I was just very fortunate. I was a 32C before the surgery, and I stayed a 32C. Given the size of the implant, they were able to do it all in one step.

Why do some people not have the same options you did?
It has to do with size, as in the elasticity of the skin. For some people, the skin needs to be stretched out more in order to actually accommodate the size of the implant.
For some people, if they’ve breastfed before, they’re not able to do it. It just varies from person to person. Some people will go up in size; some people will go down. It’s very individualized.
Did you ever consider another option besides reconstruction?
I always went into it knowing I would want to pursue some type of reconstruction option. When I made the decision to get tested, one thing that made me feel okay about getting the surgery is that back in 2014, more surgeons had started doing what’s known as a nipple sparing mastectomy.
It’s a type of mastectomy where you actually are able to keep the nipple. The incision is made underneath the breast, so it kind of results in a much more natural outcome.
I never considered not getting reconstruction, and the easiest thing about the process was knowing that I could do the nipple sparing in one step. However, it’s a very personal choice for people.
Surgery
What did you have to do before the mastectomy?
I got the results in July, and then I met with Dr. Acharad and Dr. Choi in August. They scheduled pretty far out into December.
I met with both of them separately to talk about what their approach would be, particularly with Dr. Choi. We met over 3 or 4 times — 1 time for me to get comfortable with her, another time for her to do some preliminary photos, and then the third time to actually go in and pick out the implants that I was going to use for the actual surgery.

There’s silicone, there’s saline, there’s round, there’s teardrop, and there’s textured and non-textured. In addition to that, there’s a lot of pre-op work that you have to do.
I had both a mammogram and an MRI the month before the surgery, just to make sure there were actually no signs of cancer there.
Additionally, because of the ovarian piece, I started seeing an OB-GYN. What they do for BRCA mutation carriers is make you undergo a blood test called the CA 125, which is a marker in your blood that if elevated can be a sign of ovarian cancer.
They also do what’s known as a transvaginal ultrasound, which is where they go in and look at the ovaries to see if there’s anything abnormal.
Since there is a slight enhanced risk of melanoma, I also saw a dermatologist and an ophthalmologist, because it’s most common to get melanoma in the skin around the eye.
I also just spent a lot of time trying to physically get in shape because I’d been told the surgery would be easier if I was in good physical condition. I started going to barre classes like 3 or 4 nights a week.
Was there anything surprising or painful about the whole process?
I started seeing a therapist after I had the surgery, about 2 months afterwards. In hindsight, and this is advice that I give a lot of people, I wish I would’ve started seeing a therapist before. It is a really complex emotional journey, and I wish I’d had someone working through that with me.
I don’t think there was anything that was surprising, but I had never undergone any type of surgery before, so it was a little bit nerve-wracking to go through surgery.
Same with having to be put under anesthesia. The recovery was certainly easier than I had anticipated. I was back at work after about 3.5 weeks. When you have a preventative mastectomy and your body’s not going through cancer or dealing with cancer treatments, I think the process is easier to recover from.
The last thing that I’ll say is that even when you’re having a mastectomy preventatively, I think it’s still very scary. I think it’s still a loss of body parts, and I think people forget that.
It’s okay to grieve and to mourn.
Which is another reason why I always tell people, even if you just talk to a therapist one time, I think it can be really helpful for processing all of those feelings.
What was the preparation before surgery like?
I was delayed in getting my MRI, and they called me and told me I needed to get an MRI or else I couldn’t get the surgery. That was like 2 weeks beforehand, because they needed to review the scans.
In terms of the night before, I did have to fast for the 12 hours beforehand. I actually went to a really nice brunch with friends the Saturday before the surgery. My surgery was on a Monday, and then I had to fast for the 12 hours the night before.
My surgery was in the afternoon, around 1:00 or 2:00 p.m. The only thing I’d had was coffee, so when I woke up, I was starving.
Describe the arrival at the hospital
My mom’s a teacher, so she was able to take a week off of work and fly in from New York. She went to the hospital with me that morning. We took an Uber to the hospital together.
I was really fortunate that I had a few friends who are able to take shifts at the hospital sitting with her while I was in surgery.
When I came out of the recovery room, my mom was there, along with a handful of some really close friends.
What came right before going into the operating room?
When you get there, you have to fill out the final surgical papers. Then you’re in the back, where they do the last vital check and all that type of stuff. Then they actually let you walk into the OR.
My mom was able to walk with me from the pre-op room to the OR, basically until I walked in. I will admit it was a little bit scary, because they put you on the table and strap you in.
All I remember was just making small talk as they were putting in the anesthesia, and then 5 seconds later just being completely knocked out. The next thing I remember is waking up in the recovery room. That walk down the hallway is a little scary. It’s all sterile; it’s white.

