Genoa’s Stage 3, IDC, HER2+ Breast Cancer Story
Genoa shares her stage 3 HER2+ breast cancer story and describes her treatment, including chemotherapy, why she chose a lumpectomy over a mastectomy, and radiation.
In her story, Genoa also highlights many important quality-of-life issues, like dealing with the hair loss, working through treatment, and being a patient self-advocate.

- Name: Genoa M.
- Diagnosis:
- Breast cancer
- Invasive ductal carcinoma (IDC)
- HER2 positive (HER2+)
- Staging:
- 3
- 1st Symptoms:
- Nausea
- Treatment:
- Chemotherapy
- Taxanes (Taxotere)
- Carboplatin
- Trastuzumab (Herceptin)
- Lumpectomy
- Radiation
- Chemotherapy
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I just assumed that that diagnosis meant the end of life as I knew it, and I’m here to tell you that it does not, and it did not.
Cancer is no longer the death sentence I used to think it was growing up or what I feared it might be.
Genoa M.

Diagnosis & Tests
What was your diagnosis?
I had stage 3, HER2+, which is an estrogen-positive breast cancer. It was aggressive.
I had been feeding it. Basically, I had had an estrogen-patch that I attached to my butt every 2 weeks to help me through menopause. All that had happened was I had accelerated [it].
Through medical intervention trying to help me manage my menopausal symptoms and re-balance my hormones, I had accelerated something in my breast that was cancerous.
The best description I ever had was from a nurse practitioner [who] drew me a diagram on the sheet that they cover the examination bed with.
She drew me a diagram and said, ‘Here are the ducts in your breast. Really, what’s going on is your cells are having a party outside of the ducts, and we need to get them back into the ductwork.’
You are having an outrageous party in your breast outside of the ductwork, and that’s why you have a tumor. That made the most sense to me.
How did you get diagnosed?
My life at the time was simply that I was living in a city I’d always wanted to live in with a husband I’d always wanted to be with. I had a stepson who had made it to university, and I was working in my career.
Despite all these wonderful things, I felt nauseous.
I think as women we know that nausea is there for a reason. I for sure knew I wasn’t pregnant because I had had a hysterectomy, I was older in life, and I was in menopause.
If I felt nauseous, that meant something was really wrong. When something’s wrong, you intuitively know to go get some help. That’s how I knew something was off.
I was due for my annual mammogram, and I went to see my OB-GYN. As luck would have it — or maybe the universe was taking care of me — I had hit my deductible on my annual health insurance.
My OB-GYN, in addition to requesting my mammogram, also said, “Why don’t you have an MRI? You’ve had a history of breast cancer in your family, so let’s do an MRI as a baseline.”
I thought that was a fantastic idea. I also let her know I felt nauseated. She’s like, “I don’t know why you’d feel nauseous.” There was absolutely no reason at all to be feeling icky. I just felt icky, so I scheduled my mammogram.
Describe the MRI
It was incredible. I actually managed to have my MRI scheduled on the same day. I don’t know that you typically get both the appointments that you want on the same day, but that’s how it worked out for me.
I do think there was something very special going on because by the time I got to my mammogram in the afternoon, the results of my MRI had already gone through. They did a very different mammogram because they knew exactly where to go.
The fact that it wasn’t just a technician doing my diagnostic mammogram with an ultrasound — it was a radiology doctor — I knew something wasn’t good.
I knew something was wrong because I felt nauseous, so it was almost as if, “Okay, they’re taking me seriously. They’re not just saying we don’t know why you feel nauseous. They’re looking for something.”
They were looking for something on the right breast. They let me re-gown and sit up. Then they told me they could see a tumor-like mass, and they would need to do a biopsy the next morning.
All I remember was the doctor telling me they’d found the mass, and then the technician just gently rubbed my back while I breathed.
All I wanted to do was put my street clothes back on, go home, and find my husband.
What were the next steps?
(In 2 days: MRI → mammogram → breast biospy)
I consider myself so fortunate to be able to get that much help that quickly. Once I knew the biopsy [was] the next morning, they were already talking to me about getting a surgeon.
I was thinking, “You can take a tumor out, but what about the rest? How far has it gone?” All I could remember from my mother’s cancer — she also had breast cancer in another country a long, long time ago — they had not checked the lymph node.
Her tumor was in her breast, but the lymph node also had cancer cells. The lymph node is the gateway to the rest of the body, so I was thinking you must check the lymph node. Don’t just do a biopsy on the tumor itself.
I won’t say they fully dismissed it, but they were very much, ‘If you need chemotherapy and your tumor is malignant, then we’re going to just blitz everything.’
That wasn’t good enough for me because I wanted to know — I was almost obsessed with knowing — has my cancer spread?
They took the biopsy and put a clip in to tell where the tumor was. The clip was very important because the surgeon then went looking for the clip in order to take the tumor out.
Basically in 48 hours, I’d had an MRI, a diagnostic mammogram, a biopsy, then they sent me home for the weekend. You needed at least 3 days to get results.
Biopsy and scan results
We waited it out. It was everything you could imagine in a long weekend of not knowing and imagining everything in between.
Then I got the call on the Tuesday to say it definitely was cancer and to come back in. They would walk me through my diagnosis.
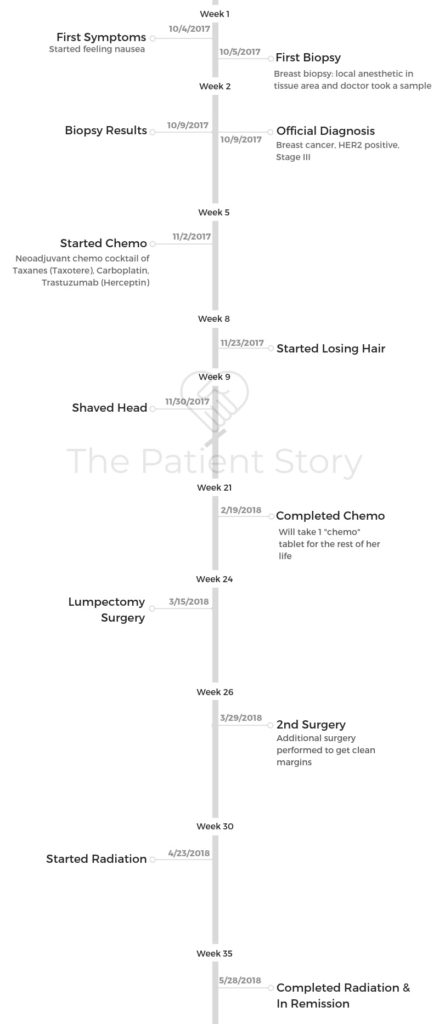
We went back in, and they actually did a wonderful job of explaining to me what my full diagnosis was [and] giving me a lot of information about the pathology from the biopsy. It was late September. I actually started chemo in October. We went really fast.
What is a clip?
The clip is a marker. When you have a biopsy, they’re already in your breast. They’ve already taken a sample of the tumor and the growth.
Before they take the needle out, they put a tiny marker. It’s like a metal clip. and they put it in there to say, “This is the place. This is where the trouble is.”
For any ultrasound or any surgery you have afterwards, that’s how they go looking for that. That’s how they map it all out.
Describe the breast biopsy
That actually didn’t hurt too much. It was once they put the local anesthetic in the tissue area. I was fine until they took a sample. When cancer is in a cellular form, everything is angry and upset, and the cellularity is compromised.
When they actually took the sample, I did feel the pinch. I felt a sharp pinch, and then it withdrew. I know I reacted, and they said, “Don’t worry. It hurts because everything is wrong, basically. We hit it. The fact that you felt it means we got a target, and we’re not going to do anything else.”
How did you decide between a lumpectomy and mastectomy?
There’s some big information here I do understand and would love to share, because you have the option of breast conservation if you want it [or] if you are really anxious.
My aunt did this after her chemotherapy because of my late mother. She decided to have a mastectomy just as a prevention.
She did the Angelina Jolie. Take it away. That for her was sanity-given, and they offered that to me. If I felt that would give me my best emotional chance of recovery, they would have taken the breast off and then worked on reconstruction.
The good news is for all women that they now know enough about how breast cancer behaves so that your chances of survivorship are just the same if you have a lumpectomy or a mastectomy.
It’s more about do you feel better not having the breast there? I actually felt better having the breast there. I chose breast conservation and a lumpectomy.

How did you choose hospitals?
I went to my usual OB-GYN for the mammogram. Because I was already getting care there, that’s where they did my MRI and breast biopsy. For chemo, I changed to another hospital because the chemistry between me and the first medical team was not what I wanted.
Then they tried to set me up with an oncologist and a surgeon within their own system. I had appointments with both the oncologist and surgeon that same week, so they definitely moved quickly.
The problem was I didn’t feel that I was with the right oncologist and surgeon. It wasn’t that they were incompetent in any way. Their style wasn’t working for me, if that makes sense.
I’m a very visual person and an emotional person, so their body language wasn’t feeling good to me. I didn’t know that I could develop a relationship with them so I could tell them how I really felt or where my concerns were.
Even their offices made me feel depressed and insecure. I kept looking at where they would give me my chemo and thinking, “Well, I’m going to be so sad sitting in that chair in this depressing room doing something I don’t want to do anyway.”
When your gut’s telling you that nothing’s coming together, you should probably listen to it.
Chemotherapy & Side Effects
How did you determine treatment?
What they wanted to do was shrink the tumor first, then remove it surgically.
Their recommendation was go through chemo, try and get the best response we can, and then it can be significantly reduced. Then we’ll go in and take it out, and you’ll have radiation.
Describe the chemo regimen
It was neoadjuvant chemotherapy, including taxanes (Taxotere), carboplatin, and trastuzumab (Herceptin).
How did chemo go?
Your first infusion is your staging infusion, and it takes pretty much the whole day.
After that they can go quicker and speed up. About halfway through, I was having the 4 bags over 45 minutes to almost 30 minutes. They were speeding me up and speeding me up. The side effects were the same, but you didn’t have to stay there as long.
The best advice I had about getting through the day of chemo — and it makes total sense if you think about it — just get up and move.
Don’t just sit there and let all the meds flood through your system. The best thing you can do is move around and get them to move around.
I found I was able to disperse a lot of the nausea and a little bit of my anxiety, too. Just get everything. The more I drank, the more I flushed. The more I moved, the more things moved around me. I definitely felt better for it.

What were the chemo side effects?
- nausea
- fatigue
- constipation
- diarrhea
Describe the side effect cycle
Days 4 and 5 were the toughest days. If you knew they were coming, you kind of just built everything around it. Days 1, 2, and 3 I just always felt floaty and drugged up.
Days 4 and 5 were the hardest: nausea or just energy, emotions. [It] got better on day 6 and got better on day 7. It was just the drugs working their way through my system.
Week 2 was always the rebuild. You’re coming back off. Week 3 was, “I’m actually feeling pretty good.” Then you go right back to week 1. I had constipation, diarrhea, so bizarrely both, and then the nausea.
The really good learning from all of that is take your side effects straight back to your oncologist and team, because they can adjust your dosages.
What made you feel better?
You don’t want to exercise. With all your being, the last thing you want to do is exercise or move, but you must because you will feel better.
I’m not an athlete by any means, but I could swim and could walk. As long as I moved and tried to do those things, even though I felt crappy, I would always feel better afterwards.
The other thing I learned was however nauseous I felt and however much I didn’t want to eat, if I ate through my nausea, I’d feel better, too. It really is true.
Then fluids. I’ve never been someone that wants to have 8 glasses of water a day. I still don’t want to have 8 glasses of water a day, but I would just take my big 1.5 liter bottles and keep refilling them.
It just made so much sense to me. I wanted to flush all the impurities out. The only way to do that was to drink a lot of water.
Radiation Therapy
Heading into radiation
Happy it was less than I thought it’d be. It is once a day every day for the whole month of May, except weekends.
Negotiating less radiation
My radiation [was] shorter than I feared. Again, you can negotiate. Your doctor will tell you that you need to have a standard. They’re supposed to tell you, and they will, that the standard radiation is 5 weeks plus a booster week, so 6 weeks of radiation.
The reason they tell you it’s a full 6 weeks is because there are 15 years of research attached to that being the best protocol. However, there are 5 years of research to say that 3 weeks and a booster week yields the same results.
They’re required to tell you that the standard is 6. Going to a hospital every day for 6 weeks is overwhelming.
Radiation, just like chemo, has side effects and other issues. It fixes 1 problem but maybe creates others.
When I really dug in and really pushed, turns out they’re very comfortable with less, as long as they’ve fully expressed to you it’s your choice.
The moral of that story is you are in charge of your health, and you have the right to ask and the right to negotiate your own treatment plan.
»MORE: How to be a self-advocate as a patient
Managing Hair Loss
Describe the hair loss
I did not understand my relationship with my hair until I was diagnosed. I think the times I broke down and cried over my diagnosis were triggered because I knew my hair was going.
Doing this interview without a wig on is one of my first attempts to be braver about not wearing a wig. I wanted to choose this opportunity to get braver and get more okay with not having hair, or at least not having the hair I would’ve liked to have.
I did not understand how much my identity was wrapped up in being able to brush my hair. When you start losing it, it’s so traumatic. You know it’s coming, and I think you resist — well, I did.
I fought against it. But every time you touch your hair and there’s a chunk, or roll over on your pillow and leave hair on one side of your pillow, you realize that’s actually more distressing.
I have a really amazing hairdresser, and I knew it was time to take all my hair off. I also had gone and gotten a wig, the kind of wig you needed cut.
I called my hairdresser, and I’m like, “Okay, Ed, I’m coming in. We have 2 missions. 1, I need a buzz cut. 2, I need you to cut my wig into something that looks like me.”
He did both of those things. He was so supportive and so kind. It was liberating having what was left of my hair cut off. It was definitely more distressing leaving it there.
I don’t know that every woman feels this way, but I kind of needed to just get it over with.

When did you decide to cut your hair?
I needed to get control back a little bit.
All of a sudden, you lose your hair after the second chemo. It’s almost like clockwork. It was after the second chemo. I just made it through Thanksgiving mostly with hair.
I was about 8 weeks in. All of a sudden, I wasn’t worried about shedding. I had a bob cut to my chin. If every time I turned around I was losing hair, it was so distressing.
It was liberating to not have that emotion on top of, “I’ve got a tumor. I need to deal with this because I really like life, and I don’t want this to rob me of anything.”
Did you wear a wig?
Yes. I hate wearing the wig. 2 weeks post-chemo, it looked like a shadow on my head, but there were tiny little hairs growing.
Today, knowing that you were coming and knowing that I wanted to show up just me and not me with a wig, I looked in the mirror and I’m like, “Could I see myself going into the office without a wig? Stuff’s happening.”
I don’t think I’m quite there, but I’m almost there. I am so looking forward to when I can go, “Yeah, I’m good to go in.” I’m closer. Hopefully, really close.
Also, I’ve realized the wig makes other people feel more comfortable. That took pressure off me, but I hate that damn wig.
There was this amazing quote I saw on the front page of a magazine at Stanford, “Don’t let cancer be the most interesting thing about you.”
I was like that was for me. If I lead with it or let other people lead with it, then I’ve lost myself utterly.
Wearing a wig has helped everybody else. Here I am for a meeting, here I am sending an email, and regular things happen.
Most people would always want to ask me how I was, and I’m like, “Honestly, I’m fine and just happy to be here. Thank you, but let’s get going and not let it be all about my cancer.” I had other comments about things.
Why did you decide against cold caps?
There were 2 things. 1, they didn’t guarantee effectivity. Once I understood that they needed to be changed every 30 minutes for 24 hours, they’re really, really cold, and the pressure is on the person with you to keep changing. You rent a special ice-cold thing that keeps the next one you’re supposed to put on cold.
I just thought, “I’m not going to put any more pressure on myself or my husband to go through changing those, and if they don’t guarantee that you’re not going to lose your hair then, this is already hard enough and they’re expensive. So screw it.”

Quality of Life
Did you work through treatment?
The crazy thing for me was — and this might be other people’s reality — I needed to not go on sick leave. I actually kept working.
The weeks of chemo, I was lucky enough to work from home, and I pretty much dragged myself through my meetings and my calls. I’d put a hat on and dial in on a Google hangout.
I could do my email from my couch if I needed to, but I didn’t really distract myself through TV or reading. I just tried to move and tried to show up for work and keep it moving.

I think the economic reality for a lot of people is earning 70% of your income by going on sick leave, if you’re lucky enough even to have sick leave, is such a hit to your budget.
It doesn’t help you get better knowing that your finances are compromised. All I knew was I didn’t need that added pressure for my family.
I remember my mom and my aunt having chemo, and they were in positions where they really didn’t have careers. I just thought, ‘Well, I’m in a very resource-rich city, and medicine’s come a long way.’
I had a very supportive family, too. I had a very supportive team. My management were not very supportive, but my team was supportive.
I knew every day that I made it into the office, they would make me feel so welcome. They would encourage me and motivate me, and they did that.
I also learned to tell certain people what I was going through because I knew they were very motivational and very warm, loving people.
I picked certain people who didn’t necessarily work on my team but I would see as I walked into the office or in elevators. I let them know (about the cancer) because I’m a private person.
They would give me a hug and go, “Genoa, you’re here!” I’m like, “I know!” Knowing that I would see those people helped.
»MORE: Working during cancer treatment
What do you wish you had known before the diagnosis?
The thing I wished I had known but I know now is that cancer is no longer a death sentence.
For any woman watching this and has been diagnosed with breast cancer, you particularly need to know that there has been so much research and so much medical progression in our type of cancer that you are already on a winning team.
Because my mother had died of breast cancer 17 years ago and my aunt struggled with it, I assumed my struggle was going to be the same, but no. It’s come a long way, and it is by no means going to kill me.
The minute I accepted it wasn’t going to kill me, I was like, “Right, I just want to get this dealt with so I can move on and enjoy my life.” That’s what I wish I had known, because I spent a lot of time freaking out.
Integrative and Eastern medicine
I did not come up with this, so I take no credit for it, but the best thing I did was go see a Chinese medical doctor who specializes in cancer and [is] an acupuncturist.
The 2 disciplines together with my chemo, I actually think I’m coming out of this probably a more whole person incredibly.
My hormones are balanced, and I feel so good about life. Do not just take a traditional approach to your treatment.
»MORE: Read patient experiences on yoga and meditation
What surprised you the most during treatment?
What surprised me the most was where the best support came from. It came from people I didn’t expect and I didn’t anticipate telling. But I’m so glad I did, because their support and their help.
Don’t assume anything going into this. Be open to love and support coming from all sorts of places, all sorts of unexpected places. It will surprise you how uplifting it can be.
How to be your own self-advocate
I just took the approach, “These are the side effects. They were on the sheet they gave me for each of the drugs, so check that box.” It wasn’t until my second round when the nurse practitioner’s like, “You know you don’t have to suffer quite this much?”
I was like, “Okay, that would be nice. Is that allowed?” Silly me, I should have made a big fuss after the first round and not waited to see if it’s as bad the second round.
When the dosages were adjusted for me, it got more tolerable, then just stayed consistently the same. Nothing really changed.
You are in charge of your treatment. Ask. They can always make changes, and you’re not being a wimp. I think there’s this thing about chemo — it’s meant to be awful, because cancer is awful.
If it’s awful and you get through it, then you’re definitely going to be cured. It doesn’t have to be awful, and you don’t have to fight through it. You can still be cured. It gets a really bad rap is what I’ve learned.
» MORE: How to Be Your Own Advocate

Inspired by Genoa's story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation