Rach’s Stage 2 IDC Triple-Positive Breast Cancer Story
Rach shares her stage 2 triple-positive breast cancer story and how she got through treatment: chemotherapy, hormone therapy, targeted therapy, double mastectomy, and reconstruction surgery.
In her story, Rach also highlights the process of going through fertility preservation, the importance of self-advocacy for patients, and dealing with financial toxicity in paying for treatment. She gives some guidance on how to navigate the impact of a cancer diagnosis on relationships.

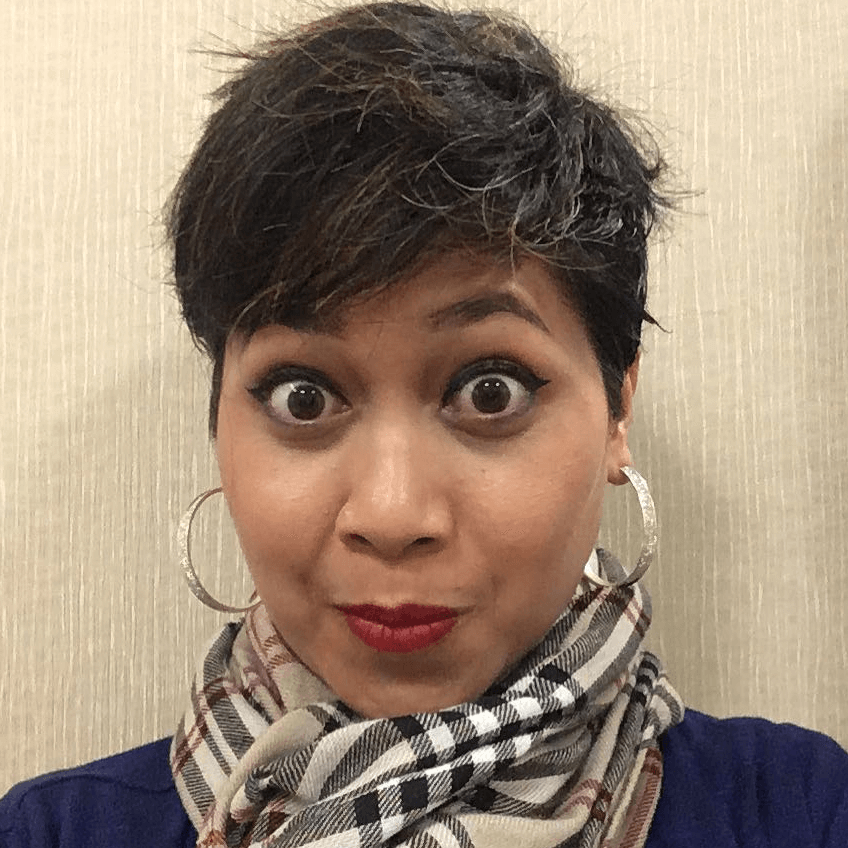
- Name: Rach D.
- Diagnosis:
- Breast cancer
- Triple positive
- Staging:
- 2
- 1st Symptoms:
- Mass on right breast
- Treatment:
- Chemotherapy
- Hormone therapy:
- Zoladex (goserelin)
- Targeted therapy
- Herceptin
- Surgery
- Double mastectomy
- Reconstruction
- Other drugs:
- Zometa
- IVF (fertility preservation)
- Diagnosis
- Describe your first symptoms
- Describe your diagnosis process (medical visits, tests, etc.)
- Describe the breast ultrasound
- Biopsy confirms cancer
- How did you process the diagnosis?
- How did you tell your loved ones the news?
- Did you get a second opinion?
- How did you decide where to get treatment?
- Neoadjuvant chemotherapy
- Fertility Preservation
- Chemotherapy and Side Effects
- Targeted Therapy
- Double Mastectomy Surgery
- Quality of Life
- Were there any surprises during your treatment process?
- Were you surprised by your hair loss?
- What was the worst thing you experienced?
- What got you through the tough times?
- Were there any moments you had to advocate for yourself?
- How important is it to have caregivers?
- How did cancer affect your relationship with your husband?
- Any advice for cancer patients on how to deal with a spouse during treatment?
- How did you deal with the financial aspects of treatment?
- Did you have any help preparing for outside of treatments (insurance, family cooking, etc.)?
- Was there anything you wish you had known?
- Survivorship
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Diagnosis
Describe your first symptoms
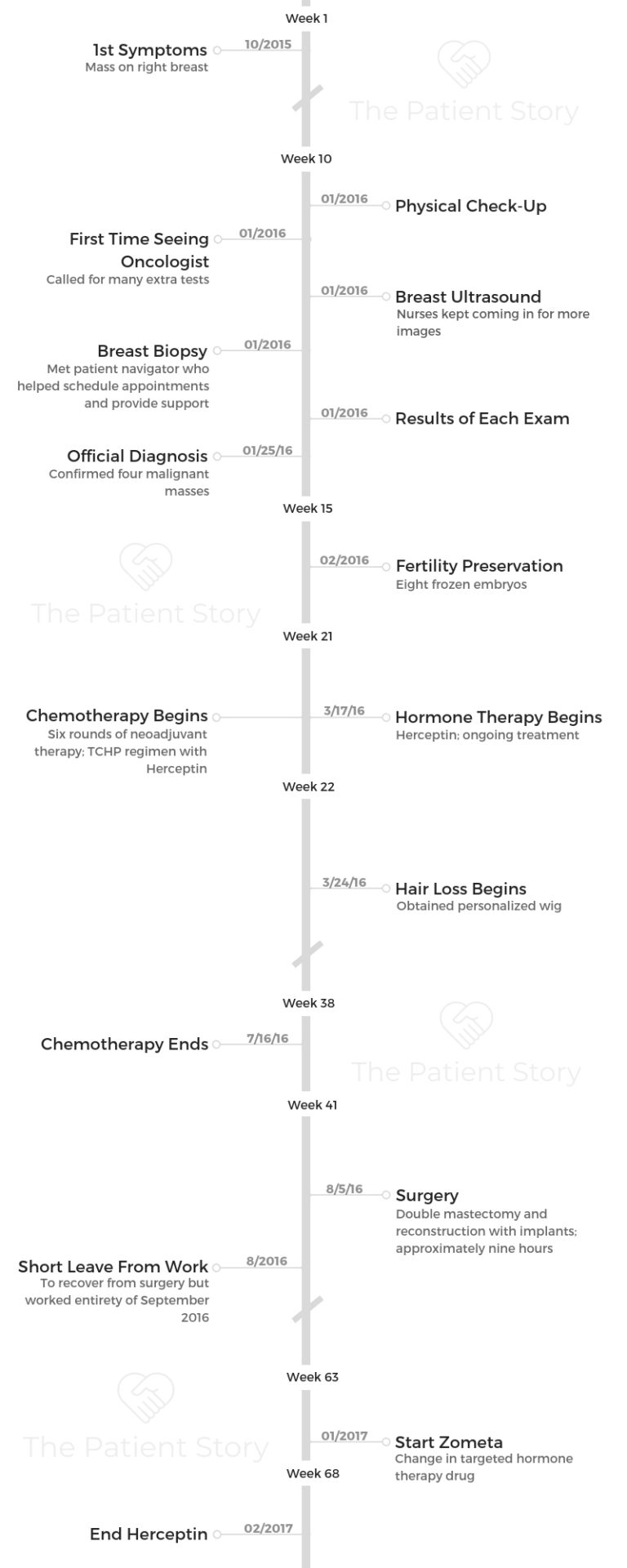
It was a little bit of a process. I think it really started during my honeymoon. I had my honeymoon in October.
We were in the Greek Islands, pretty much enjoying life. One of the days, we were like, “Oh let’s just hang out by the sun.” I was putting on my swimsuit top, and it’s one of those that were clasped in the front.
As I was attempting to put my swimsuit top on, that’s when my right hand just brushed over my right breast, and I felt something there.
The thing is, growing up I’ve always had this tiny lump, what I hear is common with other girls. It really wasn’t deemed as anything, and it probably wasn’t anything.
But I will admit, I rarely did any self breast exam because I just didn’t see the point.
The only time I would have it was when I would go see my doctor every year for my annual exam. As I brushed my right breast, I was like, “Okay, I’m kind of confused because I don’t know if it always felt this way, or it actually feels bigger.”
When I was explaining this to my husband, I seriously was about to faint. Part of me felt like something was wrong.
Of course, by the time we got back from our honeymoon, I forgot about it. The truth is I didn’t think anything could really be wrong with me.
Describe your diagnosis process (medical visits, tests, etc.)
The beginning of January, I actually had my physical exam that I was scheduled to have with my primary doctor. During my time there, she asked me when she was doing the breast exam, “Did that feel different?”
I was like, “Actually, I was hoping you can tell me. Because I can’t tell. Maybe? But I’m not sure.”
At that time, she said it does feel different. “It feels like you have 3 masses in there, but it could be fibroadenoma.”
She’s said, “You’re 27. At that age, women start to develop fibroadenoma. But just to be sure this is fibroadenoma, let me just schedule you a breast ultrasound.” She scheduled that immediately.
Describe the breast ultrasound
I did the whole breast ultrasound. I thought it was weird because the technician would continuously come back into the room and then tell me she needed more images.
Each time she thought she was done, she comes back saying, “Oh, we need more.” This literally took the whole day.
As I was getting dressed, they told me, “Oh wait, don’t dress yet. We need some more images.”
It just so happened I had my first-ever mammogram, and I was so confused.
Biopsy confirms cancer
As soon as I got home from the hospital, I got a call from my primary doctor. The next thing I know, I got my biopsy scheduled.
When I finished it, there was a patient navigator in there with me. My primary physician actually called me during her vacation, and she’s like, “I’m sorry I have to call you.”
She pretty much confirmed that I had 4 masses that were malignant, basically 4 cancerous tumors, and confirmed with me that I have breast cancer.
Luckily, for some reason deep down inside of me, I also felt like I should work from home that day, and I’m very glad I did.
Hearing you have cancer while you’re in the middle of working, you’re just like, ‘Wait, I just finished one of the most important meetings, and now I’m being told I have cancer? This is bizarre.’
But at the same time, it didn’t register. I heard her say I have cancer, and I immediately called my husband, my family, or anyone I was close to to tell them what the results were.
As I was saying it, it just didn’t feel real. As if it had to belong to someone else, not me.
Ultimately, that’s what led to my official cancer diagnosis. It was January 25th.
How did you process the diagnosis?
That’s the weird part. You know how your mind thinks there’s something wrong, but maybe not? I’m not quite sure exactly how to process what I was thinking.
You hear the word “cancer,” and you know it’s bad. You see it on TV, and you always feel bad whenever you hear that anyone has to go through cancer.
But you never ever think it actually will affect you.
It’s a weird feeling thinking, “Maybe there’s something wrong.” But at the same time, I kept telling myself, “There’s no way. This is a rare thing.”
»MORE: Patients share how they processed a cancer diagnosis
How did you tell your loved ones the news?
I immediately called my husband and said, “Hey, I just got the results.”
He’s like, “All right.” I think he knew. I think he probably could tell by my tone, my voice. I’m not sure, but he knew. He was like, “I’m heading home now.”
I called my parents and pretty much just told them, “I got my biopsy results, and they confirmed that it is breast cancer.”
At first my dad was confused, because he was like, “Are you sure that’s what you heard? Maybe you think…”
I was like, “No, I’m pretty sure that’s what she said, because she’s having me schedule to see an oncologist and a surgeon.”
My dad’s like, “Okay, well, I’m going to call your mom. I’m going to pick her up from work now, and we’ll come over there.”
I texted my best friend because she’s been asking me, and she kind of knew what was going on. Next thing I know, she didn’t really tell me she was coming over. She just came over.
I think it was harder for my in-laws — I’m also close with them — because they weren’t in town. They were in Florida.
They were being very optimistic the entire time because people who have abnormalities, usually it’s nothing.
It was also really hard to hear it is cancer. I let my husband handle it. They were very shaken by with the news, but there was no way to dance around the results.

Did you get a second opinion?
Yes. I wanted to take advantage of all the great hospitals that I live by, so I pretty much had 4 second opinions. I wanted to make sure, because I came from a family who has worked in the medical field.
I also understand the importance of being in the right care, and that also has to mean who I feel the most comfortable with. It’s a chemistry kind of thing.
If you have a good vibe about your doctor, I honestly believe it’s not going to be an easy process, but it’d be easier. I wanted to make sure that I found the right one for me.
How did you decide where to get treatment?
With my patient navigator, it was all regarding that one hospital. I was pretty vocal with every doctor I met at that first hospital.
I’m like, “I’m going to go seek a second opinion.” They also agreed. They were like, “You know, that’s good.”
Then I also worked with that hospital to make sure to start releasing some of the test results to all these different hospitals that I wanted to get a second opinion on.
I also asked a couple family members who are doctors about who they think would be best and to give recommendations.
My husband and I did a little bit of our own research. Some of our other family members who wanted to help us out in a way did their own research.
Ultimately, I came to a decision with which doctors I wanted to see in each hospital. I met with the main doctor I wanted to see and their team.
One thing I know is you may have a primary attending that will be your doctor. They’ll handle your standard of care.
But they always have a team. You have to make sure you feel comfortable with that team, too.
They’re the ones who are going to be checking up on you more often than the attending physician. I also wanted to hear what their treatment plan was.
What’s crazy was every hospital was slightly different, and I was glad I was able to see that. For me, it’s very important to go with a treatment plan that I feel most comfortable with and with the best outcome.
Neoadjuvant chemotherapy
My treatment plan was neoadjuvant chemotherapy. It is basically having chemotherapy prior to surgery.
Every doctor had a different opinion, but I went with a doctor who preferred neoadjuvant chemotherapy because they said that shows evidence and proof that the treatment is working.
If they’re seeing the tumor shrink, then they know whatever they’re doing is killing the cancer cells. They said in their eyes, if they remove the tumor first and then get treated, they are not sure if they’re giving me the right regimen. They’re kind of just killing it blindsided.

Fertility Preservation
Describe the process of fertility preservation
One thing I wanted to make sure before I started chemotherapy was that I did the fertility preservation, which is why there’s a gap between when I got diagnosed and when I started chemo.
I got diagnosed on January 25th, but I didn’t start chemo until March 17. In between, I was not only doing second opinions, but was also thinking about fertility preservation.
My husband and I knew we wanted to have a family. We didn’t plan on having a family soon after we got married because, at this point, we were only 6 months into our marriage.
A lot of the doctors did say, “If you want to have a family, that’s something you have to consider.”
With treatment, things can change. Your reproductive system can change, and it may not be a guarantee that I can naturally conceive a baby.
She had me meet patients who naturally had a baby without going through any IVF process, but also had me meet some of her patients who went through the fertility preservation.
She said, “I want you to know you have options, and I will support whatever decision you make.”
There’s a fertility specialist that deals with cancer patients, and she said, “I’m going to talk to him and make sure every medication that he is providing you is something I feel comfortable with. No matter what happens, my team is ready to manage whatever it is.”
How did fertility preservation affect you emotionally
It was a very hard decision. Because it’s triple positive, it also means that my hormone receptors are what’s feeding my cancer.
I was afraid to first go through this fertility preservation process, because it does mean that they’re going to have to give me more hormones to speed up the whole fertility preservation process and make sure they retrieve everything they need in order for it to be successful.
One of my doctors told me, ‘I want to take care of you now. I want you to be alive, but I also want to make sure when you’re alive that you also have a good quality of life after.’
She told me, “If having a family’s important to you, even if you don’t see yourself having it right now, I really think this is the route that you should go. It doesn’t mean that you cannot naturally have a baby.”
I thought, “Okay, I like this. I like what she’s saying. I liked that she cares what my life would be like in the long run.”
I did the fertility preservation process, and it took about a week to retrieve my eggs. Then we also did the whole embryo process. I feel very fortunate to say that we have 8 frozen embryos.

Describe the IVF process
I think I was in what they call survival mode. I was like, “Okay, I just need to figure out what the next steps are.” I obviously knew cancer is bad, and it came to me that I have cancer. I was like, “You know what, I’m ready to fight this.”
I was like in more survival/fighter mode, but it was exhausting because I had a very intense day job. It was demanding just due to the nature of the work I do, so trying to juggle that and then going to doctor’s appointments — it’s mentally exhausting.
By the end of the day, you just literally don’t want to do anything.
There were times, though, I was really, really scared because you hear those things about cancer. Ultimately, I just wasn’t sure what the outcome would be.
I feel comfortable with the team I’ve selected, but I also know there’s only so much that could be done. I just really, really hoped that the route I chose was the best route to take.
»MORE: Read a patient’s detailed IVF journal
What was the next step after fertility preservation?
I did the neoadjuvant chemotherapy. At the same time, they started targeted therapy and part of my hormone therapy.
My regimen is TCHP, which included Herceptin, the targeted therapy. For my hormone therapy, they had me already started on the Zoladex shots.
They just wanted to make sure they were protecting my ovaries and said it was important for me to basically have a baby afterwards.
They wanted to suppress any hormones in my body. I went through 6 rounds of it. It definitely wasn’t easy.
Chemotherapy and Side Effects
Describe the chemotherapy
It was 6 rounds.
There were times where I couldn’t even do my next round of chemo because my blood counts were so low, and it had to be rescheduled.
That was very disappointing. I remember the first time that happened because I had this countdown. I’m like, “Okay, just finish round 1 or round 2, which means by the time I’m done with everything, I’ll be done on this day.”
When you can’t go in for your treatment, it just sucks because then you’re like, “Ugh, then that means my date gets pushed back when I’ll be done.”
There is a good thing, though. I say good thing because you always have to find silver linings even in the toughest times. The day before you go on your next round is when you feel your best.
You’re like, “Oh, my God, I feel like me. I have a little bit of energy. Oh, my gosh, I can actually drink water because it doesn’t taste disgusting.”
Those were my favorite days, and I always try to think, “Oh, what do I want to do because I feel well?” I make those days very special for me.
It’s crazy because I think I took for granted what it felt like to be me.

When did you lose hair?
I would say I immediately lost my hair. I thought I had time with my own hair, but I lost it literally maybe a week after the first round.
All my nurses said things like, “If you want a wig, we suggest you go look for a wig now before you lose your hair, if that’s something you’re looking into.” I did get a wig, I think, before I started.
Did you get a wig?
I did get a wig, which I didn’t really wear much except for when I was on the blog. In Chicago, they have this salon specifically for people with chronic illnesses.
It’s like a regular hair salon. It has all the bells and whistles, but it’s super clean and sanitized. They only have one patient in there.
You can select wigs to make you look like you, so before I even went in for my appointment, I had sent them a picture of myself. I walked in, and they had 5 or 6 different wigs that kind of looked like my hair.
I tried each one on, and then whatever one I feel comfortable with, that was mine. Then they’re willing to cut it, shape it, and color it however I wanted, which was incredible.
»MORE: Dealing with hair loss during cancer treatment
I did blog still when I was diagnosed. It was kind of my saving grace, if you call it, because during chemo you feel so sick, you feel so helpless, and it’s so hard to describe because it’s like an illness I’ve never felt before.
It wasn’t the cancer that made me sick. It was literally the treatments.
There are times where I felt like, “I don’t know if I could do this anymore.” I can see why it could be so easy to give up because there are times when you’re waking up, you don’t know how you’re gonna feel. You just don’t know how your body’s going to react.
No matter what meds the doctor prescribed you to alleviate the side effects, it’s still there, and you still feel like crap.
What were the chemo side effects
It’s a little hard to give a timeline, but I would say the day of chemo, it’s obviously a really long day, but I don’t think the side effects or any symptoms really start showing up then.
I know it’s different for everyone. Some may feel it immediately, but for me the day of, I was exhausted just from being at the hospital all day and the next day, too. I didn’t start experiencing side effects till a couple or a few days later.
It would first start with the nausea. I think nausea was definitely the worst. Then nothing tastes good.
Mainly everything tastes metallic-y, which makes it even harder to want to drink water, even though you’re supposed to stay hydrated. That was hard.
I would say one that I didn’t expect to have, even though I was told about it, was the mouth sores.
When I thought mouth sores, I thought maybe 1 or 2 here and there. No, this is like mouth sores where your entire mouth is coated in it.

That made it harder to even want to eat or talk, because it was painful. They did provide me this magic mouthwash, which kind of temporarily numbs the inside of your mouth just to make things a little bit more tolerable.
It comes in stages, every side effect. Sometimes, some weeks or some rounds, you’ll get a lot of them all at once. Then another side effect comes in.
You pretty much have your side effects up until a day or 2 before your next round, and that’s when you seriously just feel your best.
»MORE: Cancer patients share their treatment side effects
What helped with the side effects?
I pretty much just had to suck it up; I don’t know if there’s anything really you could do. They provided me Zofran and other anti-nausea meds. I tried to get on it before my next dose is due so there’s no gap, but it’s still there.
They always tell me, “Oh, whatever you do, don’t throw up. We want you to just keep it all in.” There were times where I was like, “I am so sick to my stomach I have to let it out.”
It’s so easy to want to give up because you just feel awful. There were times where I had my dark moments, and I thought, ‘I don’t know if I want to go through this anymore. I really don’t.’
If I came up with new side effects, I definitely let my team know. My husband is definitely frequently at the pharmacy, just picking up meds.
We actually had a good relationship with the pharmacist. I guess it’s a good or bad thing, right? You don’t want to always be there, but it’s kind of good.
Without them knowing fully what’s happening to me, they already knew, and they were very sweet about it. They tried to give tips and advice, which was really, really sweet of them.
What helped me was that I realized I’m young, and I still have a life to live.
Overall, I love my life, but I also know I have a life that I’m building with my husband, who has been the sweetest thing and the greatest blessing ever.
I want to fight for him; I want to be there with him. I want to have that family and live the dreams that we wanted to do.
We had a bucket list of things we wanted to do as newlyweds, and I felt bad because we couldn’t do them.
We literally had to put the newlywed life on hold. We didn’t experience that right after we got married, because I was diagnosed.
That gave me a little bit of a motivation. As far as handling it, I just try to be good with taking all these meds, but I mean I just really had to suck it up.
Sometimes getting a little fresh air helps, but sometimes it’s getting that push to get that fresh air.
My blog was one of the things that got me to go outside. My husband’s like, “Get ready, and even if we shoot for 10 minutes, then 10 minutes it is. We don’t have to do a full-on shoot.”
That 10 minutes of outside really help just for a little bit. It gave me that little push I needed, and it helped me feel better.
Blood pressure problems during chemo
One thing that did happen during chemo was my blood pressure. I’ve always had normal blood pressure, but during the second round, my blood pressure was really, really high — close to the 200s over 110.
It was just ridiculously high, to the point where they were a little scared because they weren’t sure if that was the Herceptin or if it was my heart working too hard.
Chemo is basically toxins in your body, so your heart probably is working a little extra hard. Also, I know heart disease and hypertension runs in my family.
During that time, it was also difficult to find the right blood pressure meds because they had to make sure whatever meds they were giving me also went well with chemo.
They found a couple of blood pressure meds that would pair well with chemo, but they didn’t work – they didn’t do anything – my blood pressure didn’t lower.