How long did the surgery take? How did you feel when you woke up?
My surgery was about 5.5 hours. I definitely remembered waking up and being extremely out of it because of the anesthesia, but also the sensation and weight of the implant.
It was just so new. It was pretty late in the evening when I woke up, so I really just wanted to go to bed.
The nurses told me that I had to go to the bathroom before I could go to bed, so I got out of the bed to do that.
I remember standing up and almost falling over, just because my body was getting used to something new being there, and it felt really strange.
I definitely had bad moments after I got home. Since it was my first surgery, I’d never been that physically weak before. I needed help to go to the bathroom and pull myself up out of the bed by myself.
My mom would have to come in and pull me up out of the bed. That first week was tough because I knew it was a good thing to do and I’m happy that I did it, but I’ve never felt so physically helpless before.
You also can’t take a shower. You have these post-mastectomy drains that are installed that are there for about a week. They collect the runoff blood, so you have to empty those out every couple hours. The first week was a lot to handle. Then it just got easier and easier.
How long did you have to wait to shower?
You can’t shower while the drains are in. My surgery was on Monday, and then they came off the next Monday.
How long did it take for you to fully recover?
I went back to work after 3.5 weeks, although I went back on a reduced schedule.
In terms of fully feeling better, it probably took closer to 2 or 3 months, just because I live in New York, so I walk all the time. I remember that the first couple of months, I would walk a pretty short distance and feel pretty exhausted.
Reflections & Follow-Up Procedures
How did it feel to go through all of this?
I think we have a tendency to make everything either all good or all bad, whereas with my mutation, it’s a mixed bag. I’ve seen my mom go through cancer, and I feel really fortunate that I’m able to avoid that outcome.
I do feel very grateful that I was able to have surgery on my own terms and on my own timing. I kept thinking to myself that if I did have a BRCA mutation and if I were to get breast cancer, I’d be likely to have to have a double mastectomy anyway. I figured I should just do it while I’m healthy and on my own time table.

At the same time, it was certainly very disruptive. I was an attorney at the time, so having to take off a lot of time from work and having to explain it to family and friends was difficult, especially because I didn’t actually have cancer, just a high risk of cancer.
It’s a weird thing to explain. I’m ultimately happy about what I did, and I would do it all over again, but it is certainly a journey.
I’m very thankful for my therapist, friends, and some of those support groups I’ve found. Those have all been instrumental in processing all of these complex emotions.
What’s the follow-up protocol?
I still see Dr. Julia Smith once a year. She does a manual breast exam for the breast tissue that is left. For the ovarian piece, I still undergo the CA 125 blood work and the transvaginal ultrasound every 6 months.
I see a dermatologist and an ophthalmologist once a year. I will start undergoing colonoscopies when I’m 36 or 37, and ultimately, I’ll have my ovaries surgically removed somewhere between 38 and 40. I’m 34 now.
Are the follow-ups indefinite?
The ovarian cancer piece will be until the ovaries are removed. The melanoma and the colonoscopy stuff will be in perpetuity, and I would imagine the breast stuff is in perpetuity as well. I’ve been doing it for the past 5 years. Then the implants have to be removed every 10 years or so.
It is ongoing. I tell people it’s almost like having a chronic illness. You’re not ill, but there’s ongoing management. They still are finding out a lot of things about BRCA mutations.
For instance, now BRCA mutations are linked to pancreatic cancer. I am supposed to start seeing a specialist for that. I just haven’t made the appointment yet.
How did you handle everything after surgery?
It’s just such a roller coaster of happiness, then resentment for having to do this. There are probably things going on hormonally because you’ve lost breast tissue.
Going to therapy was really instrumental in helping me process all of those feelings — the feeling of being happy that I’m avoiding something, and that I’m resentful that this was the best option that I had.
I was really fortunate. Dr. Julia Smith recommended me to a therapist who works with a lot of other BRCA mutation carriers, and that’s been really helpful.
I do a lot of writing about BRCA, so I’ve made a network of other women of color BRCA carriers who actually are all attorneys as well. I meet with them every month or every couple months in New York. That’s been really helpful as well.

Have you seen a greater response to this because of your work?
I think it’s sometimes slow going because it’s not my full-time job, and I’m not an academic. I am encouraged because I do get emails from people occasionally or LinkedIn requests from people who say, “I saw something you wrote, and that encouraged me to go seek out a genetic counselor,” or, “Can I meet with you and talk about this thing?”
I would say probably on a broad level it seems slow going, but even this weekend I had a friend say to me, “I know this woman. She’s a woman of color, Filipino, she just found out she has BRCA, and she just really needs someone to talk to.”
We talked, and I referred her to my team at NYU. I try to be happy about those incremental processes, because I think for each person you find, their family members get tested. You have to just sort of start at that micro level, if that makes sense.
Did you ever talk about possible fertility complications?
I did meet with someone about fertility preservation, which is essentially freezing the eggs in the event that I had an ovarian cancer diagnosis or if I didn’t have children before my ovaries needed to be removed.
I went to the consultation in 2016 only to find that this a very expensive process. It’s somewhere between $15,000 to $18,000 to do fertility preservation.
I didn’t feel that strongly about having kids, and so I just ultimately decided that if I wanted to have kids, I would try to arrange my life in a way that I would be able to do it without having to do the egg freezing.
Work With BRCA Awareness
What kind of work do you do to bring attention to BCRA?
When I found out I had BRCA, I just would go and do a lot of research about it. I guess this is just because I’m a lawyer. I would read medical studies and all these type of things.
What I would come across is that BRCA mutations are commonly associated with the Ashkenazi Jewish community. It’s a 1-in-40 rate in that community.
I would find all these papers that made us think that there’s also probably a lot of BRCA mutations in African American women, but we don’t know because they don’t get tested. They don’t get referred to genetic counseling and testing at the rates that they should be.
I just thought that was really incredible, because from a breast cancer perspective, black women tend to get diagnosed earlier. They’re usually diagnosed with more aggressive cancers, and they’re more likely to die from breast cancer.
Therefore, if you can at least know if you have one of these BRCA mutations, or just knowing of one in your family history, you can try to avoid some of those later outcomes.

What I started doing in 2015 was hosting events with local oncologists, and then using myself as a patient speaker to go out and educate black women on why they should know their family history, how their family history impacts their cancer risk, what a genetic cancer is, what happens in a genetic counseling appointment, and what it means to have BRCA.
I usually have tried to do those once or twice a year, usually with black women attorney groups — because that’s who I am — or at churches.
Earlier this year, I created an Instagram account, Black and BRCA, to collect stories from black BRCA carriers.
Now people, advocates, doctors, [and] foundations sort of realize that this is a population that is impacted by this problem.
Do you have anything to say to people who are on the fence about getting tested?
When people think about getting tested, they’re like, “If I get tested, I have to have surgery.” That’s not necessarily true.
The science is getting a lot better in terms of really being able to calculate what your actual breast cancer risk is, depending on what your mutation is.
My surgery was the best option for me because of how aggressive and how young my mom had been when she had cancer. I had multiple doctors tell me if my mom had cancer in her 40s or her 50s, I could’ve delayed having a preventative mastectomy.
The science is getting a lot better, and so you shouldn’t think of it that way.
There are a lot of doctors and researchers who are working to improve the options, and ultimately I think it’s always just better to know so you can do something about it versus not ever having that information.

Inspired by Erika's story?
Share your story, too!
Previvor BRCA2 Stories
Erika S., BRCA2 Mutation
Cancer Details: Previvor
1st Symptoms: Family history of breast cancer, no physical symptoms
Treatment: Preventative double mastectomy, direct implant reconstruction
...