Amelia’s Stage 1 IDC, ER+, PR+, HER2- Breast Cancer Story
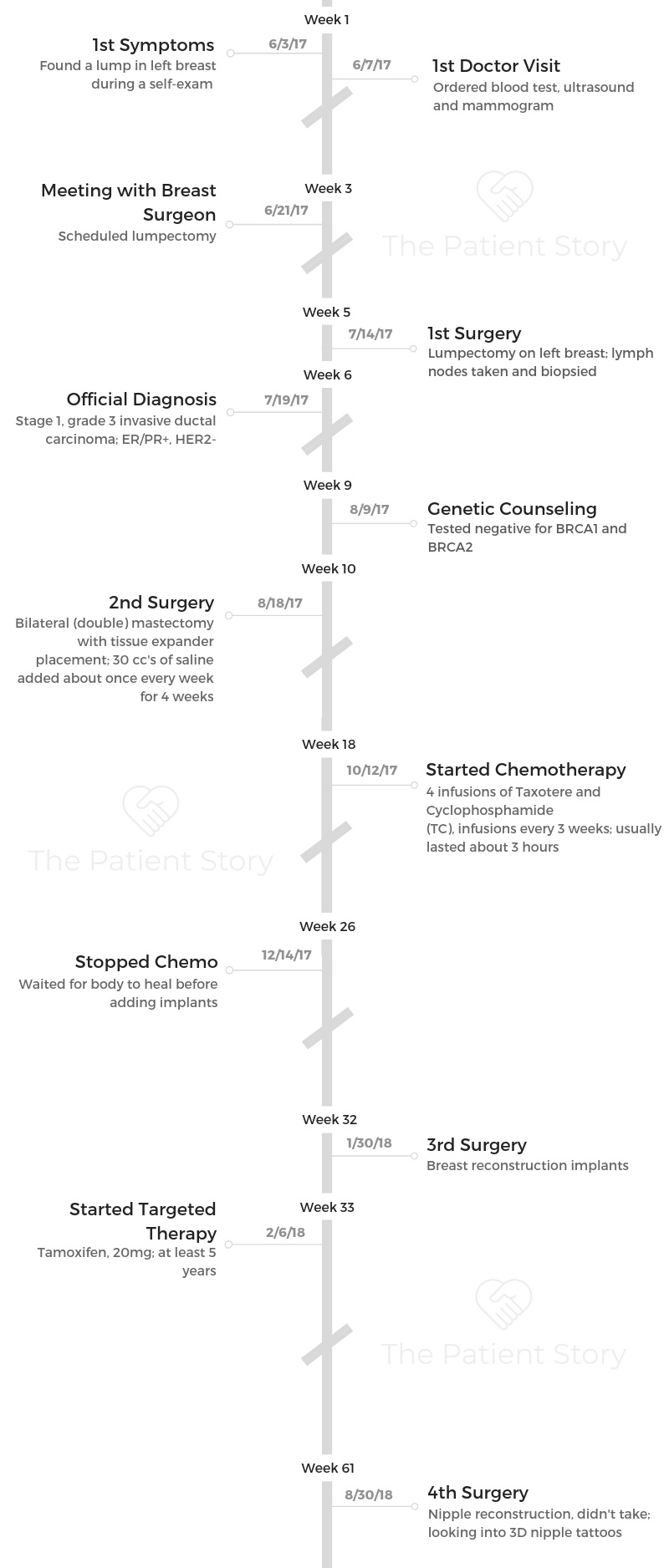
Amelia shares her stage 1 breast cancer story, which took her through a lumpectomy, double mastectomy, breast and nipple reconstruction, chemotherapy, and targeted therapy.
In her story, Amelia also describes how she navigated through several issues, like managing hair loss, the significance of getting a mastectomy tattoo, and survivorship.

- Name: Amelia L.
- Diagnosis:
- Breast cancer
- Invasive ductal carcinoma (IDC)
- ER/PR+, HER2-
- Staging: Stage 1, grade 3
- 1st Symptoms:
- Lump found in breast during self-exam
- Treatment:
- Surgery
- Lumpectomy of left breast (had 1st lumpectomy 20 years prior)
- Bilateral (double) mastectomy
- Breast reconstruction with implants
- Nipple reconstruction
- Chemotherapy
- Taxotere (docetaxel) and cyclophosphamide (Cytoxan) (TC)
- Infusions once every 3 weeks for 12 weeks
- Taxotere (docetaxel) and cyclophosphamide (Cytoxan) (TC)
- Targeted Therapy
- Tamoxifen
- Daily for at least 5 years
- Tamoxifen
- Surgery
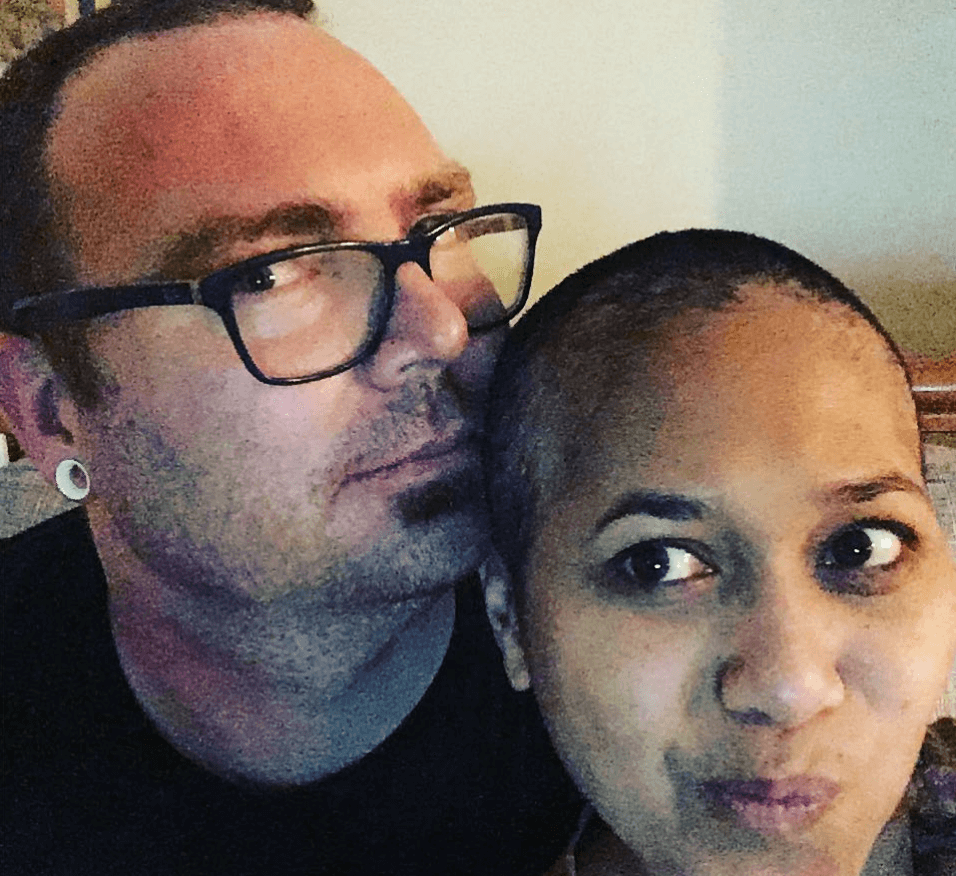
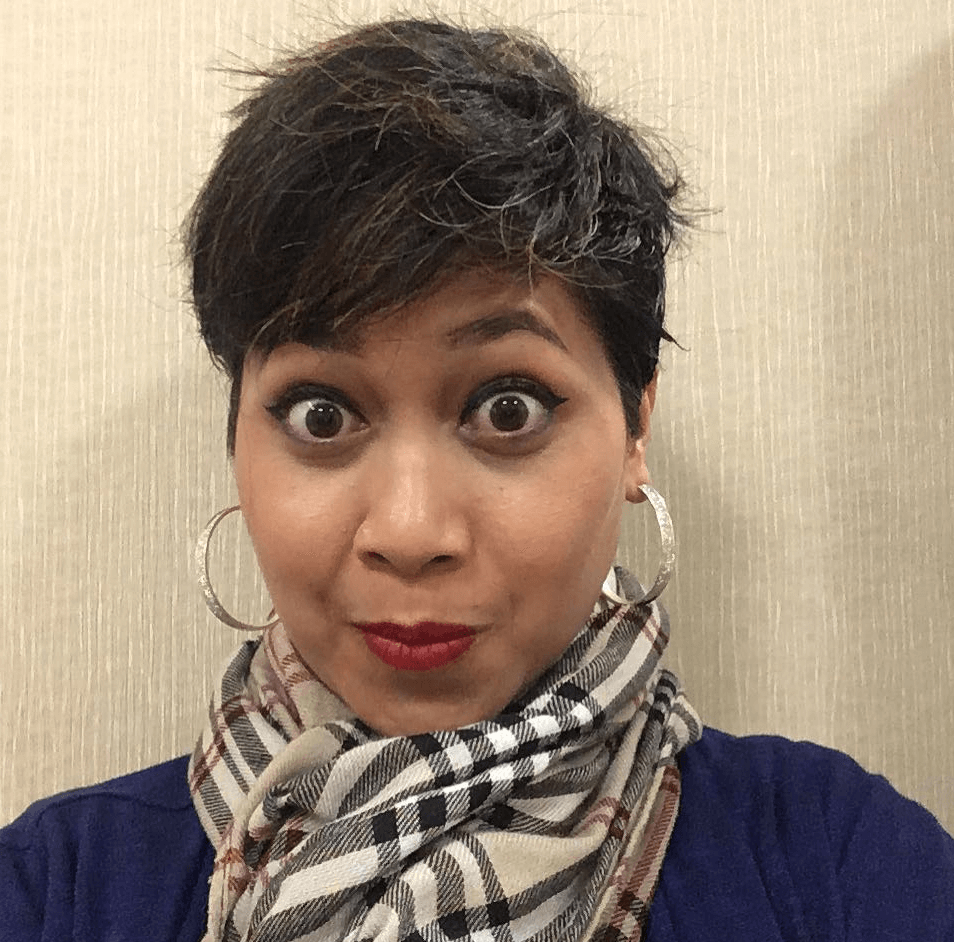
When I lost my hair, I had a new confidence. I don’t know what it was, but maybe it was the ‘battle’ mentality. I was really confident with my short, buzzed haircut.
That stuck with me for a long time. I don’t get nervous anymore.
It’s almost like the opposite of the story of Samson. When they cut his hair, he lost his power, right?
When I cut my hair, I felt like I gained so much power.
Amelia L.
- Diagnosis & Testing
- Mastectomy & Recovery
- Chemotherapy
- Reconstruction
- Survivorship
- What’s the ongoing follow-up protocol?
- What is your “new normal” after cancer?
- What was the lowest point you had?
- How did the cancer affect your relationship?
- Any advice for married cancer patients?
- How did your kids handle the diagnosis?
- How was the financial aspect of treatment?
- Do you have any advice for someone who has just been diagnosed?
- Hair Loss
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis & Testing
What were your first symptoms?
I found my first lump back in 2002. I was in my 20s then. Ever since then, I’ve always taken the time to do a monthly breast exam. I had a lumpectomy back then.
This time, I had just turned 40. I was due for my mammogram that year. I was lying in bed, doing a normal self-exam.
I noticed there was a lump in a different spot than the first one. My first lumpectomy was on the left side of my nipple. This was on the right side.
I felt the lump and knew it hadn’t been there the month before. It felt different than the first one, which had been benign.
I don’t know if it was because I’m more knowledgeable about breast cancer now since awareness is everywhere these days or what, but I felt a sense of urgency about this one.
I had heard that it’s better to do the self breast exam when you’re lying down if you’re small-breasted.
They usually recommend you do it in the shower, but if I had been doing it standing up, I don’t know that I would’ve found it.
When I was lying down, it was more prominent, and I could feel it. It wasn’t big. It was less than a centimeter.

Primary care doctor visit
I had just seen my primary care right before turning 40. I called her and made an appointment.
She fit me in that week. She did a breast exam, too.
She said, “I don’t want to scare you, but since you’re 40 anyway, let’s go ahead and do a mammogram and ultrasound.”
Referral to a breast surgeon
After the results came back abnormal, I met with a breast surgeon. The immediate next step was to do a lumpectomy and try to get it out.
Then they did a biopsy on it. It was found to be cancerous. My first thought was a double mastectomy.
At that point, I was like, “I’m 40. I still have another 40 years. I don’t want to leave anything to chance.”
I wanted to get everything out that we could possibly get. Because I made that decision so quickly, I didn’t talk to an oncologist until after that surgery.
It was like a normal doctor appointment. Maybe that’s because I was trying to downplay it and not freak out, but it was really normal. My husband was with me. I wasn’t nervous or scared.
Can you walk us through the lumpectomy?
It was pretty easy for me. I’ve had 2 C-sections and had the right side of my thyroid removed, so it was no big deal.
It’s just a small incision on the site of the lump, so you have stitches when you wake up.
I didn’t really have to prep for it, except I couldn’t eat or drink anything starting the night before, so I was starving the day of the surgery.
Surgery took 2 hours, and it was outpatient, so I was home that afternoon.
I don’t remember waking up and being in a lot of pain. That’s the great thing about modern medicine. I think I only came home with a prescription dose of ibuprofen or something.
When were you officially diagnosed?
Cancer wasn’t even on my mind yet. It didn’t really sink in until I got the call from the breast surgeon right after the lumpectomy.
She didn’t say it on the phone, but she did say she needed to see me right away. That’s when I was like, “Okay, this is cancerous.”
The first person I told was my 13-year-old daughter. That was the first and only time that I cried throughout the experience.
We didn’t even know for sure until I went to see the surgeon again, but when I had to tell her it might be cancerous, I got emotional. I just had a feeling.
My husband and I went in on July 19th. She came in and had a diagram of what different cancers look like. She was showing me the ones I have. She wrote down all the treatment options on the back.
We had already done a lumpectomy. I had decided to do a double mastectomy and didn’t know if I would need chemo.
If I hadn’t decided to do the surgery, it would’ve been radiation and chemo. We didn’t know for sure what type I had, so we didn’t know if chemo was an option.
She just really wanted to get our minds set on dealing with cancer now.
»MORE: Patients share how they processed a cancer diagnosis
How did you tell your husband you had cancer?
He works from home, which is great because that’s how he was able to be with me. I took the call in my living room.
My kids were home on break. I literally just turned around and told him, “The doctor wants to see me immediately.”
I have kind of a short attention span, so having him there with me for appointments was great. He would remember things that I don’t remember.
I couldn’t take notes and try to listen at the same time, so he was like my own personal notebook. He probably asked more questions than I did.
I was just going through the motions. I didn’t see the point of getting more information on things if I was going to have to go through them anyway, but he wanted to get all the information. He wanted to know side effects to look for and things to do.
What happened after the official diagnosis?
I have a weird medical history. I actually had a heart attack after my second pregnancy. It was pregnancy-related.
Because of that, they wanted to make sure my heart could handle the mastectomy. I went to see a cardiologist first. Then I saw a plastic surgeon because I wanted to do immediate reconstruction.
I also saw a genetic counselor. I didn’t see an oncologist until after my mastectomy.
Describe the genetic counseling
My nurse navigator planned everything for me. She knew the people I needed to see and made the appointments for me. One of those was a genetic counselor.
It was to figure out if I had the BRCA gene mutation, and I didn’t. I wanted to know if I needed to get my daughters tested. Also, had I tested positive, the approach would’ve been different.
It was a simple process. I can’t remember if it was a simple blood test or if I had to spit in a cup or something. I had been prodded and pricked so much that it was no big deal.
»MORE: Read our interview with a genetic counselor
Mastectomy & Recovery
Can you talk about the mastectomy prep?
The prep was a little more involved than the lumpectomy since I’d be staying in the hospital for a few days. I had a list of things to bring to the hospital, like my phone charger and things like that.
I had nodes removed on both sides, so I had limited mobility in my arms after surgery. Especially with all the dressing they have on you, it’s hard to really do much.
I brought a ton of pillows because that’s what they told me to do. They wanted me to put one on my chest when we were driving back home from the hospital.
We knew I was going to have drains attached to me for a little bit. People warned us that there might be leakage.
Before we left, we set my chaise up in my project room. We put a bunch of pillows on it, and it was low enough to the ground that I could get up easily.
That’s where I stayed for a few weeks after the surgery. If anything leaked, it was easy to take care of.
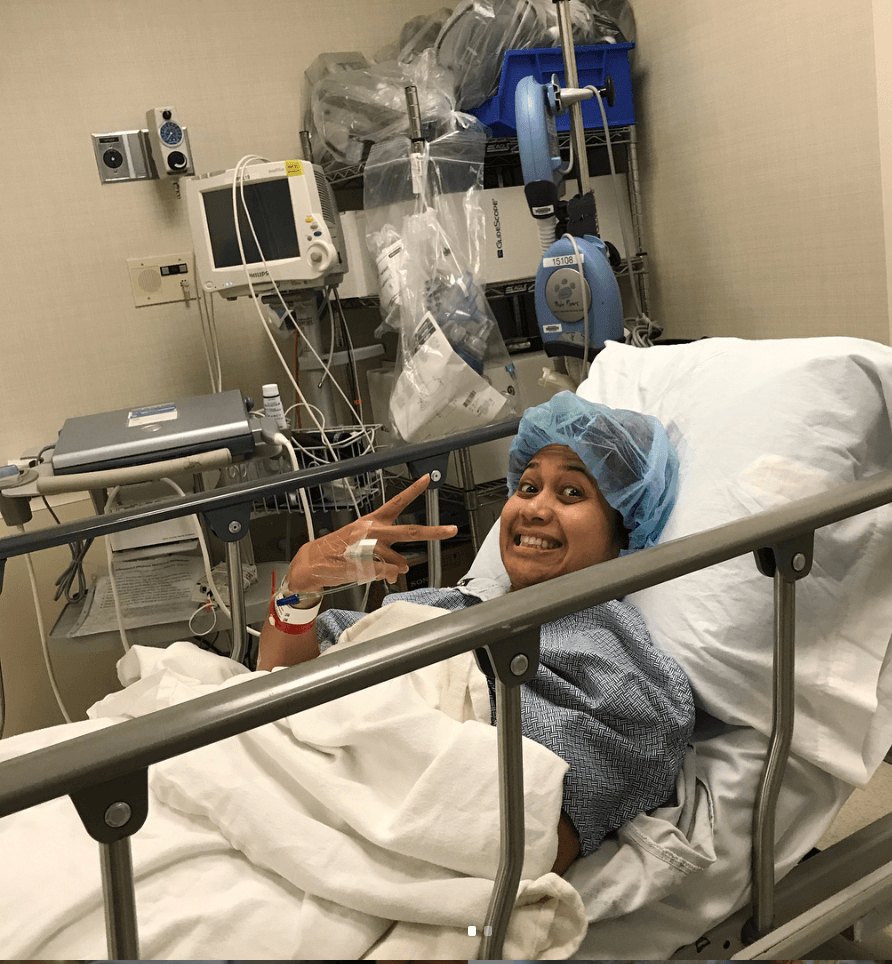
How were you feeling before surgery?
I wasn’t nervous. I didn’t see a reason to be nervous. I already knew it was cancer. I already knew it could kill me. I had a ‘going into battle’ attitude.
I was just ready to go. I wanted to get everything over with. It might just be my coping mechanism, but I went into survival mode.
I also knew my kids would be watching. If cancer can happen to me, it can happen to anyone. I wanted to show them that cancer is not as scary as it used to be. I wanted to be very upfront with them. They saw everything.
I wanted to reassure them that cancer is not a death sentence anymore. It still takes many lives every year, but my case was doable. Half of surviving is having a good attitude. I didn’t want to victimize myself.
How long was your recovery at home after the mastectomy?
I took full advantage of my short-term disability. My employer covers up to 12 weeks of full pay. I think I was ready to go back to work after 10 weeks, but I wanted to make sure that I was good to go.
I was up and moving around the day after I got home. I just couldn’t really lift my arms. I was doing a lot of little exercises to increase my mobility. After the 12 weeks, I went back to work.
Chemotherapy
You had to decide if you wanted to go through chemo or not
My mastectomy was in August. After that, we did an oncotype test. They wanted to make sure we had the right approach.
The oncotype came back 22. That’s in the gray area. From zero to 18, no chemo is needed because it doesn’t make a difference in your recurrence probability.
From 19 to 30-something, they don’t have enough evidence to show that chemo would reduce your chance of recurrence. It’s kind of up in the air. 40 and above is when you definitely have to have chemo.
I was ready to throw everything I had into this. I wanted to do the chemo.
My husband was very adamantly against the chemo. He saw one of his friends die from cancer. It really left an emotional scar for him. He didn’t want to see me that way. He didn’t want to see me lose a lot of weight, lose all my hair, and be sick all the time. He was not convinced that it was the right thing.
We went to see the oncologist then. She couldn’t give us a recommendation. She said it was completely up to us. I knew that whatever decision I made, I had to be okay with it.
I didn’t want to live with regrets. I didn’t want to ask myself what I would’ve wanted to do differently.
My husband and I just needed to come to a consensus. I know I’m the one who was going through the cancer, but he was the one that was going to be right there beside me the whole time.
It’s such an emotional task to ask your loved ones to take care of you.
We did some research. I created a typical pros and cons list. I didn’t want to leave anything off the table. Even if chemo only reduced my chances of recurrence a tiny bit, I still wanted to do it.
One of the things we learned was that the type of chemo cocktail they were going to give me actually makes you gain weight because of the steroid. Little things that helped sway our decision.
I went to another doctor at another facility for a final recommendation. She looked through my history. She said, “If you didn’t have the lumpectomy in 2002, I probably would’ve said no to chemo, but since you have a history of growths, I would recommend it.”
Before this, I had told my oncologist to schedule chemo just in case. I was at my 89th day post-diagnosis when I got the recommendation.
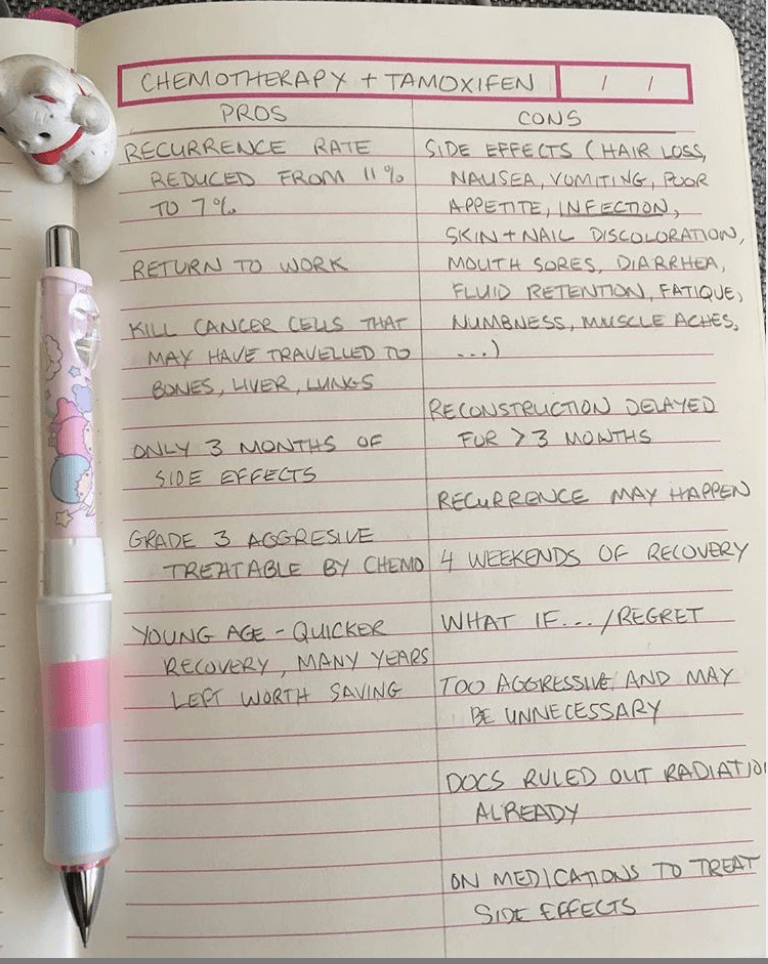
They told me I had a higher chance of surviving if I started chemo within 3 months. I literally waited until the day before the last day, but then I went in for my first session.
Deciding whether or not to do the chemo was the hardest part of the whole process.
What was your chemo regimen like?
Because of my oncotype and how small the cancer was, my oncologist wanted to go for TC. That’s Taxotere and cyclophosphamide. It’s one of the least toxic chemos there is. Mine was only 4 infusions.
I did one infusion every 3 weeks. It wasn’t even a full day. I would get to the cancer center at about 9:00 a.m. I would be on the chair from about 10:00 a.m. until 1:00 p.m., and be out about 30 minutes later. If I could’ve had any type of cancer, this was the easiest one I could’ve had.
The effects from the chemo were still the typical things, though. I lost my hair and everything, but the chemo itself was not that bad. It was a big deal, but it wasn’t.
I did everything my oncologist told me to do. I made a little chart with all my meds on it and would put a checkmark next to each one every day. They have apps on your phone for that now, but I like the physical list.
I stayed on top of my medicine. I rinsed my mouth with salt water to prevent mouth sores and all that. I did everything I could.
The only really bad side effect I had was the fatigue. I was so tired, and I wasn’t expecting that level of fatigue.
I also lost all my taste buds. Everything tasted like cardboard, which sucked because I love to eat. The only things I could taste were sweets.
People started sending me fruit arrangements. Someone sent me a bunch of cupcakes. I ate a lot of fruit and a lot of desserts. Anything salty didn’t taste like anything really, or it tasted horrible.
My diet was pretty bad because I was eating mostly desserts.
It took a few months for my taste to come back. My last infusion was in December. It wasn’t until the following year that food started to taste good again.
People on forums can scare you. I read something that said, “You’re going to hate the foods that you loved the most after chemo.” Thankfully, everything went back to normal, but I just eat more sweets now.
I don’t want to downplay the treatment and the whole experience, but it wasn’t like life was throwing me anything I couldn’t handle. Everything was kind of doable.

Do you have any advice for someone who’s about to go through chemo?
Take it easy. Don’t set the expectations for yourself so high.
Chemo’s effects can be cumulative. Right after your first session, you might feel great, but fatigue, hair loss, loss of taste. and everything gets worse and worse as you go on.
For me, I overdid it after my first infusion. I was still working out. After my second one, I knew my body was trying to tell me something. I knew I couldn’t pretend that I was still normal. I binged so many shows on Netflix. I just chilled out.
Did you work through chemo?
I went back to work in November in between my last 2 infusions, and my head was shaved. People noticed. obviously. I let my coworkers know that I wouldn’t be able to do things the way I could before.
It took forever for me to walk through the parking lot. I’d get winded going up the steps. Fortunately, they were very understanding. I was very open about my diagnosis, mainly to set the expectations for what I could do.
»MORE: Read more on how others dealt with work after a cancer diagnosis
Reconstruction
What was the process for reconstruction?
I chose immediate reconstruction, but because I didn’t have enough fat and tissue to build the new breasts, they added tissue expanders. My breast surgeon and plastic surgeon had worked together during my mastectomy.
As the breast surgeon was taking out tissue, the plastic surgeon was placing the expanders.
In between chemo infusions, I would go see my plastic surgeon, who would add more fluid into the expanders. It wasn’t painful, but it was definitely very uncomfortable. There was always a numbness or tightness in my chest.
After chemo was over, we had to wait about a month to do the swap from the expanders to the implants to let my body heal.
What was the breast reconstruction surgery like?
After going through the mastectomy, it wasn’t too bad. I was just excited. I told myself, “I’ve gone through cancer so I can get new boobs.”
I don’t remember the recovery time because I was back to work. I might’ve taken 2 days off or something like that.
With everything that I went through, this was almost like a consolation prize.
It’s not that I didn’t like my breasts before this. My husband and I jokingly made a pact years ago. I would only do breast implants if we had a million dollars in our bank account.
It’s such a big expense and it’s unnecessary, so unless we had a million dollars to blow, I was never going to do it. Since cancer was doing this to me, I wanted to do it right and get something out of it.
I’ve heard stories where people just go flat, and that’s not a bad thing at all. Breast implants get recalled sometimes. There was one recently, so I went to my oncologist to check mine out. Luckily, mine aren’t ones that were part of the recall.
Of course, I don’t want my implants to be recalled, but if I do wind up having to go flat, I’ll be okay with it. It really doesn’t define me. It’s just a fun thing to have for me. Add in the fact that I didn’t have to pay thousands of dollars for them. It was something I wanted to do.
What about the nipple reconstruction? How was that?
I wasn’t sure if I wanted the nipple reconstruction or not. Mine had already served their purpose. I already breastfed 2 kids.
I was happy to be able to wear a t-shirt and not having to worry about wearing a bra ever again.
To me, it wasn’t a big deal. I was fine with looking like a mannequin, but I do have a husband.
He thought it looked a little weird. We waited 7 months before doing that reconstruction. I don’t remember why we waited so long, but I did have them done.
The surgeon took part of the skin and recreated the nipple. The reconstruction didn’t take, though, so now I don’t have nipples anyway. The nipples he created are flat now. I don’t know if that’s just my body or what, but I wouldn’t necessarily recommend it.
He spent all that time and I was in surgery, and still no nipples. I was supposed to get the 3D tattoo for nipples, but I had to move, so I’m in the process of finding a new tattoo artist that can do it for me.

Mastectomy tattoo
I don’t have an elaborate tattoo like most people get. That’s only because I want to save room for my nipple tattoos if I do get them, since they’re for my husband. He’s gone through so much, so it’s the least I could do.
When I was deciding to get the mastectomy, I was looking online at all the mastectomy tattoos people had gotten. They’re all so beautiful.
I didn’t want anything that would show too much because I work in a professional setting. I don’t want to have to worry about what to wear to work because of a tattoo showing.
Right after the implants were put in, everything was still so numb. I decided the best time to get a tattoo was when I couldn’t feel it.
I have a love symbol since I’m from Philly. I wanted something to remind me of where I come from. It’s on the left side, which is the side where the cancer was first found.
Instead of the “o,” she put the breast cancer ribbon, but I didn’t want it to be pink. There’s good and bad intentions behind the whole pink thing, so I wanted polka dots instead.
Getting the tattoo was such a breeze. I was mostly excited. It took me a while to find the artist. I wanted it to be a certain style. She’s really feminine and all tatted up.
The polka dot thing was kind of her signature. She does a lot of 50s throwback designs.
What does your tattoo mean to you?
It’s cathartic. I survived. I left Philly behind. I left my cancer behind.
It’s a good reminder of where I’ve been and how that doesn’t define who I necessarily have to be.
Survivorship
What’s the ongoing follow-up protocol?
There was never an official remission conversation. My breast surgeon took everything that she could see, and if there were any cells leftover, that’s what the chemo was for.
After the mastectomy, there was technically no evidence of disease. I haven’t had any scans in a while.
I’m on tamoxifen. I do blood work rarely. For now, I just go see my oncologist every once in a while.
Sometimes I question how and why my experience was so easy. It’s that sort of thing that makes it so dangerous to compare your experience with others.
What is your “new normal” after cancer?
When I lost my hair, I had a new confidence. I don’t know what it was, but maybe it was the “battle” mentality. I was really confident with my short, buzzed haircut.
That stuck with me for a long time. I don’t get nervous anymore. Public speaking used to bring me to tears, but now I’m good.
When my job told me I had to move from Philly to Atlanta, I thought it was no big deal.
It’s almost like the opposite of the story of Samson. When they cut his hair, he lost his power, right? When I cut my hair, I felt like I gained so much power.
I was in Georgetown like 2 weeks after my surgery, around Valentine’s Day. I was walking in a parking lot to my car after dinner with a girlfriend.
It was 10:00 p.m. in D.C., so the place was buzzing. I saw this guy walking towards me. It was a cold day, so he had a winter cap on. I turned around, and he was right next to me.
He kept my door open, and he had a gun in my face. I started to scream. It was like, ‘I’ve gone through cancer, and you’re going to try to take my life with a gun? No way this is going to happen.’
I just kept screaming. There’s so many people in that area, so I guess he got scared and took off. There’s no way that I would give up now. If I hadn’t gone through cancer, I don’t think I would’ve acted the same way.
I think I would’ve been too scared and mild to do anything. Instead, I was like, “Screw this guy! Who does he think he is?”
My hair gave me a sense of confidence.
What was the lowest point you had?
It was when I was told I was told I would be moving for my job right before reconstruction. That was the scariest thing for me because I had to leave my medical team behind.
I really owe my life to them. This is probably a daily thing for them, but I really attribute where I am to how they dealt with everything.
They were very caring and professional. I didn’t feel like I was a number. I felt our interactions were very individual. They all made it feel like they were very committed to me.
I was not ready to leave them. I saw them so often. When I had to leave, it was like breaking up. That was my lowest point.
How did the cancer affect your relationship?
This is probably bad, but I didn’t really put any focus on our relationship because I didn’t feel like I had time to deal with anything else. I just needed to focus on getting better.
Once I was better, I knew I could be in the relationship again. I needed to focus on that to be present in the long-term. Our relationship took a break.
We couldn’t be intimate because I was going through a bunch of medical procedures. This is where “for better or worse” comes into the picture. He stuck around, and here we are on the other side.
There wasn’t any question or doubt in my mind that he was going to be there. It was expected. I knew he would be here.

I was sleeping in the project room and not in the bed with him, because I didn’t want to leak all over everything. Maybe I put way too much faith in our relationship, but here we are.
He never gives me any doubt. We’re committed, and if the roles were reversed, I would do the same thing. I wouldn’t say that cancer made us stronger, because we were already strong to begin with.
He’s the typical old school guy. He doesn’t see the need to seek professional help. I kept telling him, “I think you might have some PTSD. Maybe we should go see someone.”
Everyone is different. I can’t force him, but so far he’s still okay. I guess maybe he doesn’t need therapy right now, but maybe down the road he will. I don’t want him to go through any depression or anxiety.
Now that I’m healthy again, we have the rest of our lives, so I want both of us to be in a good mindset and be okay.
Any advice for married cancer patients?
Appreciate your significant other. Appreciate the people around you. My husband could have left. My kids could’ve had mental breakdowns. Appreciate the people that stick around you.
I didn’t see anyone leave, but appreciate the things that they go through. I was physically the one going through it, but they were going through it in their own way. They came out the other side.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
How did your kids handle the diagnosis?
When I told my daughter, all I knew was that I had a lump and the doctor wanted to see me immediately. I didn’t know my stage. I didn’t even have the official diagnosis, but I had a feeling. I knew that wasn’t good news.
I’m all about transparency. My kids were old enough to see and understand.
It might’ve been different if they had been younger, but I didn’t want to paint a picture that everything was just totally fine and normal. That’s why I let myself be vulnerable that first phone call when I cried.
As long as my kids knew what to expect beforehand, it was okay. We didn’t make anything a huge deal.
We didn’t freak out about me being home or losing my hair. They were in the bathroom when I shaved my head. We were trying to show them that this was just a part of life.
I think we maybe downplayed it too much. They don’t think it’s a big deal. Even if I tell them now that I have to see my oncologist, they’re just like, “Yeah, okay,” and shrug it off.
I joke around with them and say things like, “Wait, you don’t want to give me a hug? I had cancer!”
»MORE: Parents describe how they handled cancer with their kids
How was the financial aspect of treatment?
We’re still dealing with the financial side of things. We have a higher deductible, but it covers 80% of everything. Once you max out the deductible, everything is covered.
I think my deductible is about $6,000. That’s what we’re dealing with now. Every year, we max out because of one thing or another, so that’s something we just have to plan for.
We’re in a good enough financial place, though, that it was never really a big stress for us. If you could pick one perfect person to go through what I went through, it would be me.
Financially, we could handle it. My body could handle it because I was young and healthy. Mentally and emotionally, I could handle it.
This is where I do think that Obamacare is a wonderful thing. I don’t want to get too political, but health care should not be a choice. It is a right.
You shouldn’t have to be stressed out about how you can pay your bills because you’re insurance won’t cover. That’s such a foreign concept. I really wish that everyone could have the ability to go through this the way I did if they’re going to have to go through it.
Finances should be the least of your worries when you’re fighting cancer. You don’t want money to be impacting your treatment decisions.
Do you have any advice for someone who has just been diagnosed?
Every cancer is different. You need to make your own decisions based off of what is right for you. There is no right or wrong. Just be confident in your decisions. Don’t look back.
Hair Loss
You buzzed your hair and then shaved it
One of the first things the oncologist told me was that my hair was definitely going to fall out.
I had the option of doing cold caps, but it’s like $2,000, and you’re always cold. I hate being cold. I just decided to be fine with losing my hair.
Before my first infusion, I went to a hair salon and got a really short haircut just to test it out. Then we did the first chemo. I could feel hair starting to come out.
I would run my hand through my hair, and clumps were coming out. I didn’t want to experience that for real because it was kind of unnerving, so I buzzed it.
It was around my second infusion that I shaved my head. Even with the buzzed haircut, it was coming out so much.

I didn’t want it to be traumatizing for everyone. I didn’t want to see hair on my pillow case, and I didn’t want my kids to see hairs everywhere.
It was liberating to get rid of it. It was a reminder of the bad things that chemo was doing to my body. It was like I was being proactive and doing it first.
Right before my last chemo session, I knew I was never going to have a bald head again, so I got a henna tattoo over my whole head. That was a really cool experience.
Did you like having short hair?
I knew I was never going to have short hair again, so I was kind of excited to try a bunch of different short styles. My husband was really happy, too, because he’s always wanted me to have a pixie cut.

I was taking advantage of that. I didn’t want to focus on the negative things. I still don’t. I want to focus on the positive, because that’s something I can control. I can control my attitude.
Do you have any advice on how to deal with the hair loss?
Embrace it. It’s going to happen. Even with the cold caps, it still can thin out. Everyone is different, but after you accept your circumstances, you’re in a better place to tackle it.
If life is dealing you these cards, you have to accept it. I only have so much energy. I’d rather spend that thinking positive thoughts.

Inspired by Amelia's story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy




