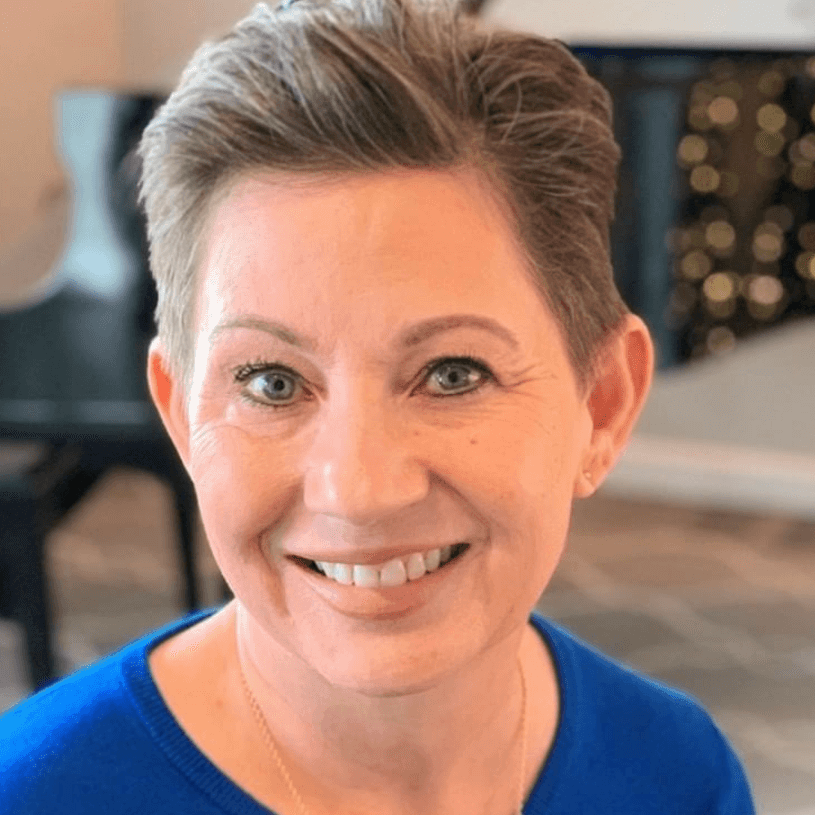
Andrea’s Stage 2B/3 IDC Breast Cancer While Pregnant Story
Andrea shares her stage 2B to stage 3 breast cancer story, which was found during pregnancy. She describes how she got through treatment, including chemotherapy, multiple surgeries like mastectomy and reconstruction, and radiation.
In her story, Andrea highlights how the breast cancer diagnosis affected her marriage, how she handled treatment as a parent, and gives guidance on how people can ask for help and support.

- Name: Andrea A.
- Diagnosis:
- Breast cancer
- Invasive ductal carcinoma
- Staging: On the border of 2B/3
- 1st Symptoms:
- Divot in breast
- Found during pregnancy
- Treatment:
- Chemotherapy
- 4 rounds of “pregnancy-safe” chemo
- 4 rounds of Taxol
- Surgery
- Nipple lift in preparation for mastectomy
- Mastectomy
- Reconstruction
- Implant removal due to infection
- Radiation
- Chemotherapy
When you come out on the other side, you will feel a deeper meaning and purpose for your life.
View it almost as a blessing, even though this is the scariest and hardest time of your life.
Andrea A.
- Diagnosis
- Chemotherapy
- Surgery & Radiation
- Functional Medicine
- Reflections
- Processing hair loss
- What’s your “new normal?”
- How has the whole experience affected your relationship with your husband?
- How did the cancer affect you emotionally as a new mother?
- Did you have a strong support system?
- It can be hard to ask for help. How did you handle that?
- What advice do you have for someone who is newly diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
When did you first go to the doctor?
I was pregnant. I had noticed a divot in my breast, and I just thought it was a milk gland. I hadn’t brought it up to anyone at my weekly OB-GYN appointments until I went in for my week 30 checkup.
I almost didn’t say something, but at the end, I said, ‘By the way, I have this spot in my breast.’
For an otherwise stoic doctor, she freaked out a bit. She seemed concerned. She did a quick ultrasound with the wand, and she said it was concerning, so she wanted me to go to the breast center that day.
I went to the breast center. My husband met me there. They did a biopsy on my breast and lymph nodes. They went in with the needle.
What was the needle biopsy like?
It was the most excruciating experience of my life, probably. The breast biopsy didn’t hurt at all, but the one for the lymph node was wrapped around a nerve. There wasn’t really anything they could do for nerve pain.
My husband was out in the lobby, and he could hear me. It was so painful. They had to take it out and go back in because they didn’t get an adequate sample the first time.
Processing the diagnosis
The doctor said she was concerned and that I definitely had breast cancer. I had already been thinking cancer after the OB-GYN appointment, but it was still an out-of-body experience. It was so surreal.
I’m not really a Pollyanna. I usually hope for the best and plan for the worst, so I think I knew. I was still in shock, though.
I got the full diagnosis the next morning. That’s when the full results of everything came back. I got set up with an oncologist for the following week.
»MORE: Patients share how they processed a cancer diagnosis
Cancer treatment plan
When meeting with the oncologist, it was just chemo talk mostly. I was pregnant, so they went over the protocol for that with me.
I was supposed to do chemo, the mastectomy, and then go into radiation. It was just marching orders all laid out for me.

Chemotherapy
Describe the chemo regimen
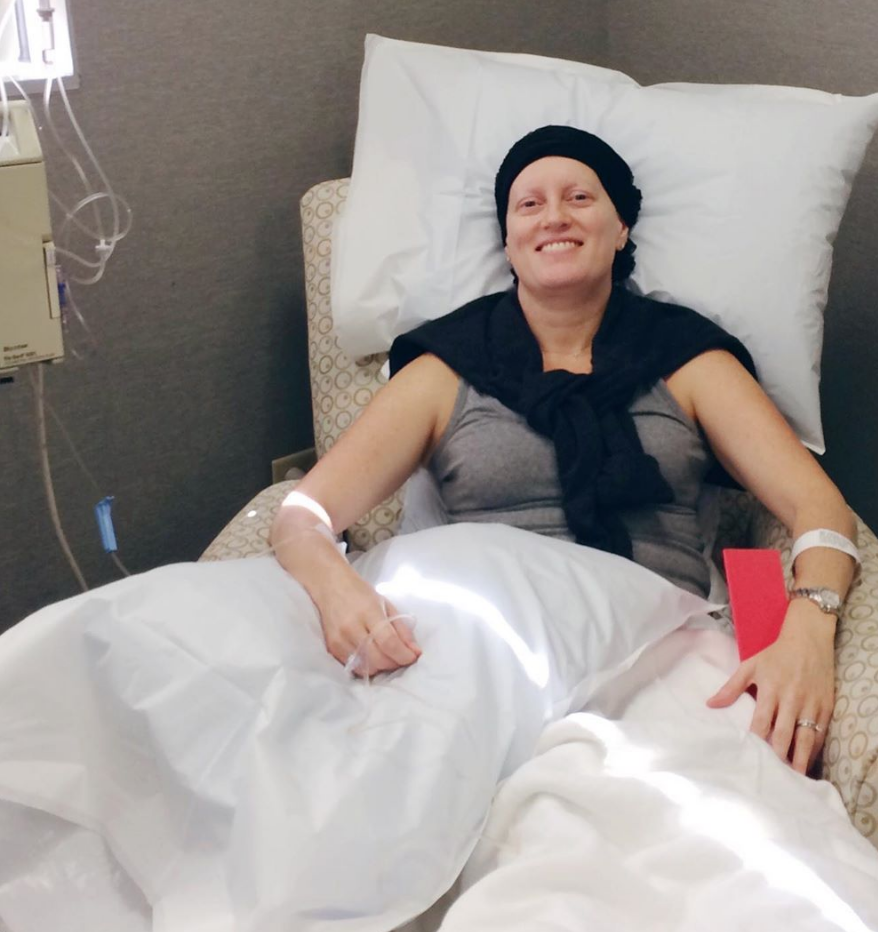
The regimen was 4 cycles of what was considered a pregnancy-safe chemo. The last 4 would be Taxol. I went every other Thursday. The first couple of times, it didn’t hurt as much.
I didn’t get a port. I didn’t know that would be a good idea. My veins got so sensitive after a few infusions, so it was pretty painful.
The first session was strange because I was pregnant. The IV was more painful than the chemo itself.
Sitting back, observing the sick people in the room, and watching the nurses put this poison in you while they’re wearing hazard suits is just so weird.
Describe the hair loss
After a week, my hair started coming out in the shower. I tried to get to my baby shower with my hair intact because I didn’t want to tell anyone I was going through cancer yet.
I made it to that 2-week mark, had my baby shower, and the cycle after that, clumps just came out. I shaved it after that.
I made it through the third pregnancy-safe cycle, and I didn’t want to do it anymore. I was probably week 37 at this point, and when I would sit in the chair, my son would be bouncing around in my belly. I didn’t want to do the fourth.
I gave birth between cycle 3 and 4. I took about a month off, and I finished 4 through 8.
»MORE: Dealing with hair loss during cancer treatment
Going through chemo during pregnancy
I felt horrible. I can’t find the words. I get choked up about it.
I was really jacked up. I was watching and reading a bunch of things about functional medicine and watching a docuseries on chemo.
I hated having to wonder if I was increasing my son’s risk of cancer by treating my own. You just never know what’s going to happen until they’re born, but I felt like garbage because I thought I was endangering him.
The newborn bliss and joy of being a new mommy wasn’t really something I got to experience at all because of the diagnosis and treatment.
What side effects did you experience from chemo?
I didn’t have any issues from my pregnancy. I had no nausea or anything. I was working out and everything, so I know all the side effects I experienced were from chemo and not pregnancy.
I had so much fatigue. It was unreal. I had a lot of pain. The first 72 hours after chemo, I had flu-like symptoms. It was sheer exhaustion, depression, and loneliness. I had zero energy.
I immediately started trying to eat even better, and I was looking into what I could do to keep myself healthy. It wasn’t until the last 5 rounds after I had given birth that things really got worse as far as nausea and vomiting.
Taxol was a really aggressive treatment. I had severe neuropathy in my hands and feet. I couldn’t really walk because of the painful tingling. I ended up telling my oncologist to down my dosage, and the neuropathy was more manageable after that.
I lost my eyebrows and eyelashes immediately after starting Taxol pretty much. I had cancer face at that point, so that was hard. The side effects were more intense on Taxol.
»MORE: Cancer patients share their treatment side effects
What helped fight the chemo side effects?
At the time, I was juicing daily. I was drinking green juice. I was trying to stay away from a bunch of carbs.
I ate a lot of veggies. I drank a lot of water and tried to rest.
Surgery & Radiation
Describe mastectomy prep
I had a nipple lift to prepare for the mastectomy. That was a little surgery. I had anesthesia and stayed one night in the hospital, but it really wasn’t a big deal.
My own personal preparation was just coming to terms with what was happening. I just wanted everything to happen as fast as possible because I didn’t want my son to have any memory of any of this.
I took pictures of my breasts because that was going to be all I had left of them. I came to terms with that. I prepared mentally for an 8-hour surgery and a few-day hospital stay.
The whole thing was just sad for me because I knew I was going to need help for about a month after surgery with my son. I wasn’t going to be able to hold him until I was fully recovered, and that was harder than the surgery itself.
There was no physical prep that I had to do. I just showed up that morning, got wheeled in, and hooked up to IVs.
Recovering from surgery
I was very drugged up, but I remember glimpses of waking up from surgery. I have low blood pressure to begin with, and I remember the nurses coming in constantly because my alarm was going off, and I wasn’t breathing.
They would say, ‘Breathe, Andrea, you’ve got to breathe.’
All night long the first night after waking up from surgery, that went on.
I was so drugged up, though, that I don’t really remember anything else. I don’t remember going home even. I don’t remember anyone who visited.
I didn’t have a lot of pain. My recovery was about 2 weeks, even though they told me it would be about a month or better. I feel like I rebounded pretty fast.
»MORE: Read more patient experiences with surgery
How was radiation?
I put my arm up in the machine, and they radiated a section of my breast. That was 28 rounds. I did that every day except for holidays.
I didn’t want to be doing it. I actually argued with the radiologist. I was like, “Why do I even need to do this?” I had already had the mastectomy. He said, “If I were you, I’d want to do everything I could to be alive for my son.”
I was very angry about feeling forced to do radiation. I probably would’ve done it had I had a choice, but I didn’t want to be doing it.
I had expanders in from surgery plus radiation, so my skin was just rock hard. My skin blistered and was peeling off. I got so raw sometimes that I would need to take a day off.
They gave me Aquaphor, and I’d slather that on. It actually helped, but you’re still frying your skin.
I had big-time fatigue and nausea from the radiation as well. I underestimated the impact it was going to have on my energy level.
I had just started a new job before radiation, and I was so exhausted. I was in a state of chronic fatigue for about a year afterwards.
How were you feeling about ending treatment?
I was so happy to be done and feeling like I could get on with my life and heal. I knew that I was broken in a lot of ways.
But I knew that I’m a strong person. I knew that the hard work to heal myself was just beginning.
I knew I needed to take this experience and use it for a reason. I got pretty philosophical. It was a very pivotal moment for me. I realized I needed to truly connect with what fuels my spirit.

Describe the breast reconstruction
I had been getting my expanders filled periodically before radiation. The surgery was technically easier than the mastectomy, but I had complications. I had an infection, and I had to go the ER.
The bottom right half of my breast was burning red, and I went to see my doctor. She said I needed to get the implant taken out on that side, so I did, and I didn’t have it replaced.
Is there anything you wish you would’ve known at the beginning of treatment?
I wish I had known to take my time.
If I could turn back time, I would’ve insisted on a chemo sensitivity test. I found out about that through my own research.
Everywhere else in the world, they have pretty amazing cancer screenings, one of which is a chemo sensitivity test.
Some doctors in Western medicine will do them. You get it, and it tells you what chemo and what natural agents will fight your cancer best. That would’ve been incredible information to have.
Are you dealing with any long-term side effects?
Mostly, it’s the mental thing. I feel like I’m getting better, but I’m still getting accustomed to not having a breast.
I’ve had to learn to find a bra that allows me to fake it until I make it. There are limitations as far as not feeling as comfortable as I used to.
I’m finally coming out of the fog, and it’s been 4 years. I’m finally starting to get to a better place. I don’t break down in tears like I used to on certain dates.
The feelings are still raw sometimes, but it’s not as bad as it used to be. I don’t ever want to forget, but I want to move forward. The more I talk and digest and process it, I can see a little bit more clearly.
Functional Medicine
Your thoughts on functional and integrative medicine
It’s an approach around treating the patient, not the tumor.
You have to understand that we’re not in touch with all of the different elements and levers in our body. In the world of holistic and functional medicine, it’s about all the axes of the person.
It’s about your spiritual, mental, emotional, and physical health. You’re addressing all dimensions of self. Based on all of those different areas and given that person’s current lifestyle, what can we do to go at it from all different angles and get to the root cause?
At the end of the day, why do you think you got sick? Most patients will tell you. They’ve got a pretty good understanding of how they’ve been living their life in all areas. That’s not addressed in most conventional medicine settings, unfortunately.
»MORE: Read other patient experiences on yoga and meditation
What changes did you make to your lifestyle?
My first big obstacle was my diet. I had a pretty powerful sugar addiction. I didn’t even realize that until I was told not to eat sugar.
We all know we’re supposed to eat vegetables. I had zero idea how to cook vegetables. I had to learn. I did a complete 180. The catalyst for me as far as real diet change was when my mother-in-law came to visit. She’s Greek, so thank God for her and Mediterranean-style cooking.
I was a fumbling crybaby for the first year because I was always hungry, and I couldn’t figure out what to eat. She helped me see the simplicity in Mediterranean-style vegetables. They were so delicious.
That sparked other changes. I took supplements. Everything I started doing was about my immune system. I detoxed my liver. I needed to address my chronic inflammation, which is the precursor to all disease.
I addressed my connection to myself. I didn’t really journal. I wish I would have. I would just sit and reflect. It was a full-time job to take care of myself, but it was worth it. Thankfully, I was in a position to take a full year off.
For detoxing, I did daily green juicing for 3 years. I still green juice, but it’s only a few times a week now. I did coffee enemas. I went to the infrared sauna, and I drank lots of water.
To address the inflammation, I used turmeric supplementation. I ate anti-inflammatory foods. Everything was alkaline. Everything was green. If anyone does the anti-cancer and anti-inflammatory diets, they’re all the same foods.
I focused on the short list of foods I could eat, and I rallied around that. I focused on portion control for animal meat. At the end of the day, everything needed to be centered around plants with a limited amount of animal proteins, and absolutely no sugar.
What you’ve learned about living a more holistic lifestyle
Some folks might think that changing your lifestyle or diet doesn’t really make that big of an impact. I would challenge them to think differently.
Every 3 months, I was checking my blood work and markers. Everything I was doing showed up in my blood work. If I slacked, it would show in my blood work.
It makes a very profound impact. There is a much better way of existence.
Cancer is your body’s way of waking you up. Slow down long enough to hear what your body is telling you and embrace it. It can absolutely change your life.

Reflections
Processing hair loss
It was really hard. I’ve always had long, flowy hair. It’s thick and black. I’m a minimalist as far as makeup and all that stuff, so it was always all about the hair.
When all that came flying off into the drain, the sensation itself of the hair coming out was heebie jeebies.
Then when you look at yourself in the mirror, it’s so difficult. I wouldn’t hardly look at myself in the mirror for 2 years because I felt so ugly. I was so sick, and I just couldn’t deal with it.
There was nothing about the visual that I wanted to look at. I wasn’t really hard on myself, but it was more like I just didn’t want to see myself like that.
When I looked really sick, I didn’t even know who I was. I wouldn’t recognize me on the street. I looked so different.
The chemo changed me so much. It’s hard to believe what I went through and how I looked like that. That’s the emotional work that has to be done. You have to grieve and mourn your old self.
The symbol of losing your hair is like the shedding of your old life. It’s not going to be the same again, and you have to grieve and accept that. It took me 2 or 3 years to get my hair to look halfway normal.
Every time you look in the mirror for a long time, you’re reminded that you were so sick. It looks different for a long time, and it’s hard to accept that difference sometimes.
What’s your “new normal?”
I was this lively, successful, and professional woman. I was going places and doing things.

All the while, though, I knew wasn’t really joyful in my life. I had known that for quite some time. I was burnt out and exhausted.
Now, there’s a greater depth about me. I place more importance on prioritizing myself now. I don’t let anyone or anything derail me from taking care of me.
I take care of myself, I put myself first in a non-selfish way, and I do everything I can to show love to this body and this mind. I slow down and allow spiritual growth.
On a personal level, I’ve always been a Christian. I spend more time now in really developing my faith. It’s led me to be able to be a much more calm and peaceful person. I don’t let things get under my skin.
How has the whole experience affected your relationship with your husband?
Not well, actually. We ended up separating. We got hit with the stresses of new parenting, he was in the process of starting a new business, I got cancer, and then my mom died of cancer. The hits just kept coming.
Even if one person is trying to get healthy, the other one is holding you back. I needed peace in my fragile state. I accepted that I may very well have been the screwed-up one in the relationship, but I knew I needed to protect my space and my energy.
I couldn’t willingly let toxicity literally bring me right back into cancer. It went back to that life lesson: ‘Who am I going to love more? Myself or someone else?’
If I couldn’t love myself enough, I was going to get cancer again. We amicably separated. We still see each other, but we are separated.
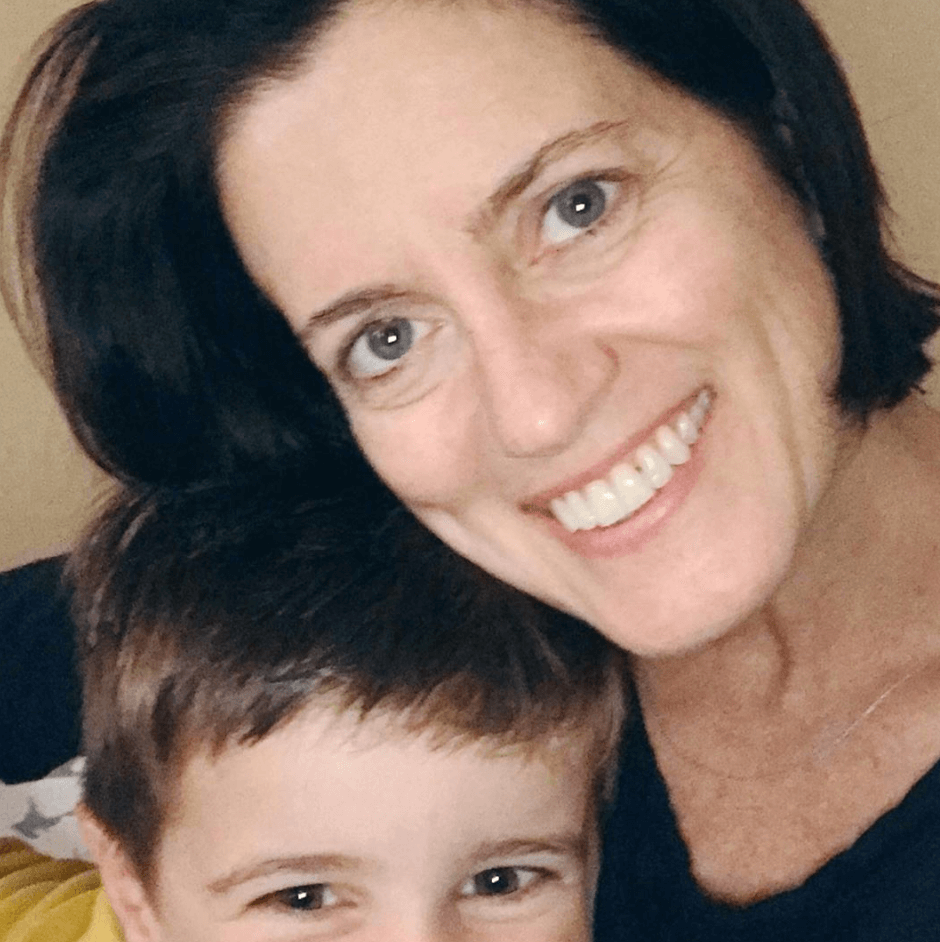
How did the cancer affect you emotionally as a new mother?
It affected me greatly. I felt like I didn’t get a chance to truly bond with my son. I’m sure at some unspoken level, he could feel my fear and stress.
He probably picked up on that. I beat myself up a lot over that. I was very distracted by that.
I was always in pain or had to go throw up. I couldn’t be really present. That pisses me off to this day. I’m making progress with it, but it makes me angry. At the time, I was extremely upset. You have to grieve that, too.
I was preparing to take 2 years off, so I had saved a bunch of money to be able to take off of work and be with my son. God has a sense of humor, I guess, because I had my disability plus my savings, so I was able to hire a nanny.
Did you have a strong support system?
My old work colleagues would come sit with me in chemo. My husband came the first few times.
I had friends who would come sit with me. My family isn’t local, except for my dad. He would come to my surgeries.
There were 2 women from work who went above and beyond. They sent me gifts and helped me. My mom came down a few times to stay with me.
Work friends and other friends really rallied around me, but those 2 ladies from work were especially there for me.
»MORE: What kind of support cancer patients say helped the most

It can be hard to ask for help. How did you handle that?
It was very hard for me. I still feel like I’m inconvenient sometimes. I don’t like troubling anyone.
My friends and family would remind me I needed to ask for help. Then they just started doing things without me asking, which was so much help.
I got better at it. It got easier. As women, we’re so programmed to take care of everything. It’s ridiculous. There’s some chip in our brain or something. I’m a high performer by default.
What advice do you have for someone who is newly diagnosed?
Go deep within. Let go of control. Do not fear. You will be fine. You will get through this, and you will find a strength that you never knew you had inside of you. When you come out on the other side, you will feel a deeper meaning and purpose for your life.
View it almost as a blessing, even though this is the scariest and hardest time of your life. This will be used for good and a higher purpose that you can’t see yet, so have faith.

Inspired by Andrea's story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump found during self breast exam
Treatment: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Cancer details: IDC is most common kind of breast cancer. Stage 1B.
1st Symptoms: None, caught by delayed mammogram
Treatment: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in right breast
Treatment: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Cancer Details: ER/PR positive = estrogen and progesterone receptor positive
1st Symptoms: Lump found on breast
Treatment: Lumpectomy, AC/T chemotherapy, radiation, and hormone therapy (Lupron and Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in breast
Treatment: Chemo, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Tightness and lump in left breast
Treatment: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: chemotherapy, lumpectomy, radiation
Doreen D., IDC, Stage 2A, Triple Positive
Cancer details: IDC is most common kind of breast cancer. Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in left breast
Treatment: Neoadjuvant chemotherapy (TCHP), lumpectomy, radiation
Melissa H., Stage 2B, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Lump in left breast
Treatment: Mastectomy, chemotherapy, 2nd mastectomy
Genoa M., IDC, Stage 3, HER2+
Cancer details: HER2-positive tends to be more aggressive than HER2-negative cases
1st Symptoms: Nausea
Treatment: Chemotherapy, radiation
Andrea A., IDC, Stage 2B/3, ER+
Cancer details: Found cancer while pregnant
1st Symptoms: Divot in breast
Treatment: Chemotherapy, radiation, surgery
Stephanie J., Stage 3, Triple Negative, BRCA1+
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer
1st Symptoms: Lump in left breast
Treatment: Chemotherapy, surgery
Renee N., IDC, Stage 3-4, HER2+
Cancer details: IDC is most common kind of breast cancer.
1st Symptoms: Lump in breast
Treatment: chemotherapy, bilateral mastectomy, radiation
Shari S., Stage 4, Metastatic, Triple Positive
Cancer details: Triple positive = positive for HER2, estrogen receptor (ER), progesterone receptor (PR)
1st Symptoms: Lump in breast
Treatment: Surgery, chemotherapy, radiation
Erin C., IDC, Stage 2B/4, Metastatic, Triple Negative
Cancer details: Triple negative doesn’t have any receptors commonly found in breast cancer making it harder to treat
1st Symptoms: Pain in breast
Treatment: Surgery, chemotherapy, radiation
Margaret A., IDC & DCIS, Stage 2B
Cancer details: IDC is most common kind of breast cancer. DCIS means cancer has not spread into surrounding breast tissue
1st Symptoms: Pain in left breast, left nipple inverting
Treatment: Double mastectomy, chemo (AC-T), Radiation
Abigail J., Stage 4, Metastatic
Cancer Details: HER2-low, node negative, PIK3CA mutation
1st Symptoms: Back and leg pain, lump in breast
Treatment: Surgery, chemotherapy, radiation, CDK4/6 inhibitors
Bethany W., Stage 2, ER+
Symptoms: Lump in breast and armpit
Treatment: Chemotherapy, double mastectomy, radiation
Bethany W., Stage 4 Metastatic
Symptoms: Lower back pain
Treatment: Chemotherapy, radiation, maintenance treatment
Lainie J., IDC, Stage 2, HER2+
Symptoms: Lump in breast
Treatment: Chemotherapy, double mastectomy, radiation