Stefanie’s Stage 3 IDC Triple-Positive Breast Cancer Story
Stefanie shares her stage 3 triple-positive breast cancer diagnosis, undergoing chemotherapy and side effects, lumpectomy, and radiation therapy.
In her story, Stefanie also highlights how she navigated the hair loss post-chemo, how she approached work during treatment, and the impact of the breast cancer diagnosis on her marriage.

- Name: Stefanie H.
- Diagnosis (DX):
- Breast cancer
- Invasive ductal carcinoma (IDC)
- Triple positive (Triple +)
- Age at DX: 33
- Staging: 2 initially, then 3
- 1st Symptoms:
- Lump in breast
- Treatment:
- Chemotherapy
- 4 rounds of Adriamycin & Cytoxan
- 12 rounds of Taxol & Herceptin
- 9 months of Herceptin
- Surgery
- Lumpectomy & lymph node removal
- Revised lumpectomy
- Radiation
- 30 treatments to chest
- Chemotherapy
If my cancer is the worst thing I go through in my life, I’m very blessed.
I know there are people who have had it way worse than I did with cancer and otherwise.
I just tell myself what I’m grateful for all the time. I have my family, and there’s people out there who don’t have that. I just try to count my blessings.
Stefanie H.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
I was pregnant. I gave birth on October 4th, so 2 days before I found out everything. I found a lump in my breast while I was pregnant.
I was 5 months along when I noticed it. I was usually in and out at my appointments, so I brushed it off and thought it was a clogged duct. I just didn’t think anything of it.
After I gave birth, one of the postpartum nurses said, “You have a lump on your breast.”
I said, “I know. It’s a clogged duct, and it’s gonna go away when I start nursing.” They did a sonogram that night, and my OB/GYN felt horrible for me.

I look back, and I think ignorance is bliss in a way. It’s a blessing that I didn’t know about it during my pregnancy, because I would’ve stressed out. My doctor said if I had found out when I was 8 weeks pregnant, there would’ve been other options, and who knows what I would’ve done.
The way it worked out for me was okay. I’m not saying it would work for everyone, but it worked for me.
How did you get the diagnosis?
They did the sonogram on the night I gave birth. They did a biopsy the next day since the sonogram was inconclusive.
They told me I could call on the 6th for my results. I was still inpatient from giving birth after my scheduled C-section.
My husband was working because I told him I was going to need a lot of help when we got home, so I wanted him to be working as much as he could until then.
I was alone and called the radiation department. The doctor said, “I’m so sorry. You have cancer.”
I got out of the hospital the next day, but I was just ready to go home right then. I wanted to crawl into my bed and forget this was happening.
»MORE: Patients share how they processed a cancer diagnosis
Chemotherapy
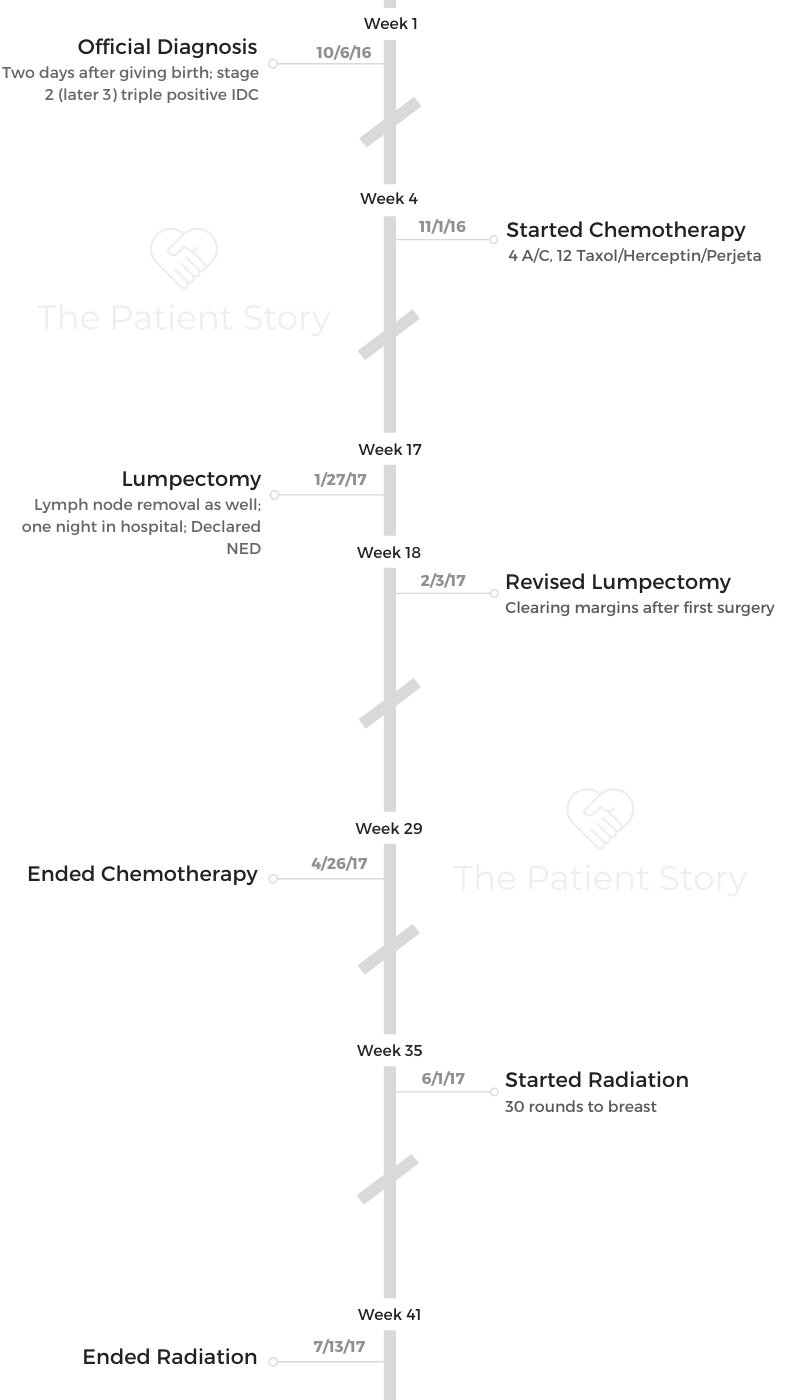
What was your treatment plan?
Originally, I was going to do my 4 rounds of AC and 12 rounds of Taxol and Herceptin. Then we were going to do surgery. We decided on a lumpectomy, especially because my little one was so small.
My surgeon said she was confident she could get it all, so that’s what we were gonna do. You make plans, and God laughs.
My ejection fraction was really low at one point, so they had to stop my Taxol and Herceptin. We did the surgery early. Because I had to stop chemo for a while, she said they were going to go ahead and operate.
That gave my heart some time to rebound. It did bounce back. I was under the care of a cardio specialist.
What was your chemo regimen like?
I had AC every other week. Then I did 12 rounds of weekly Taxol and Herceptin. The first chemo was terrifying. It was the scariest thing I’ve ever experienced.
That’s when everything became real for me. You see all these people already well into their treatments, and you see what you’re going to become.
They hook up to this bright red bag of chemo, and it’s so scary looking. They have to tell you all the potentials of what could happen. They have to tell you all the possible wors- case scenarios, and you’re sitting there wondering if it’s going to happen to you.
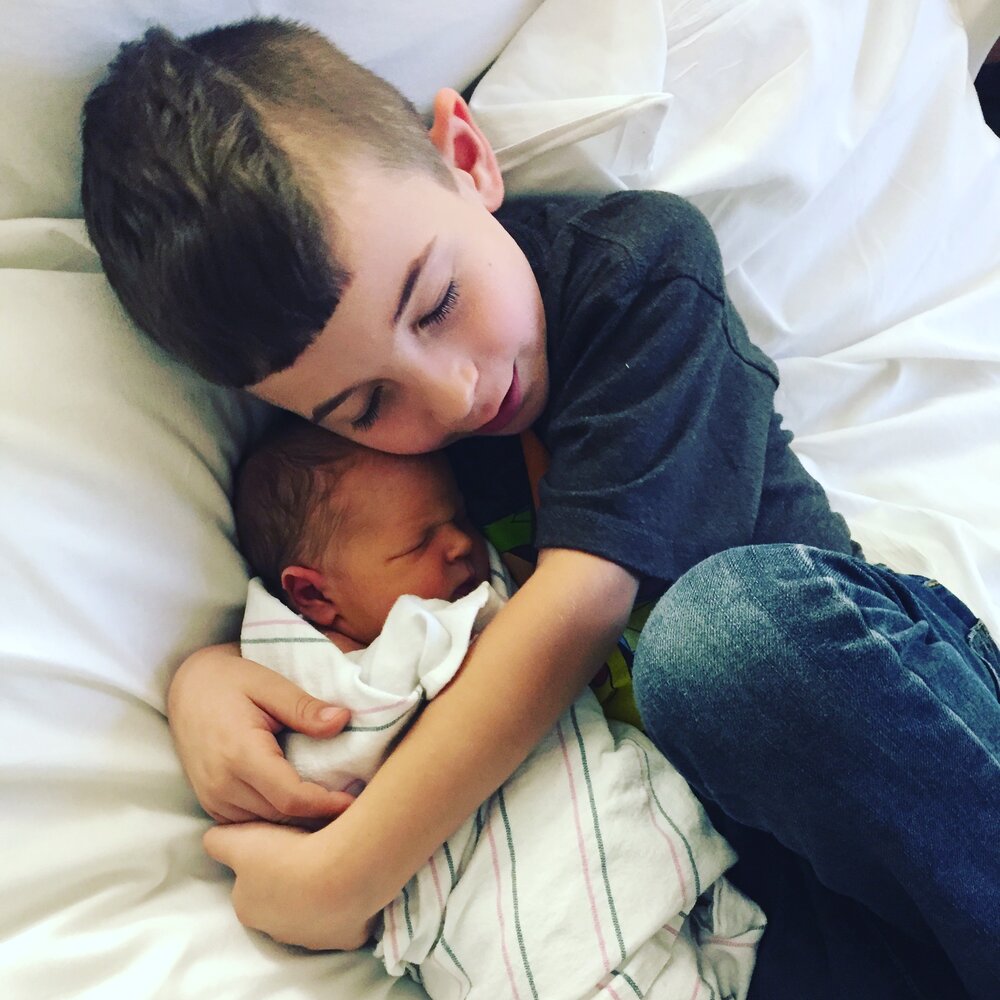
I had a 6-year-old and a less than 1-month-old at home. I had a lot to worry about. Luckily, I had the nicest nurses. As scary as it all was, I knew it was going to be okay.

What side effects did you experience from chemo?
I was fine the day after infusions. The day after that, I felt like a train hit me. My bones ached, I couldn’t hardly function, and I was nauseous.
They had given me anti-nausea medications, but I felt fine the day before, so I didn’t take them. I learned very quickly that even if you’re not feeling nauseous, you should still take the medicine.
I would be tired and need a day to recuperate, but then I’d be okay. It wasn’t so bad. I felt so much better on the Taxol and Herceptin than I did on the AC.
I had some fatigue and diarrhea a couple of times, but other than that, it was so much easier. My hair started growing back during it, which I was not expecting.
»MORE: Read other cancer patient experiences with chemotherapy

Surgery
What was your surgery like?
They did a lumpectomy and lymph node removal on January 27th. I had a revised lumpectomy the following week because they didn’t clear the margins the first time.
I told her, “If you can’t clear the margins after this, just give me a mastectomy.”
At that point, I just wanted the cancer gone.
I was thinking, “You just need to get this over with.” They told me they weren’t sure about my lymph nodes when I went in for surgery. They said if they wound up needing to take them, I would wind up having to stay overnight in the hospital.
I was sad about needing to be away from my kids. I was nervous and wondering what was going to happen. At the same time, I was confident in my surgeon and knew they were cutting out what they could.
There was part of me that was just glad we were doing something and glad to be there fighting the cancer. There was another part of me that was nervous and just wondering what was going to happen.
I ended up having to stay overnight. Calling your little kid and telling him you’re not going to be home that night is terrible. Not being able to hold your baby is one of the worst feelings in the world.
»MORE: Read more patient experiences with surgery
What was recovery from surgery like?
I remember waking up from surgery, and my surgeon being there hugging me. She told me, “It’s good. You’re done. It’s all over.” She’s amazing.
I wasn’t in any pain when I woke up, thankfully. I had a drain, and I didn’t like that. That was a little uncomfortable. I wasn’t happy about having to stay overnight.
My husband would probably tell you I was argumentative because of that. Once I calmed down about that, I was okay.
They were giving me Tylenol intravenously, and that worked really well. They told me I was going home the next day. I just kept that in my head, and that’s what helped me make it through.
When I got home, everybody took a turn to come and stay and help me. I couldn’t lift anything because of the lymph node removal. My best friend came and stayed for a day. My grandma, my aunt, and my husband took a day off, and everyone was just so wonderful.
It really did take a village to get me through all this. I’m so lucky to have my village. I can’t imagine going through what I did without my family.
You had more treatment after surgery
After surgery, I went once a week for 9 months to get Herceptin. It’s really nothing compared to the other chemo I was doing. At that point, I was feeling so fine that it was mostly just an inconvenience.
Describe the radiation therapy
I also had 30 rounds of radiation. It was horrible. It’s not because it’s painful. I did get a burn, but that’s not why it was horrible. You don’t feel it while you’re getting treatment.
It was just an inconvenience because you have to go every single weekday. If they’re backed up, it just takes forever. The treatment itself isn’t long, but the wait times could be terrible.
»MORE: Read other patient experiences with radiation therapy
Reflections
Can you talk about hair loss?
By the grace of God, I didn’t lose my hair until the day after my son’s baptism. I was so glad I had hair for that.
My mom and other people would say, “It’s just hair,” but it’s never just hair. The hair loss was heartbreaking.
I shaved my head. I wasn’t about to let it just fall out. My scalp actually hurt, too. It was my hair follicles dying. It felt better to shave it.
»MORE: Patients describe dealing with hair loss during cancer treatment
I wore wigs for a little while. I stopped pretty early on, though, because they’re annoying and itchy. I don’t care how nice it is; it’s still a wig. I was more comfortable not wearing anything than wearing a wig.
My kids were so used to me being bald, so it was fine for me. Their friends came over one day, and they were horrified by my bald head. I had to apologize profusely, and of course, I was crying.
I hated that my kids’ norm was mommy not having any hair. That shouldn’t be normal for any child.
Did you work through treatment?
I went back to work in December in between getting AC and Taxol. My job let me take off one day a week for treatment when I started Taxol.
I’m a teacher, and at that point, I was teaching special ed pre-school, so that wasn’t easy. I was grateful my job was accommodating.
I enjoy routine, so going to work was a break from reality. It was 6 hours a day I could not think about cancer and just do my job. In a way, I think that helped get me through it.
»MORE: Working during cancer treatment
How did cancer affect your relationship with your husband?
My husband and I already had one son. We got married and had a baby right away. That wasn’t the easiest road, and we have our own notions of how things should be.
I’m opinionated and high energy. He’s more passive and quiet. We’re complete opposites.
My husband was terrified in the beginning. We just had our second baby, and here his wife is with a cancer diagnosis. He didn’t know what was going to happen.
He did everything for me despite being scared himself.
Anything I asked of him, he did. I couldn’t have asked for somebody better. He wasn’t singing from the rooftops about how amazing I am, because that’s not his style.
He was just so supportive. He kept it together when I couldn’t. The laundry was done, the kids were fed, and everyone was where they needed to be.
Looking back, I realize how important it was to me that he took care of those little things.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer


Being a cancer patient and a mom
I had to learn really quickly that I couldn’t do everything I was used to doing. I wasn’t able to make lunch or get my kid on the bus.
I was tired. I just had to resign myself and realize when I couldn’t do things.
Emotionally, it took a toll on me. I cannot imagine leaving my children without a mother. Especially the timing of my diagnosis.
I went through a moment of “why me,” because we had a newborn baby. It was just terrible. I heard the best sound of my baby crying and heard the worst thing you can hear 2 days later.
I have my mother, and I know that everyone would step up and do what they had to do, but it’s not the same. Those are my kids. They’re everything to me.
I asked my doctor right at the beginning, ‘Am I going to die?’
She looked at me and said, ‘No, you’re not going to.’
I just had to trust her.
»MORE: Parents describe how they handled cancer with their kids
Transitioning into survivorship
I’m so hypersensitive to my body now. Any little thing can alert me. I live with a little bit of fear. I remember in the beginning thinking, “I don’t want to go through that again.” I really don’t, but I did it once. I know I could do it again if I had to.
Now, I’ve settled down. There are days where I forget I had cancer, and there are days when it feels like it was yesterday.
Every day is different for me. I can go days without thinking about it. I feel compelled to share my story where I can.
If my cancer is the worst thing I go through in my life, I’m very blessed. I know there are people who have had it way worse than I did with cancer and otherwise.
I just tell myself what I’m grateful for all the time. I have my family, and there’s people out there who don’t have that. I just try to count my blessings.
What advice do you have for someone who has just been diagnosed?
Stay positive even on your worst days. Try to find something to be grateful for, even if it’s the littlest thing. Don’t be afraid to lean on other people for help. Somebody set a meal train up for us, and that was amazing.
Don’t feel embarrassed about accepting the help someone is offering you. Take the help. Don’t be afraid to ask for it either.

Inspired by Stefanie's story?
Share your story, too!
Invasive Ductal Carcinoma
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation