Rachel’s Stage 1B IDC Breast Cancer Story
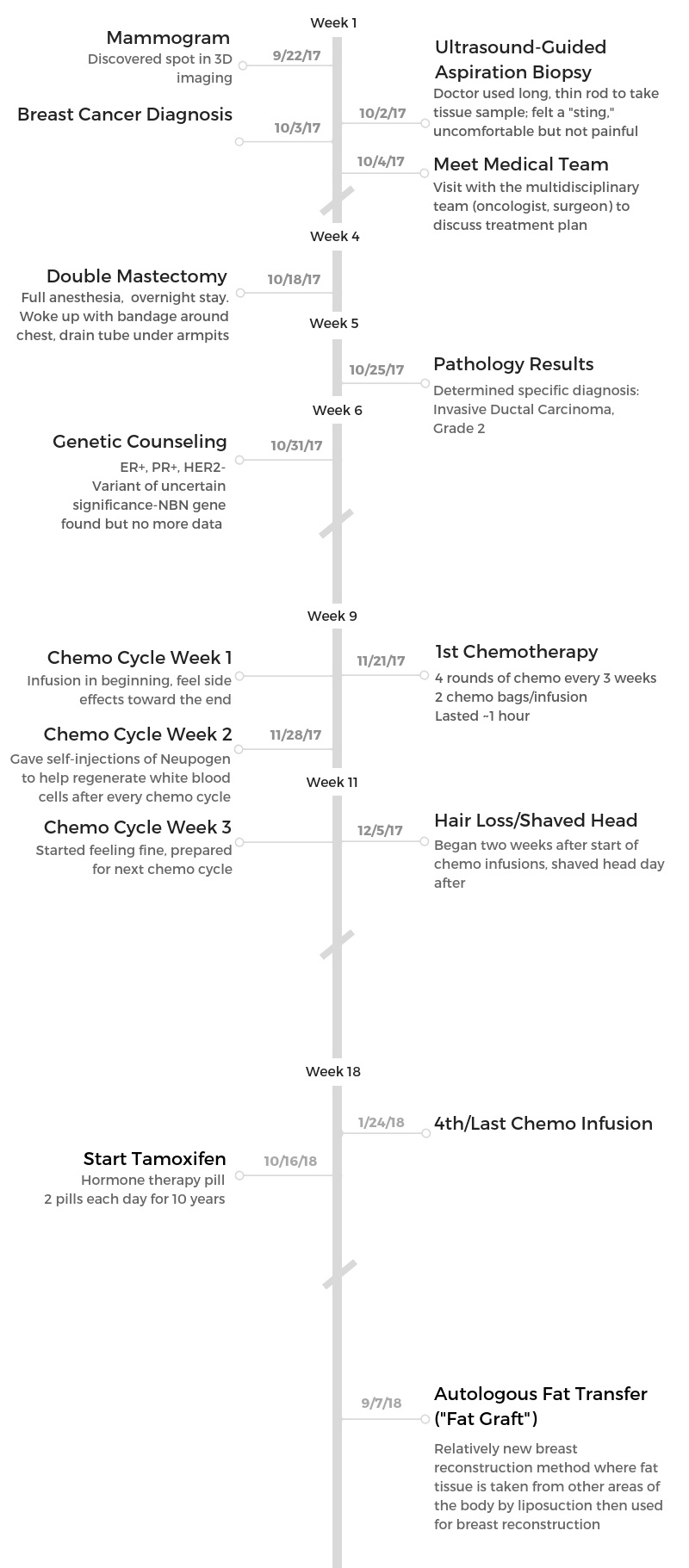
Rachel shares her stage 1B breast cancer story, one that started after a delayed mammogram showed a lump. She describes undergoing a double mastectomy, chemotherapy, and hormone therapy.
In her story, Rachel highlights how she managed through the hair loss, the importance of self-advocacy for patients, and the transition to survivorship.

- Name: Rachel Y.
- Diagnosis:
- Breast cancer
- Invasive ductal carcinoma (IDC)
- Right breast
- Staging: 1B
- 1st Symptoms:
- No symptoms
- Delayed mammogram showed lump
- Treatment:
- Double mastectomy
- Removing all breast tissue
- Chemotherapy: AC-T for 6 weeks
- AC (Adriamycin + cyclophosphamide/Cytoxan): 4 weeks
- T (Taxol): 2 weeks (cut 2 weeks early)
- Hormone therapy for 10 years
- Double mastectomy
This is who we are. Cancer cannot define us. Our mastectomies and the bald heads can’t define us.
The cancer wants to try to beat us, but we can beat it back.
Rachel Y.
- Diagnosis & Tests
- First symptoms
- Getting diagnosed
- Describe the ultrasound you underwent before diagnosis
- Describe the biopsy after the scan
- Waiting for results
- How did you get the specific diagnosis?
- How did you break the news to loved ones?
- Did you get a second opinion?
- How did you decide where to get treatment?
- What did you like about going to your larger-size hospital?
- Did you undergo genetic testing?
- Mastectomy & Recovery
- Chemotherapy & Side Effects
- Hormone Therapy
- Hair Loss
- Quality of Life
- What got you through the toughest times?
- What’s your advice to others on how to deal with the stress?
- Were there moments you had to advocate for yourself in and out of treatment?
- Describe the transition to survivorship
- What’s your advice to others on how to get support?
- What got you through the toughest times?
- Were you able to work through treatment?
- Did you get any financial assistance?
- Message to other patients
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Diagnosis & Tests
First symptoms
I had no symptoms. I went in for a routine mammogram. What was kind of odd about this mammogram is I had put it off for 6 months.
I had a reminder on my bulletin board, and every day I walked past the bulletin board and out my door like, “Oh, I have to call.”
I put it off for 6 months, and then as I was walking out my apartment door, I get a call from the imaging department.
They’re like, “Hey, we noticed you’re past due on your mammogram. We’d like to make an appointment for you.” Since I’m on the line with them, I made the appointment.
A week later, I go in for my appointment, not thinking of anything because I’m in shape. I had no symptoms.
It was just routine — until I got a call from my doctor saying that they found a lump or a mass.

Getting diagnosed
It was the mammogram, and I was scanned with that 3D imaging. Through the imagery, they found a spot. It was maybe like a quarter-sized spot that they seen.
Just for precautionary measures, my doctor ordered an ultrasound. Then during the ultrasound, it was verified that what they saw on the mammogram was actually in concurrence with what they saw.
Those were already 2 verifications, but just to make sure if it was benign or cancerous, they ordered the biopsy.
At this point, I’m a little freaked out because this has never happened to me before.
I think the biopsy took 2 days, and then I got a call from my doctor.
She said, ‘Are you in a good place to talk?’
I said, ‘Yeah.’
She said, ‘I have bad news. You have cancer.’
I think at that time, I was just so shocked. I didn’t even know. I had no emotions. I think I’m still not really processing everything yet. It was just kind of devastating.
Everything progressed really fast after that — from one minute being diagnosed to the next minute having a mastectomy, followed by chemotherapy.
Describe the ultrasound you underwent before diagnosis
The technician just scans your breast, and they’re able to look on the monitor to see if there’s any hollow spaces or dark spaces.
If the breast is gray, the tissue is gray. If there’s a black spot, that’s an indication of a mass, whether it’s benign or cancerous.
She just scans over the breast and is able to take a picture of all the different sides.
The ultrasound probably took about 15 to 20 minutes, because the technician was really took her time. She was really going over each area, dissecting from one quadrant to another. At the same time, she was taking pictures.
Whatever area that she stopped at, she would take a picture, and then she would just make sure that she had the best pictures for the doctor to be able to look at the scan and determine if it was indeed what they suspected.
Describe the biopsy after the scan
The biopsy is a little bit different. I really didn’t know what to expect. The doctor has a long rod, but it’s really thin. It’s almost like a plunger.
All I felt was a sting. It was very uncomfortable. What the doctor does is taking out that tissue, right in the office.
You don’t have to go under any anesthesia. It’s just a poke. Definitely uncomfortable, but nothing to be afraid of.
I think more of the fear is what are they going to find out? The biopsy was really quick. Probably the same thing, about 15 minutes. The doctor took 2 samples of the tissue. Pretty easy.
Waiting for results
I waited less than a week, but it was very agonizing because you want to know now.
Living in Hawaii, everything has to be sent to a mainland lab. I think that was what was painful.
During that week, I tried to not think about it. I kind of kept my mind occupied with other things. By the time I forgot about it is when my doctor called with the results.
»MORE: Dealing with scanxiety and waiting for results

How did you get the specific diagnosis?
My primary doctor told me that I had breast cancer. The following day, I had an appointment to see the cancer care team.
It’s in a multi-disciplinary clinic, and they had 5 doctors that came in to talk to me.
One was my oncologist, who was the one who told me that I had female breast infiltrating ductal carcinoma on my right breast.
The oncologist told me about type. Then the plastic surgeon came in to tell me I could either opt for a lumpectomy or a mastectomy.
They had a radiologist and the nurses. It was pretty intimidating in the sense that all this information is being thrown at you.
They were very caring. It happened on the same day. What has happened in the past is cancer patients would have to go from one appointment to another.
I don’t know if it’s like this everywhere, but Kaiser decided to bring all the doctors to the patients.
I sat in a room. One after another doctor came in to me, then the next one would come in to see. They just were very passionate, very kind. In a sense, I’ve never been treated that way going to my regular accounts.
I think I’m still in disbelief, still in shock. But the only thing that brings me back into reality is when I look at my scars every day, when I’m getting ready, when I’m looking in the mirror.
How did you break the news to loved ones?
I had started a new [work] position. Right before my start, I had a colleague [whose] wife was going through cancer at the same time.
I told him, “I think I may need to talk to your wife.” He said, “Oh, nah, nah. It’ll be okay. You’ll be fine.” Then once I found out about the cancer, I told him, “I need to talk to your wife.”
He was devastated. She was devastated. She actually came with me to my appointments, because I’m single. I went through this journey — really, when I look back at it — alone.
I broke it to my friends. I think the hard part is, what do people say?
They’re too afraid to say anything, or they say the wrong thing.
»MORE: Breaking the news of a diagnosis to loved ones
Did you get a second opinion?
No, because I trust my doctors, and it would cost money for me to get a second opinion. [The diagnosis] was pretty straightforward.
Again, I’m glad they caught it when they did. I think for me to get a second opinion, it would just prolong my agony.
How did you decide where to get treatment?
I was always at Kaiser, and I decided to stay there. For me to have to change, it’s just such a hassle, and it would end up costing me way more financially.
What did you like about going to your larger-size hospital?
I have to say that I had a great cancer care team. I think the problem is there’s either not enough chairs or too many cancer patients, so they’re always busy.
Other women going through the same thing at other local hospitals [said] it’s the same. There’s either too many cancer patients, or you could have more chairs and still be out of room.
I think for Kaiser at least, they do their best. They’re just very kind-hearted to people. I’ve never had a problem.
Did you undergo genetic testing?
Yes. I did the genetic testing. They did find something, but it was inconclusive.
Mastectomy & Recovery
Choosing a double mastectomy
I decided to do a double mastectomy, even though the cancer is on the right side.
The reason why I chose both is because I think I would be more devastated looking into the mirror and seeing one breast.
Also, I don’t want chances of cancer coming back in my left breast and the doctor saying, “Hey, you have cancer.”
Describe the double mastectomy surgery
No prep work. The only thing they did is scheduled my appointment, then I just went in and had the surgery. It was pretty upfront. Full anesthesia.
I think it took the whole day, and then I stayed a night. They wanted to keep me overnight. I think that’s pretty common.
I remember waking up and having a bandage around my chest with 2 tubes, one on each side below my armpits.
They’re called drain tubes. It wasn’t that I was sore. I think I was just numb. It didn’t really hit me until I took all the bandages off probably 3 weeks after.
I don’t know how I reacted. Shocked. I think I’m still in shock, like I said, but it’s the reality. My breasts are gone.
My doctor was pretty upfront that this is what’s going to happen. She left enough skin so when they do have my reconstruction surgery, she said it won’t be a problem.

Did you feel any side effects from the surgery?
Not overnight. I think I was a little sore, having to ask for more medications. Most of it was because they require you to blow out of this breathing tube.
So anytime you inhale or exhale, I do remember I was a little sore. [It lasted] probably two days.
Describe the drain tubes post-surgery
It didn’t last very long. What I had to do every day for about a week is empty my drain tubes. They require you to empty the drain tubes and then record how much fluid comes out.
Then when I was about to start showering 4 days after the surgery, one of my tubes came out. Of course, I’m freaking out. I called the doctor’s office and said, “I don’t know what happened, but the tubes have fallen out.”
They’re like, “Ah, don’t worry about it. It’s okay.” It’s supposed to stay in for a good week.
The tubes are really long, and you [need to] pin them up. I’ve noticed just looking at websites, women make these little aprons to put the little tubes in.
Women have made these aprons for the next women in line that have to go through this. Otherwise, those tubes are hanging down, and I didn’t know any better.
I let them just hang by my side, and I think one of them just got a little too loose.
Have you had reconstructive surgery?
I have not. The reason why is because I’ve had a few other surgeries since then. I don’t want to start the reconstruction until my other surgeries are done with.
I’ve had various injuries before cancer and before chemo. Right after chemo, it just did something.
It just made my bones really weak, and it has exasperated a lot of my old injuries. I’ve had 2 shoulder surgeries. I’ve had a back surgery.
»MORE: Read more patient experiences with surgery

Chemotherapy & Side Effects
How long after surgery did you start chemotherapy?
I started a month after. They had to give me time to heal from the surgeries.
Describe the chemotherapy regimen
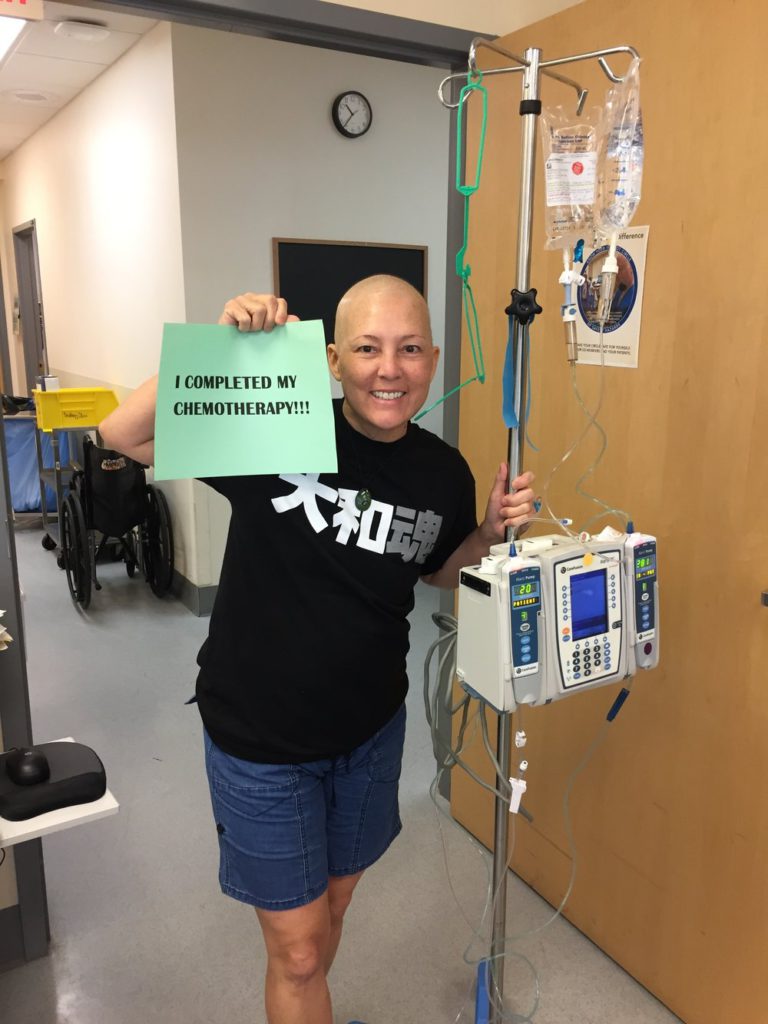
[The infusion] lasted like an hour, hour and a half. I had 2 [chemo] bags.
I had 4 rounds of chemo, and it’s every 3 weeks. The first week, I have chemo.
Towards the end of the week, I started feeling kind of ill. The second week, I had to give myself injections (Neupogen).
I was really in a lot of pain, like muscle ache and joint ache. It just helped regenerate the white blood cells. Then the third week, I was fine. Then it would start all over again.
Can you describe the chemo side effects?
- Foggy mind
- Stomach pains
- Feverish
- Body aches
- Taste changes
- Slight nausea
I just felt real cloudy. My mind was real cloudy. I just felt like my body was hallucinating. I don’t know if you can understand that. Then just sometimes feverish and just the body aches.
Then my taste changed. I had certain cravings, wanted to eat, but then I didn’t want to eat. It was just very frustrating.
I had nausea. It wasn’t as bad as some people’s. I think I had more stomach pain and stomach issues than anything. Stomach pain instead of a nauseating feeling.
Did anything help prevent or reduce the side effects?
Sometimes the medicine. They had me on oxycodone. That helped a little bit. Not sodas, but drinks that were fizzy.
I tried to eat because I didn’t want to get weak or sick, but it’s just different how the body reacts.
I remember one week I had cravings for chocolate donuts and French fries, and I never eat that stuff. Then when I start eating it, it’s like it doesn’t taste. It’s bland.
Any advice to others on what can help with side effects?
Keep ginger chews handy. Just try to eat what you can, whatever it is, just whatever you can hold down.
Part of the problem is if you don’t eat, then you get sick, and then you can’t do your next treatment.
Were there follow-up scans after the surgery and chemo?
I didn’t do any scans after. What happened is just office visits with my oncologist. They felt that they had taken all of the cancer via the mastectomy.
Hormone Therapy
Describe tamoxifen, the hormone therapy
My oncologist just said most women do really well on tamoxifen, which I thought was for 5 years. But for me, it’s 10 years. He said that women have a greater chance for the cancer not coming back.
However, there is that side effect of cervical cancer, and then he named a few other side effects — weight gain, early menopause. That’s it. He didn’t really say too much more.
It’s a pill. Every day I take 2 tablets, and I hope the cancer doesn’t come back. [I take it for] 10 years.
Are there day-to-day side effects to the hormone therapy?
Joint muscle pain. It seems like I’ve already gone through menopause, and then weight gain. I have not been able to lose weight.
My doctor mentioned to me to try 2 weeks of getting off of tamoxifen or stopping tamoxifen to see if it helps, but it didn’t.
Any advice to others who are about to go on hormone therapy?
Just be prepared. If weight gain is an issue, prepare to maybe change the lifestyle [and do] more healthy eating, whether it be plant-based, vegetarian, or whatever it is that you can do to not gain weight.
For the joint and muscle pain, I don’t know, because I’m dealing with it now. No matter how much I have to tell my doctors, there still isn’t a solution yet. I know some women do CBD.
For me, I can’t because I’m subjected to random urinalysis, so I can’t do it. I guess whatever works for them. My doctor recently recommended that I try red light therapy. I’ve done 2 sessions, and I can’t really tell you if it works or not.
»MORE: Read more patient stories of hormone therapy
Hair Loss
Describe the hair loss
I have pretty long hair. I have a lot of head shots because I’m a background actor, so my hair was my identity. Then I was told, “14 days after chemo, you will lose your hair.”
It was exactly 14 days. I was washing my hair, and it didn’t come out in clumps in the shower. It was when I brushed my hair, just clumps of it came out.
That was on a Sunday. I had to go to work on Monday, so I called my friend. She was going through chemo at the time, and I asked her if she could come over and shave my head.
I didn’t want it to happen, but I didn’t want to go to work with just patches of hair.
I think I’d be more devastated if my hair started falling out at work. She came over, and she shaved my head. It was different, but I think what really hit me is when I lost it all.
She had shaved it short. Then, I think it was like a few weeks later, it was in patches. I had to get it shaved — like shiny, bald head.
»MORE: Patients describe dealing with hair loss during cancer treatment
What was the hardest part about the hair loss?
It changed my look, and I felt like people were looking at me or staring at me. I felt really vulnerable.
Then having to go to work, I wore a baseball cap for the most part. Then I’m at work, and my head is just burning up wearing this hat. Then I take the hat off. It was a vulnerable feeling.

What helped with the hair loss?
I think some of my colleagues just kept encouraging me, saying that, “You look good. You have a nice-looking shape for your head.”
Sometimes I would go without my hat. I think, in a sense, of me being vulnerable, I still wanted to please others.
Did it feel good to go out without covering your head?
It felt good. I’m free.
I think it’s just funny how people are because after my mastectomy, no breasts, I would catch people looking at my chest.
That was before all my hair came out, and then my hair came out and the same thing. I think then they would put 2 and 2 together, and then others were like, “Oh, nice haircut.”
Any advice for others on how to manage the hair loss?
Just embrace it. The new you. Know that it comes back, and it’ll come back curly.
People that know me, they’re really shocked. Others are like, “Oh, nice haircut. Oh, nice perm.”
I said, “No, this is my chemo curls.” Like I would get a perm this short!
Embrace it. You will feel awkward, embarrassed, but that’s you. It’s a sign of what the cancer and the chemo has done, but be proud.
You’re alive. Know that the hair will grow back. It’ll grow back healthy and curly.
I think, just for women, we need to be more, “This is who we are. Cancer cannot define us.
Our mastectomies and the bald heads can’t define us. The cancer wants to try to beat us, but we can beat it back.
Quality of Life
What got you through the toughest times?
Everything happened so quickly, and then I started a new work position right when I found out that I had breast cancer.
There was the stress of my boss, who was very unsympathetic. I don’t even know how to describe it, but just some of the things that she would say.
Do you understand I’m going through chemo right now? I was just numb. I think it’s bad, because I’m sure it’s going to hit me.
What’s your advice to others on how to deal with the stress?
Just find somebody who understands, who really understands, whether it’s a group.
I would’ve been involved with a group like this or any other cancer group with women that have been through that circumstance. Friends and family may say what they say because they don’t know how else to say it, but they don’t know what you’re going through.
I would just suggest to get a good support group, have one that understands, and a better-understanding person or women that have already been through this.
I’m more sympathetic, and I can understand. When I see somebody’s hair’s coming back or they’re bald and wearing a cap, I can reach out to them or say something to them because I know exactly what they’re going through.
Were there moments you had to advocate for yourself in and out of treatment?
No. I feel like I’m having to speak up for myself now, which is pretty odd, with some of the side effects that I’m experiencing.
It’s really hard. I remember talking to my oncologist — great guy. He took time out in the lobby to talk to me, and he answered every question that I had.
He gets it, but it just seems like because what I’m feeling with my side effects, that’s really not his lane. It’s now pushed over to another doctor in their lane, and they don’t get it.
They don’t understand my side effects and what I’m going through. I just don’t know really what to do anymore.
»MORE: How to be a self-advocate as a patient
Describe the transition to survivorship
There are some people that I’ve noticed, mainly people at work, they say that my hair’s growing back, so you’re fine.
But they don’t understand that I still feel a certain way, I get tired during the day, or maybe I can’t think clearly.
I think it’s great that the hair grows back, but at the same time, it’s like a person forgets that you just went through a life-altering experience.
What’s your advice to others on how to get support?
Everybody has different circles, but I also feel that it’s important to get involved in a cancer group because I can be honest and open with somebody who’s been through cancer. They know exactly what I’m going through.
We can help each other on that. My issue may be different than yours, but it’s the same, whereas if I talk to somebody at my work, they can agree but don’t really understand.
»MORE: What kind of support cancer patients say helped the most

What got you through the toughest times?
It was difficult because when you have faith in God, to get something like, it’s almost like, “Why, God, did you put me through this?”
At the same time, I think without that faith in God, I don’t know really where else I would be.
It’s only my only hope that I have to hope. Just spending time to be alone and just to rest.
Were you able to work through treatment?
I had to take a break in my second week, so the first week after chemo I worked. Then the second week when I was administering my shots, I had to take a break because I started getting really sick, and other people in my office were always sick.
I ended up going to the emergency room a few times with a high fever.
If I had to do this all over again, I probably would’ve taken more than just a week off, but at the time, my circumstances were a little bit different because I just started a new position.
It was temporary, but I was also competing for it. I felt like I had to be there, otherwise I wouldn’t have gotten this permanent job.
»MORE: Working during cancer treatment
Did you get any financial assistance?
No. I am very fortunate because I have insurance. I was able to get medical financial assistance. Then I had used all my leave, all my sick leave, all my annual leave, but my employer has a voluntary leave.
What other members have done is they’ve donated hours and hours of sick leave to me so I could stay home on sick leave and still get paid.
Without that, I don’t know what I would do.
Message to other patients
When I say to try to find somebody that you can rely on, I’ve tried that, and it’s a little bit difficult.
If you can’t find a person or if you don’t have people around you, then just go to a support group, cancer group, care group to walk you through it.
Then just find that person that can stand by your side and that understands. It’s the compassion, because that’s what a person needs when they’re going through this terrible disease.

Inspired by Rachel's story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation