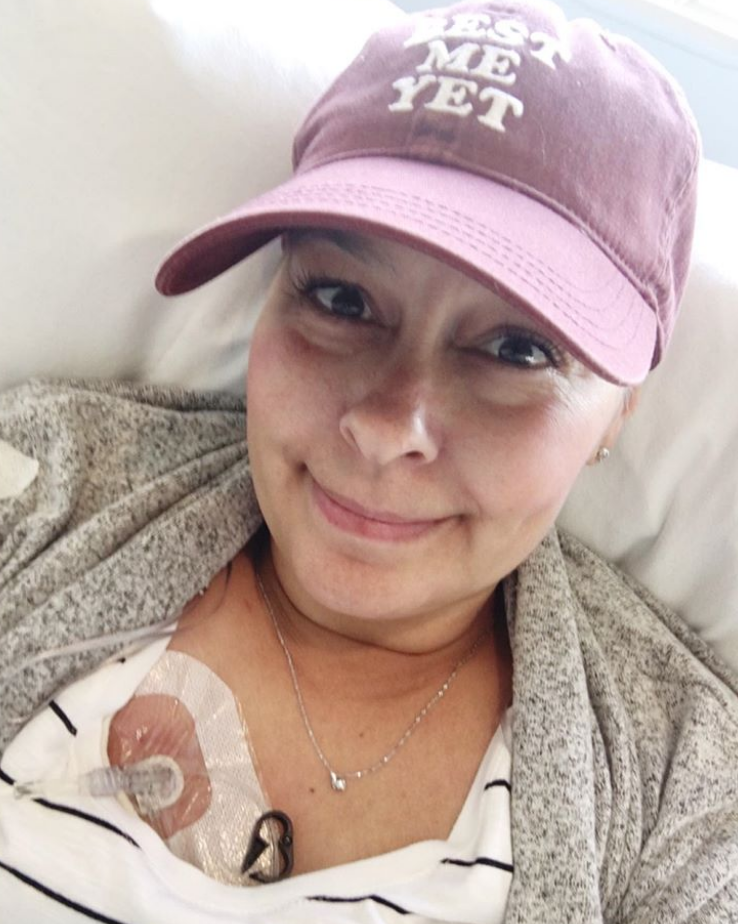
Renee’s Stage 3-4 Relapsed IDC, HER2+, Metastatic Breast Cancer Story
Renee shares her story of stage 3 breast cancer before she relapsed and was staged at 4, or metastatic breast cancer. She details how she was able to get through chemotherapy, a bilateral mastectomy, and radiation.
In her story, Renee also highlights how she parented with cancer, how the diagnosis impacted her marriage, and how she has managed treating her cancer like a chronic illness.

- Name: Renee N.
- Diagnosis:
- Breast cancer
- Invasive ductal carcinoma, HER2+, at age 46
- Staging: 3
- 1st Symptoms:
- Lump in breast
- Treatment:
- Chemotherapy
- AC-T
- 4 rounds of AC & 4 rounds of Taxol
- Herceptin
- 18 infusions
- AC-T
- Surgery
- Bilateral mastectomy
- Radiation
- 25 sessions directed to chest
- 5 sessions of SRT brain radiation
- Chemotherapy
Take it one day at a time. I know they say that, but it’s so true. You are going to be so overwhelmed. I joined Facebook groups at first and had to unfollow them.
There is so much advice out there. You have to decide what’s best for you.
Renee N.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
My kids and I were dancing around. My son accidentally knocked my boob, and it hurt really bad. I went upstairs and looked at it and felt it.
It felt hard, and it felt big. I started crying right away. I suspected it was cancer.
What happened at the doctor?
I called my family doctor and saw her a few days later. All she did was feel it, and she told me it was breast cancer.
She was going to send me for screening, but she was pretty sure. She had seen a lot of breast cancer cases before.
For the first 2 weeks, I wasn’t really okay. I came home and worked from home for a bit. I was a mess. I was terrified.
I was waiting for all the testing. When I got those results, I found out it was stage 3.
Chemotherapy
What was the chemo regimen?
The surgeon said I would probably do chemotherapy first and maybe we could do a lumpectomy, but that depended on how well chemo worked.
I did 4 rounds of AC (Adriamycin & carboplatin) chemo. My first round put me in the hospital. I had an infection in my port. I ended up in the hospital again after my third round. We reduced the dose for my fourth round.
Then I had 4 rounds of Taxol. That wasn’t as bad. I had a lot of bone pain with the first round of that, but the next 3 were okay because they adjusted my meds.
Can you talk about your side effects from chemo?
Days 3 to 6 were the brutal days. With AC, I was nauseous from the start. My nurse told me to eat little meals throughout the day. That really helped, but I wasn’t very hungry, so I had to force myself.
My appetite wasn’t bad on the Taxol. I didn’t have many problems with that.
On Taxol, I lost my eyebrows and eyelashes. I had lost my hair, and then I just looked like an alien.
Can you talk about hair loss?
I’m a really vain person, so I’m shocked at the fact that the hair loss didn’t bother me. I was more concerned about getting the meds in me and getting the cancer gone.
I shaved it when it started falling out. I had cut it short, and I thought it was cute.
It hurt when it was falling out. People had said that, and I wasn’t sure I believed them, but it does hurt. It’s hard to explain, but it was weird and painful.
Surgery
What was the mastectomy like?
After the AC chemo, I had a scan. They knew then and there that it hadn’t shrunk enough to have just a lumpectomy. My surgeon suggested a mastectomy at that point.
I had scheduled the mastectomy. Then, 3 weeks before that, I decided to go ahead with the bilateral mastectomy.
Mastectomy surgery recovery
I was nervous. The only surgery I’d had before was a C-section. I was most nervous about the pain I was going to experience after.
I wasn’t really nervous about losing my breasts so much. They were killing me. I wanted them gone.
I remember the anesthesia hurting. The needle was painful. I don’t remember much of waking up, but I know I wasn’t in pain.
They told my husband that everything went well, and he told me because I was out of it for a while after I woke up.
It was a day surgery. I came home and put my husband’s shirt on. I had bandages around me. Someone had told me not to look when the bandages came off. I was so numb that I wasn’t in any pain.
About 2 weeks later, I had some weird tingling in my nerves around my elbows, but that was it.
I’m squeamish with blood and scars, so when I looked, it was kinda ugly looking, but losing my breasts didn’t really bother me. I wasn’t as traumatized as I know other women have been.
I had the mastectomy at the end of January, and I had radiation in the beginning of April, so I had a nice break.
Radiation and more chemo
I had 25 sessions of radiation. I went every weekday for 5 weeks. Radiation took a while, and then I was just tired.
I had started Herceptin while I was on Taxol, and I continued that. I got that infused every 3 weeks. I stopped for a little bit when I had my surgery. I had 18 infusions in total.

Relapse
Remission to relapse
At my first visit after the surgery, I got the official NED declaration. I was done with treatment on December 31, 2018. When I was told I was NED, I didn’t know if I fully bought into that.
It was really hard to get back to my normal life after that. It felt like nobody really understood me and my emotions. Just because I was NED didn’t mean I wasn’t worried a lot.
When my Herceptin was done, I was having some pains in my chest. I was going to the ER sometimes. It ended up being nothing. They said it was anxiety.
Then 2 months later, I started getting headaches. I thought I was going insane. Turns out, my headaches were something.
How did you find out your cancer was metastatic?
I had headaches constantly for about a month. I was going away on vacation, and I went knowing that I very well could be in metastatic relapse. I just wanted to enjoy myself.
When I got back, I got really dizzy. I called my doctor and went to the after-hours clinic and wasn’t going to be able to get an appointment for about a month.
I worked the system and went to a different hospital in a different town. I presented myself with constant headaches. The doctor saw me and ordered a CT scan. Then he came in and told me.
I think I already knew before I found out. My twin sister, daughter, and mom were there with me.
It wasn’t until I told my son that I started crying. After that, I was a mess for 2 weeks straight.
Treatment plan for the brain mets
I had to get radiation. It was inoperable, so we went the radiation route. I had the mask and everything, but it didn’t scare me.
I must be nuts because I actually thought the mask was kind of nice.
I just thought of it as a spa mask they were putting on my face. It was cool and felt good.
I had 5 treatments. The treatment itself took 5 minutes. It was only 10 to 15 minutes total. It just made me tired. I lost my hair in certain spots.
Then I went on Taxol again. I ended up in the hospital from that for 7 days. One of my sons was sick, and I got it. I didn’t have enough of an immune system to fight it off.
That was a downward spiral. That was a horrible experience. They couldn’t figure out what was wrong. I just kept saying, “My son had a bad cold. I have it, too, and have it worse.”
I did Herceptin and Perjeta after that. I had some bad diarrhea from that, but I was okay. My oncologist was nervous about those drugs, though, because they don’t get through the blood-brain barrier, so he put me on Kadcyla. That’s what I’m currently on.
It’s an infusion I get once every 3 weeks. I’ll be doing this until it stops working. I had some bad neuropathy from it, so I paused for a few months, but I’m back on it. I get extreme fatigue from it, too. My nose drips sometimes, but it’s not constant. That’s pretty much it.
What’s your status now?
I get scans every 2 months. I was stable in December 2019. I was fairly stable in the beginning of March 2020.
There was this one spot, but they’re not worried about it. They think it’s from radiation because it’s still in the tumor area.
Reflections
How are you coping mentally and emotionally?
I went and saw a counselor at the cancer clinic. She helped me process things a lot. I have a palliative care doctor as well who helps me process things. I have Facebook support groups.
I faced my mortality, and it just gets easier to face it.
What is it like to live with cancer as a chronic illness?
I’m really optimistic. I’m quite a positive person. Either that or it’s denial, but I’m just really a positive person. I guess I just have a lot of faith in science.
It helps that I know I still have another great treatment option lined up if this one stops working.
Who knows how much time these treatments might buy me and what we might know then? I have thought about dying.
The hardest part is my children and leaving them, but I’ve done things to prepare. I’ve written them emails just in case. I get angry about it sometimes, but then I think positively a lot.
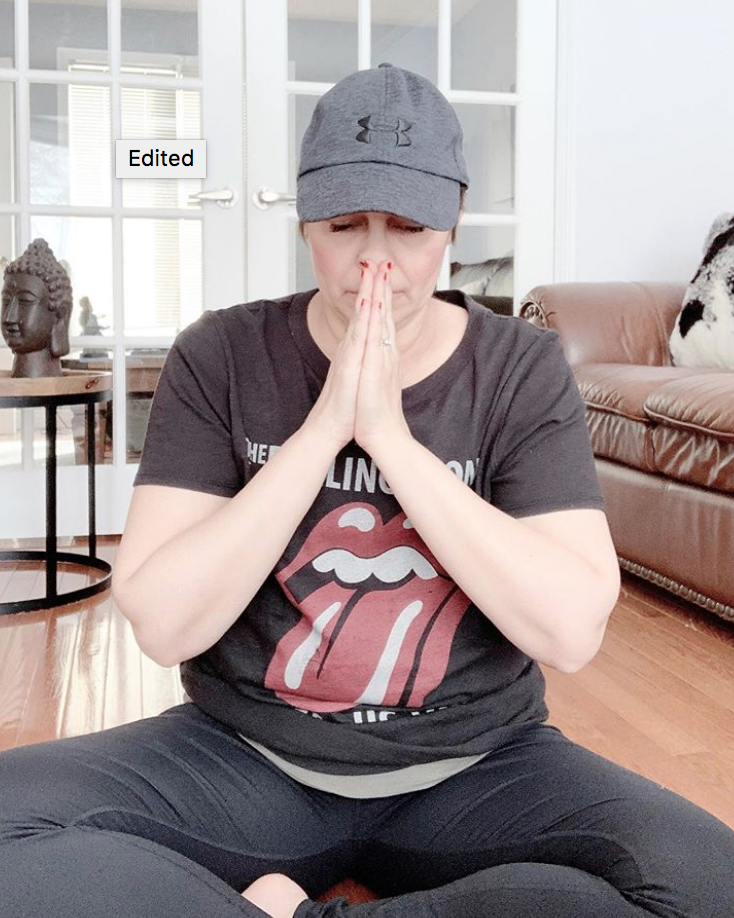
I’ve done some meditation and classes to learn to deal with stress and anxiety. It’s a daily thing.
Your support system
My husband has been very helpful. He’s taken up a lot of the housework, cooking, and all that. My kids have helped. Maybe not as much as I’d like, but they’ve helped. They’re all teenagers.
I have a twin sister, and she’s amazing. I don’t know how I could’ve gotten through this without her. I also have another sister who is very supportive as well.
We talk every day. What I like about my twin is we talk about normal stuff. We talk about what we’d like to do this summer and shopping, and we make future plans. We talk about the everyday.
My mom comes to all my chemo treatments with me. I love that time with my mom.
Others have offered to come, but I don’t want them to because that’s my time with my mom. I like how she looks after me.
I’ve had some great friends look after me. I’ve lost some friends who’ve distanced themselves. I’ve had some great new friends who have stepped up, too.
We’re a hockey family, so we get a lot of support from other families. We live in the suburbs outside a big city, so a lot of neighborhood families have helped out with meals and things.
»MORE: What kind of support cancer patients say helped the most
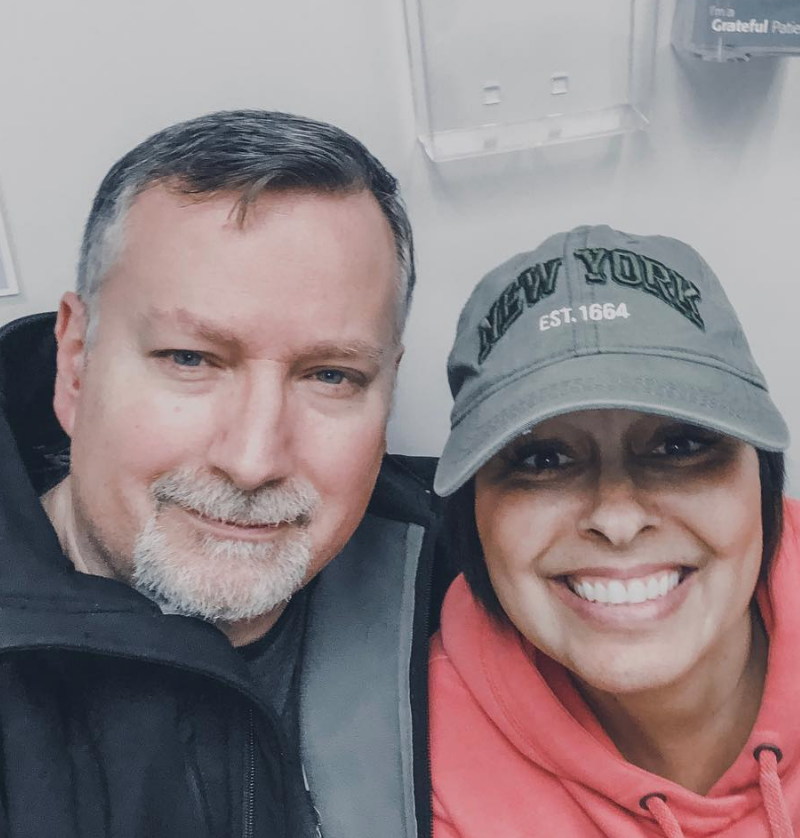
Cancer’s impact on your relationship with your husband
It’s so hard. We had just gotten married. Then 2 months later, I was diagnosed. Before that, we were together for 3 or 4 years.
I felt supported, but there was a lot of tension in the house. Then, when the stage 4 diagnosis came along, we really connected. It was like nothing else mattered. We realized what was important.
A lot of the lack of communication was me. It took me going to a counselor to find ways to express how I was feeling. I didn’t understand his side of things.
I was like, ‘I’m the one with cancer,’ but then I realized that it was scary for him, too.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
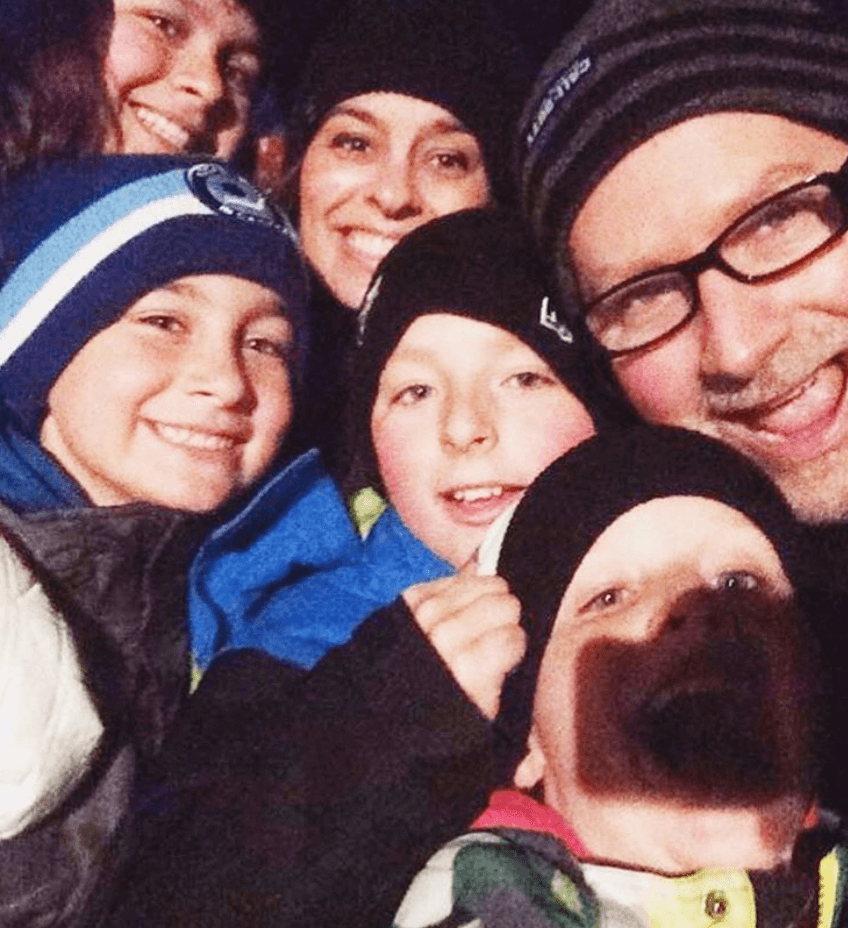
How did cancer affect you as a mom?
I felt like I failed them. Not because I felt like it was my fault that I got sick, but because I couldn’t do all the things I wanted to do for them that I normally could do. I felt tired and weak, and then I felt like a failure.
In happy moments, I’d be happy for them and then be so tired. In struggles, I wasn’t as available to them. I felt like they stopped telling me as much.
»MORE: Parents describe how they handled cancer with their kids
What advice do you have for someone who has just been diagnosed?
Take it one day at a time. I know they say that, but it’s so true. You are going to be so overwhelmed. I joined Facebook groups at first and had to unfollow them.
There is so much advice out there. You have to decide what’s best for you.
If you have a good oncologist, trust in them, but also be your own advocate. If you’re going to do your own research, make sure it’s not Dr. Google research. You’ll learn through the experience.
Try to see the positive. Maybe it won’t be every day, but find it. I’m not saying, “I’m so glad I had cancer.” I’m not. Practice gratitude, though, because having a negative attitude is not going to help you.

Inspired by Renee's story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation





















2 replies on “Renee’s Stage 3-4 Relapsed IDC, HER2+, Metastatic Breast Cancer Story”
Renee was the most beautiful woman in the world.
She was someone who inspired all those that knew her.
She was my everything.
Mike, I am so sorry to hear of Renee’s passing. Her story will live on and continue to help so many people who are looking for the support that Renee gave. My condolences.