Eventually, we found a drug that worked. I actually had to go see a cardiologist who also dealt with cancer patients. It was really nice that they had something a little specialized. We did a little trial and error. That kind of helped stabilize my blood pressure.
When I was done with chemo, regarding Herceptin, I think I reacted to that very well. It was one of those things where it was just like another drug to take.
It’s a little bit hard. I didn’t even realize that you could still experience side effects when you’re done with chemo.
I had like a 10-year treatment plan overall. No matter what drug you take, you will experience side effects. Sometimes the side effects are similar to what you took from chemo, or sometimes the side effects from chemo just wait until after you’re done.
These are considered long-term side effects. Usually, doctors don’t know when that will ever go away. It’s one of those things that you just kind of have to work through regarding the whole survivorship.
Targeted Therapy
Describe your targeted therapy
One of my targeted therapies was Herceptin, and that’s why my chemo regimen was TCHP.
Whose decision was it to start targeted therapy?
It was the doctors, and I think it’s pretty common to have Herceptin with your chemo cocktail.
Describe the targeted therapy regimen
It was hard in the beginning because it was mixed in with all the other chemo drugs.
One of the things they wanted to look out for was that it could weaken your heart, so that was one of the side effects. They’ve been proactive with checking my heart.
Targeted therapy side effects
For targeted therapy with Herceptin, that was it. I did start another one when I was done with Herceptin, called Zometa.
With that, I experienced side effects the first round. It gives you flu-like symptoms, and I felt those symptoms immediately.
You just feel like you’re out of it, you feel sick to your stomach, you just feel like you have the flu, you have chills, and then you definitely have to pay attention for fevers.
Luckily, mine was never ever high enough that it resulted in going to the ER, but those are the few things that you have to look for.
Regarding hormone therapy, I had Zoladex. With them, I take the shots every 3 months. They also put me on aromatase inhibitor, and I use Aromasin for that.
In general, with this type of treatment, it just medically induced my body into menopause.
Here I am at 27, and my body goes into a complete 180.
That means your body just freaks out. You receive all the side effects that anyone has with menopause: hot flashes, bone aches, or bone pains.
There’s just like a slew of things, and it’s something that your body, at this age, should never go through.

Double Mastectomy Surgery
Describe the preparation before the double mastectomy
It’s kind of 2 parts. With my surgery, they wanted to make sure the lymph nodes are not affected. A week before my double mastectomy, they took out 6 sentinel lymph nodes — I can’t remember, 6 or 9 — and they did a biopsy on that.
If you’re not aware of it, if you tested positive for cancer on the sentinel lymph node, then chances are that other lymph nodes are affected. I was fortunate that those tested negative after chemo.
Also, that gave them a better game plan on how my surgery would be, because ideally I wanted a double mastectomy or bilateral mastectomy with immediate reconstruction.
But I was told, “If your lymph nodes are affected, then you’re going to need radiation, and we don’t recommend doing immediate reconstruction.”
It was nice that my lymph nodes came out clean.
A week later I had the double mastectomy scheduled, but it wasn’t guaranteed. It kind of depends on what they see while I’m under and if they think immediate reconstruction is a possibility.
If not, then I had to go through the expander route and then do reconstruction later down the road.
»MORE: Read more patient experiences with surgery
Describe the surgery
Fortunately, I was able to do a double mastectomy with immediate reconstruction. Overall, that surgery took 9 hours. My whole family was there, and it was a very long day for them.
What I didn’t realize was the recovery aspect of it and how much pain I would be in. You really lose your ability in your upper half.
They put on so much pain meds that I didn’t realize how much pain I was until they had to wean me off to a lower dose of pain meds.
Recovering from the mastectomy
That’s when you start feeling everything. It hurt so bad. I remember I had to go to the bathroom so badly, but I couldn’t even walk. I had 3 nurses helping me.
You’re also a little embarrassed because people had to help you use the bathroom. I’m so used to doing things on my own and these things that came so naturally to me, but now I required assistance to even go to the bathroom or have someone to lift me up.
I also got very nauseous from anesthesia.
It didn’t help that I was throwing up nonstop, which made the pain on my chest much worse.
I would say that was quite the experience. I’ve never felt that kind of pain before because before that, I’ve had very minor surgery, very easy procedures.
Going through such a major surgery was definitely a shocker. I didn’t realize how much I relied on other people to just do my day-to-day stuff. It was frustrating because I couldn’t just go to the bathroom.
I literally had to ask someone to help me with the shower and help me dress. Then when I had to come home from it, it was just annoying to have these drains on the side.
Then, basically being told, “Oh, you have to be pretty much bedridden the entire time.” That also really sucked because I couldn’t do much. Definitely an experience I do not recommend.
Deciding between a lumpectomy and a double mastectomy
There’s 2 things that I had to consider. One was symmetry. The mass on my right side, considering I had 4 tumors, literally took out a large quadrant of my breast.
They said, “We can’t really pump you up because you’re not large chested.” To me, I felt like if they’re already taking out that much, they might as well take out the whole thing.
Then I thought about my chances of getting breast cancer on the left side because I have it on the right.
They told me, “Well, you have a higher chance. Of course, these numbers are still low, but you have a higher chance of getting it on the left if you had it on the right.”
In my mind, I’m thinking, ‘If I’m going through cancer, I’m going to go all out to fight this. I hope and I pray to God that I don’t have to go through this again.’
That was my mindset, and I was like, “You know what? Just get rid of them, both sides.”
Describe your experience with the reconstruction surgery
I had that at the same time as my mastectomy. I chose implants. Before the surgery, I was not aware of how many options you can have.
Ultimately, I trusted my plastic surgeon to choose the implants that would look best on my body and will be great long-term. I also wanted one that was as close as possible to my original breast size.
I got comfortable in my own skin, so I just didn’t care to have large breasts.
I’m a fashion blogger and I already had outfits in mind of what I’d like to wear. I got accustomed to what clothes would look good on me.

Body positivity
Unfortunately, since my breasts were really small, they didn’t have implants that could be that small. They did warn me that at the end of it that they would probably be larger.
I think that was an adjustment, just waking up and having larger breasts than I’ve ever had.
For me, my confidence came from my clothes, so when realizing some of my clothes don’t fit, it just kind of made me feel sad because I didn’t have my go-to to help me feel confident.
I had to figure out my whole new groove, and that’s really hard because your groove is what comes natural to you.
I think that’s what most people don’t see — some people take for granted what comes natural to them. When you lose that ability, you just feel lost. I didn’t feel feminine at all.
I’ve put on quite a bit of weight from treatment, and that’s one of the side effects, too. I’m 20 pounds heavier than I’ve ever been.
It’s like a whole new adjustment to your body. I feel like I have these foreign objects on my chest. It doesn’t feel like it was part of my body.
It didn’t feel natural to me, especially when you’ve lost all feeling to your chest. When they remove your breast tissues, you lose all the nerves, too, so you lose feeling.
You don’t even have this connection for it to feel like your own body. That itself is a whole ‘nother journey.
Is there anything you did to help you through this process?
I had that surgery with the sentinel lymph node. As far as any preparation, really, no. I just made sure I had all the stuff I needed, so when I come home, I was equipped with it.
I was fortunate that I had a coworker who had a mastectomy in the past, who told me, “You would want these wedge pillow because it helps you sit up.”
I had to make sure I got myself the right pajamas so that I can fit in it. I knew I was going to be swollen in the chest, but I also know it was going to be hard for me to put clothes on.
I made sure it was button pajamas, something that can manage my hot flashes, because they were coming on really strong.
I also wanted to make sure I had food. I know my husband didn’t cook. I was the cook in the family, so I had to make sure there were things prepped.
I made sure we had family members to help out since I couldn’t really do much. I was pretty much told I’d have to be in bed the entire time.
I had to make sure I had family members home with me to be able to take me to the bathroom, feed me, change me. There was that kind of coordination prior to surgery.
Quality of Life
Were there any surprises during your treatment process?
The whole surprise is the whole body change. You don’t realize how much it affects your body physically and then how your body changes. It changes you mentally.
I thought in my mind, “You go through chemo, and then you’re done.” No, because then you still have all these other treatments that can change you day to day. There’s a whole new world you go into now.
People assume you are done with everything; you’re cured. There’s no such thing as the word ‘cured,’ which is why there’s people advocating for more cancer research.
I didn’t realize how deadly it is for young women with breast cancer, especially under the age of 40. It’s so underrepresented.
Someone who is 60 and someone who is 27 may get the same treatment plan, but your bodies are in different stages. Your lives are in different stages. The treatment changes all of that.
You see your friends and family able to move on and do things that you aspired to do, but you can’t. I think that’s really hard.
Were you surprised by your hair loss?
I was surprised how quickly it fell off, but I knew eventually it would. I thought I would be really sad at that point when I lost it, but it was more annoying because you lose so many chunks of hair.
You leave trails everywhere, and it was just annoying. No matter where I go, I’m just constantly shedding to the point where I told my husband, “Just shave it off. I can’t deal with this trail.”
I didn’t realize how much I missed it. That part was hard because I’ve grown to be very, very attached to the hair growth, constantly checking to see the progress, and I had pictured the length my hair would be in a certain amount of time.
It didn’t help with the fact that I already didn’t feel feminine. I’m not saying hair is everything, but hair was part of my identity and always has been, so it took me a long time to even get a haircut when I needed it.
My hair person totally understood what I was going through, and she was like, “Let me help you. If along the way you don’t like it, then we’ll stop.”
Something about the way she was talking, I knew she would take care of me. She did a good job making me feel a little bit more feminine.
Long story short, I didn’t feel the effect of the loss of hair until after everything.
What was the worst thing you experienced?
This one is bad and good in an odd way. It’s the side effects. You literally have no control over it.
It’s so easy to want to give up. I had to think about my life and think, “Oh, do I like my life? Do I love my life?”
I had to come to terms with death. Accepting it.
I told myself, ‘If today’s my last day or tomorrow’s my last day, that is okay.’
I knew I lived my life exactly the way I wanted. Not exactly, but I knew I lived a very good life.
To me, it’s very sad to know I got to that point, but at the same time, it was good in a way because it helped me every single day.
Even though I’m still going through the same crappy side effects, it helped me learn to be present and just be appreciative of each day.
It just made each day a little bit easier to want to get up.

What got you through the tough times?
Actually accepting death because then I learned to appreciate every single day.
Were there any moments you had to advocate for yourself?
The only time I had to advocate for myself is when I was trying to educate people in the non-cancer world to understand that I still have struggles and that I get sad.
I guess the misconception is when you don’t look sick, people don’t think you’re sick.

There’s always a battle everyone’s going through.
Even at my job, I was still doing a great job, but because I was nowhere in the same capacity as I was before, it just looked like I was slacking even though I was not.
They were very supportive, but at the end of the day, the work had to be done. I had to be the one to do it, but I couldn’t even get to that capacity.
»MORE: How to be a self-advocate as a patient
How important is it to have caregivers?
So important, and caregivers could be anyone. Mine was my husband, but it could be your mom, your dad, your sister, your friend, your neighbor, or another person in the cancer community.
One thing I am an advocate for is people don’t realize that caregivers go through cancer, too, and I feel like it’s harder for them than it is for the cancer patient.
I know how I’m feeling, and I have an idea of what I can handle and not handle.
But on their end, my husband wanted to do everything he could for me; he wants the whole cancer thing to go away, to be cured. They have that feeling of helplessness.
I always tell people they’re in cancer, too, and they see the struggle firsthand. But what sucks is that they’re helpless during the entire time. It affects them physically and mentally as well.
»MORE: What kind of support cancer patients say helped the most
How did cancer affect your relationship with your husband?
It definitely solidified our relationship. I knew who I was marrying would be the greatest person ever, but this definitely showed the kind of person he is.
During tough times, people’s real personality and how they manage challenges come through. I would say cancer would have been much harder if I didn’t have him.
I just feel bad that he had to go through this. I know how much it hurts him to see me hurt, but if anything, it has brought us closer and it actually helped us really understand marriage.
It taught us how to communicate and how to advocate, when to step back a little, and really learn to be there for each other.
Any advice for cancer patients on how to deal with a spouse during treatment?
If you’re the cancer patient, check to see how your spouse is doing. They’re in it. They struggle with cancer just as much, and they need all the help they can get. I think people don’t realize it.
They’re in it, and they feel it, just in a whole different way. It’s always nice to check to see where they are and if there’s anything you can do for them.
I know it affected my husband a lot mentally. Even after chemo, he had panic attacks just because the whole thing is very hard.
They also need to seek that support. Just be there for them or have them see someone, too.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
How did you deal with the financial aspects of treatment?
I grew up with the mindset of “hope for the best, plan for the worst,” so I actually have always been a big saver. It did financially impact us.
It’s always good to have fun with your money, but also learn to save and learn to strategize and plan out your finances. When it comes to times like health, you don’t want to take a step back on it.
I want to do everything I can for my own health or even my husband’s health or anyone in my family, and I don’t want money to be the reason to hold me back.
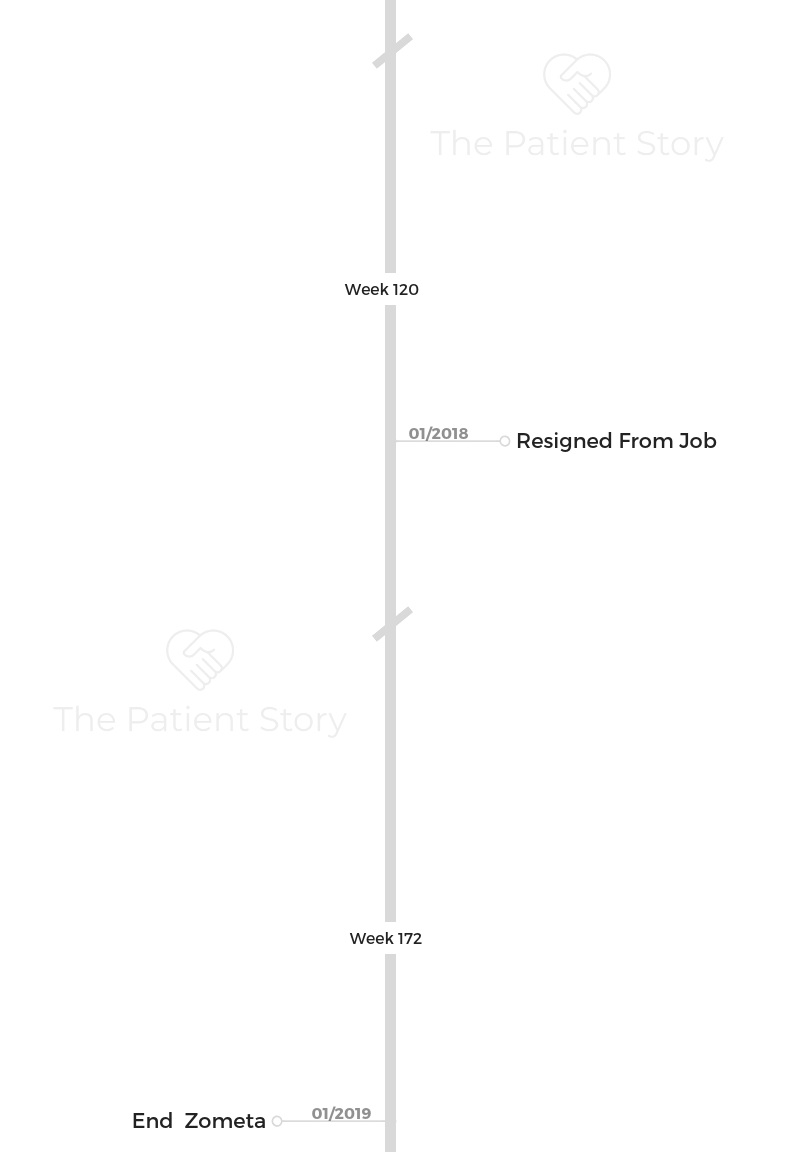
We were fortunate that my husband and I were big savers. What affected us the most is, I think a year after my diagnosis, it affected my husband to the point that he had a mental breakdown and had to quit his job.
Then there was a point where I quit my job, so there was a point where both of us were not working. It wasn’t easy. You just kind of have to thrive and use your best judgment.
For me, it was like, “Okay, it sucks that we may not having income coming in right now, but I think of the short-term sacrifice for the long-term benefit.”
Did you have any help preparing for outside of treatments (insurance, family cooking, etc.)?
We had insurance, which was good. Insurance is something you always have to challenge from time to time, so I would say if you are dealing with insurance, it’s always nice to have someone who checks that for you.
It’s work in [and of] itself. We have family that helps us from time to time. We also just learned to live a little bit more relaxed life and tried to utilize resources that made things easier.
For example, I can’t cook, so let’s sign up for Blue Apron. That way we don’t have to go out and grocery shop. Things are already preset for you, and really it’s just putting things together. Things like that.
Also, cutting down our expenses and thinking, “What do we want in our life? What can really fulfill us?”
It was really just getting more in tune with what we want out of life and using our resources.

Was there anything you wish you had known?
Honestly, no. The reason why is I think I was very thorough, and I treated every second opinion with every hospital as an interview.
I’m also very analytical and very process driven. I kind of tested each doctor. At the end of it, they ask, “Do you have any more questions?”
There’s some things that I would purposefully leave behind to see how quickly they would get back to me, or how they reacted to certain questions or when the patient responds to them.
That’s just my own personality. It helps me figure out who can I rely on when I need them on the spot. I felt like my life was on the line, and I wanted to make sure that this physician and her team were ready to take care of me.
I would like to share this with people: When you get a hospital bill, they don’t always go through insurance. My husband is an engineer, and I’ve done actuarial science.
We see numbers, and when we see it’s off, we see it very quickly. When we get a bill, we’re like, “Wait.” We notice immediately.
How did 3 out of the 4 doctor visits go through the insurance? Why am I paying the hospital when I really should be paying zero because I have already met my out-of-pocket deductible?
Those are the things I want to tell people. Just pay attention to your bill. Don’t assume you have to pay for everything.
Make sure you really look it out and vet it out. Then understand why you are being charged for this, because chances are there are mistakes. You don’t want to pay more than you have to.

Survivorship
Your “new normal”
You have to figure out your new groove.
I think the hardest part of it is that I didn’t even realize it, but it just kind of came naturally. I was constantly comparing who I am now to who I was before cancer.
I would be doing something, and I couldn’t do it as well. It’d be just frustrating. You have to learn this body that’s foreign to you.
The first year and a half was really hard. I was trying to get back to working full speed, and at the same time, I was still running my blog. I still had all these long-term side effects.
Understanding that I needed a community that understands what I’m going through, I started sharing a little bit more on social media so people could have a little glimpse of how, yes, I love fashion, but I’m also going through this thing.
I went to the Young Survivor Coalition Summit, where I found people, my community, who understood what I was going through.
They were the same age as I am, but we just feel lost. It’s a whole new world to navigate, understand, and figure out where you fit in.
I don’t fit in with other people my age because people are in different parts of their life now, while I had to put my life on hold to make sure I could live it.
The hard part is really, really, really trying to love this body, and it gets frustrating.
Then you have all the weight gain, and you still have these doctors visits in between. Everything just becomes overwhelming; your anxiety is just off the roof, and you’re having panic attacks.
I was just sharing with my onco-psychologist in my last visit that it took me up until recently to really feel like myself in a whole new way.
I really, really just love where I am and just feel very confident in who I am as a person.
Processing the cancer experience
It does affect a little bit of your quality of life, especially with the joint pains. I think the one that affected me the most is my wrist. I didn’t even realize how often I use my wrist.
I remember when I still had my day job, I was typing. Then I just couldn’t.
It was hard. I was holding a stack of binders, then I had to walk to my desk, and it just dropped because I just didn’t have the strength or my wrist was hurting.
Then you also experience what they call chemo brain, where things are just a little foggy and you can’t remember. Those are things that you can’t help. It gets very frustrating.
Certain things day to day used to come so naturally, and now I just blank out.
I remember I had to do this one process at work. Before cancer, I’m on it; I know it. I looked at the computer screen, and I was like, “I know how to do this, but I just can’t recall what to do.”
That was really sad because I obviously had to work at a different pace than what I was.
People don’t realize those are the things that you go through when you go through cancer treatment; your brain doesn’t fully function the same way, no matter how hard you want to try to get it there.
When I was back to work, I barely had hair, but overall, people said I look well.
When I’m struggling, no one gets why I am moving slower or why I can’t just do the work, meet those timelines, or get certain things to them right on the spot.
It takes quite a bit of time. That’s definitely a hard one. It’s a big adjustment to make. To this day, I still experience chemo brain, but I think I’ve learned to navigate it.
»MORE: Read different experiences of a cancer diagnosis and treatment
Was anyone crucial to your cancer experience?
I honestly am so grateful for that role of patient navigator, because they have made the whole process easier.
I didn’t know what her role was at that time. During my biopsy, she was sweet and made sure I was okay.
When I was done and getting dressed, she came over to me and said, “I want you to know just because you have a biopsy doesn’t mean you have cancer.”
I was like, “Okay.” She hands me a handbook. “You should read this from the American Cancer Society.”
I was like, “Wait what? This is so confusing. She’s telling me I probably don’t have cancer, but read a book about having cancer?”
My primary care doctor was naming all these doctors I should start seeing. I thought I had everything written down — I was trying to be diligent — but I didn’t.
10 minutes later I got off the phone, and that same patient navigator called me and said, “Hey, Rach, I want to let you know I just heard the news.”
Then she lists all these doctors. It was like, “Oh my gosh, those are exactly who I’m supposed to call.”
She’s like, ‘Don’t worry, I already have them scheduled for you. Do you have a pen and paper?’
She literally did everything for me.
She said, “I just wanted you to know that’s my role. I am here for you. I will advocate for you, and if some of the schedules don’t work out for you, you have to let me know. I will make everything possible to make it work for you.”
To this day, I am still so grateful for her. I don’t know how I would’ve handled trying to figure out how to schedule appointments and making sure they were all aligned properly if it wasn’t for her.
Any advice for cancer patients going through a similar experience?
I would say don’t compare.
I think the hardest part when I was also diagnosed is that I would tell people what I had, and they would say, “Well, why aren’t you doing this?”
Or, “Oh, so-and-so is doing this. Maybe you should do that.” You’ve just got to listen to your gut. Do what works for you.
For me, looking for a second opinion is what helped me figure out my best plan of action, but it doesn’t necessarily mean that’s what you have to go through.
You’ve really got to listen to yourself and listen to your intuition, because that’s what will help you get through the process.
If you don’t feel comfortable from the beginning, it’s just going to make every single day much harder.

Last message to other patients
Know that it’s a process and you’re going to have hard days. It’s going to be hard, but know that you’ve got to listen to your body and let it recover.
It’s going to take time, and it took me 3 years to get to where I am, and I still struggle day to day. But just know that there are good things that happen along the way.
As crappy as cancer is, there are good things that happen. I found friendships that I never ever thought I would ever have come across if it wasn’t for cancer, or really found the people that really care about me and are really there for me.
So there are silver linings, and I would say even in your darkest moments, find them.
Even if it’s a stranger that bought you a cup of coffee or you find a penny on the floor, those silver linings mean something.

Inspired by Rach's story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation