The Latest in Myelofibrosis
Understanding Promising Treatment Options
Edited by:
Katrina Villareal
TRANSFORM-1 Trial
MANIFEST-2 Trial
FREEDOM-2 Trial
XPORT Trial
Treatments to Help with Anemia
Other Treatments Being Studied
DALIAH Study
Calreticulin
The Use of Artificial Intelligence in MPNs
Following the American Society of Hematology Annual Meeting (ASH), Dr. Raajit Rampal of Memorial Sloan Kettering Cancer Center, Dr. Gabriela Hobbs of Mass General Cancer Center, and patient advocate Ruth Fein explore new treatment options.
Learn about success stories, dispel myths about experimental drugs, and understand the broader impact of trial participation on advancing MPN treatments.
Find out about the latest options for myelofibrosis patients, how to deal with myelofibrosis symptoms, and how factors like age, mutation status, treatment history, and personal preferences inform your treatment.
Learn about how the latest advancements may affect your care and get updates on exciting news about the pace and progress of myelofibrosis treatments.
The myelofibrosis panelists discuss momelotinib, fedratinib, selinexor, pelabresib, navitoclax, and other myelofibrosis treatments.


Thank you to GSK and Karyopharm for their support of our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Introduction
- Symptoms of Myelofibrosis
- ASH 2023 Updates on Myelofibrosis Treatments
- Treatment Sequencing
- ASH 2023 Updates on Fedratinib
- ASH 2023 Updates on Selinexor
- ASH 2023 Updates on Momelotinib
- Practice-Changing Updates
- Personalizing Myelofibrosis Treatment
- ASH 2023 Updates on Interferon
- Artificial Intelligence in Hematology
- How Patients Can Be More Proactive in Their Treatment
- Conclusion
Introduction
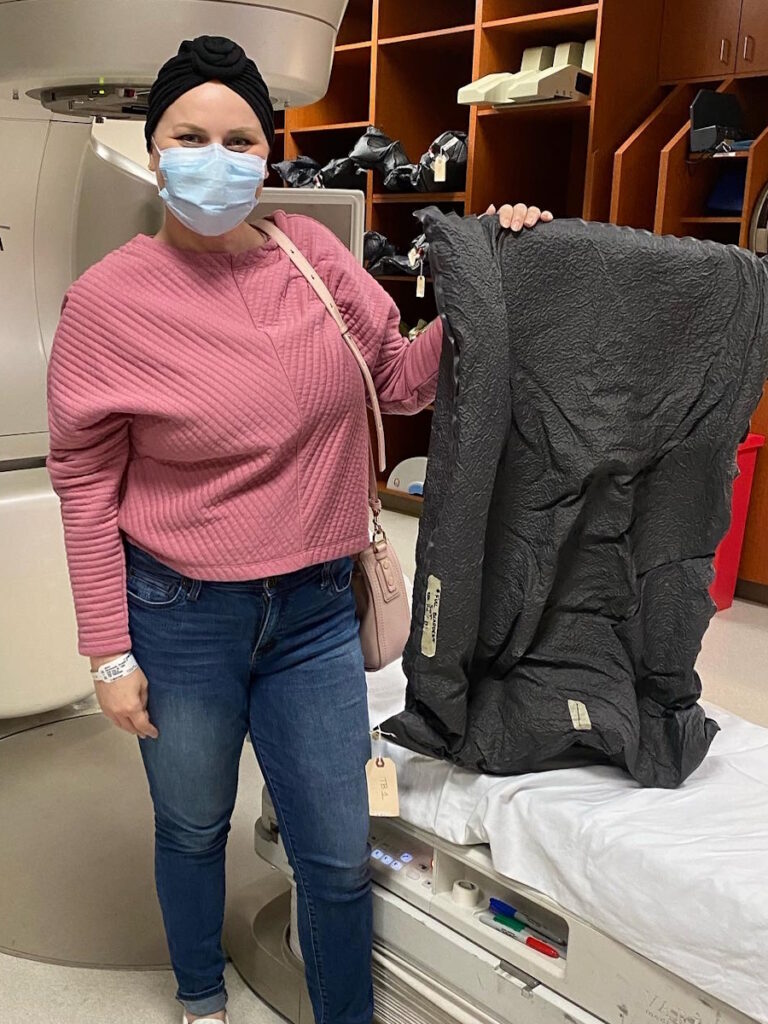
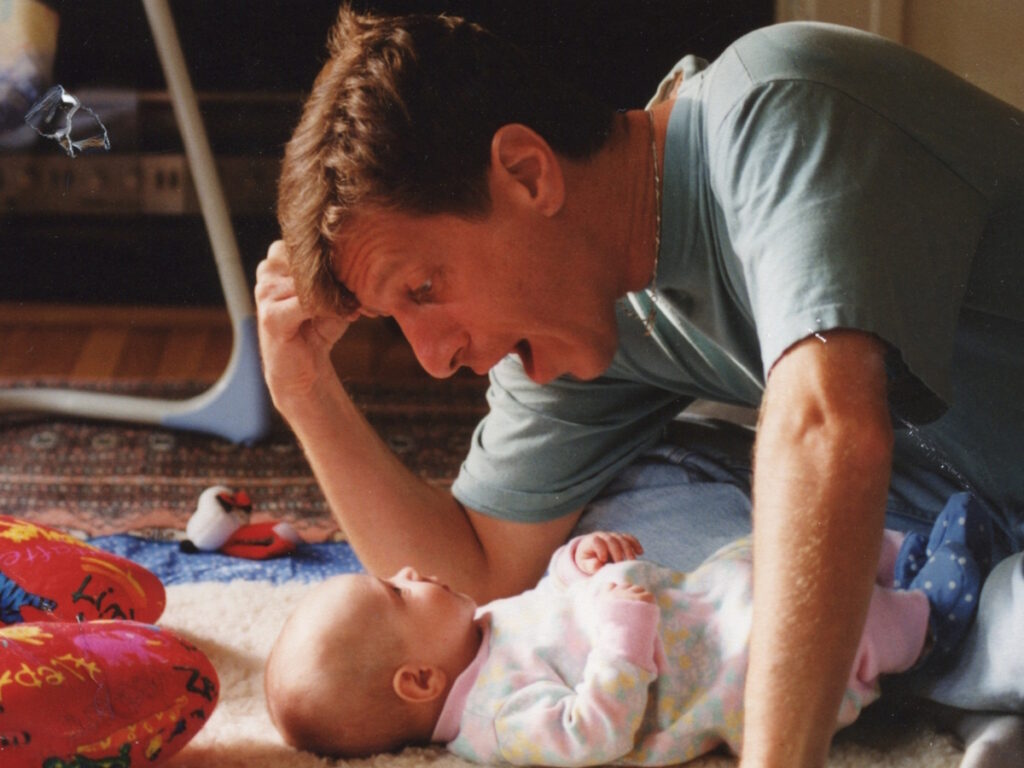
Stephanie Chuang, The Patient Story Founder
Stephanie Chuang: I’m the founder of The Patient Story and, more importantly, I also got a blood cancer diagnosis of non-Hodgkin lymphoma a few years ago.
We have so many shared experiences in what we’re looking for and that’s what The Patient Story is all about.
We try to help patients and care partners navigate a cancer diagnosis primarily through in-depth conversations with patients, care partners, and top cancer specialists, like the ones you’ll hear from today.
I want to give special thanks to GSK and Karyopharm for supporting our educational program. Their support helps programs like this more available and free for our audience. But we do want to note The Patient Story retains full editorial control of this entire program. A quick reminder that this is not meant to be a substitute for medical advice.
Our patient moderator is Ruth Fein Revell. Ruth, can you share a little bit more about your story and how you became such a passionate advocate in this space?


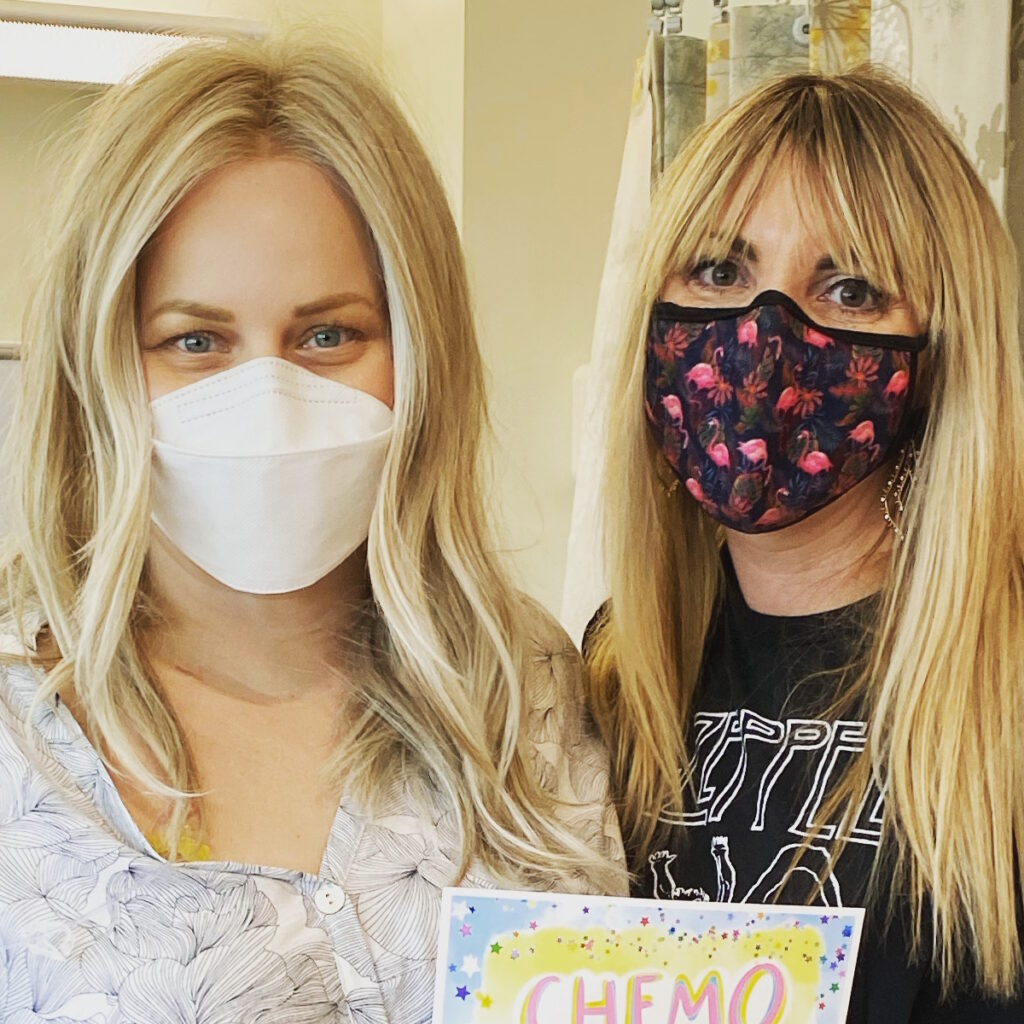
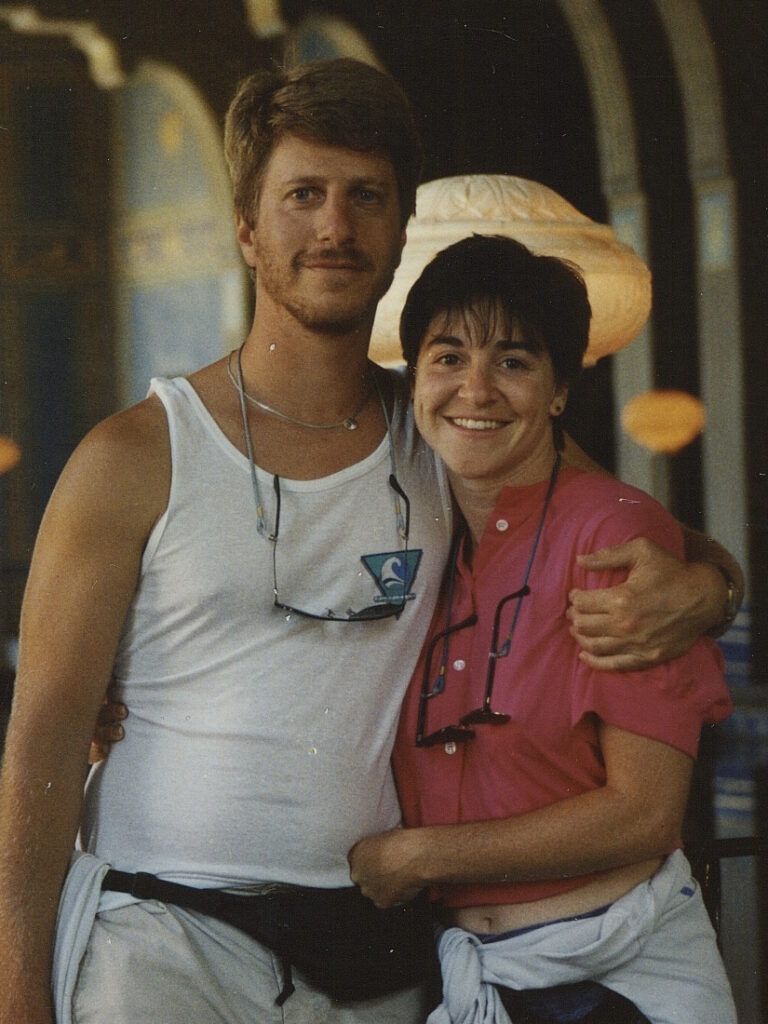
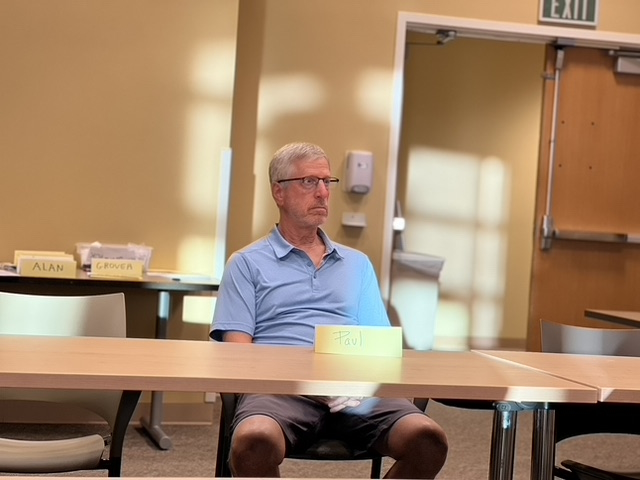
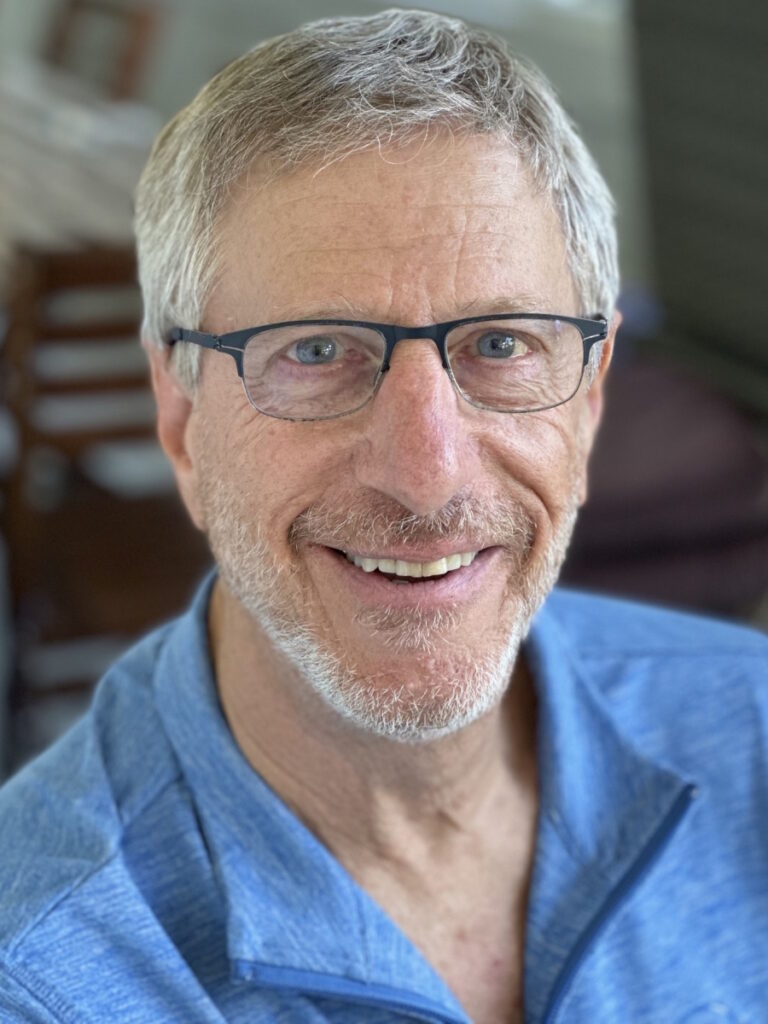
Ruth Fein Revell, MPN Patient Advocate
Ruth Fein Revell: Welcome, and thank you for joining us. I’m Ruth Fein, a health and science writer. I’m also a patient and a patient advocate who’s been living with a myeloproliferative neoplasm of one type or another for almost 30 years.
I was diagnosed with essential thrombocythemia when I was 38 years old and raising two young boys. I had had symptoms for many years, but they were disregarded or misdiagnosed. The most troublesome of which was severe, debilitating headaches with blind spots where I literally couldn’t work for hours at a time. I also had bone pain that I experienced for years.
What started as essential thrombocythemia transitioned to polycythemia vera and then progressed to myelofibrosis, which is where I am now. I’m very fortunate to be on a clinical trial that’s working so well that my life is wonderful. I also recognize that everyone isn’t in the same position as I am as there are a lot of people who suffer greatly from myelofibrosis.
I’m speaking with two world-renowned experts in MPNs, Dr. Raajit Rampal of Memorial Sloan Kettering Cancer Center and Dr. Gabriela Hobbs of Dana-Farber/Harvard Cancer Center. Both of you are very, very involved in the patient community and giving back through your knowledge and also taking time to do interviews like this so thank you for that.
We’ll dig into what’s been reported recently at ASH, the annual meeting of the American Society of Hematology where a lot of reports come out. Some of them are quite exciting.
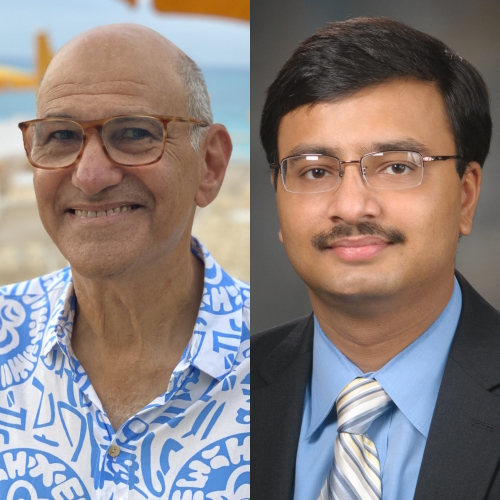
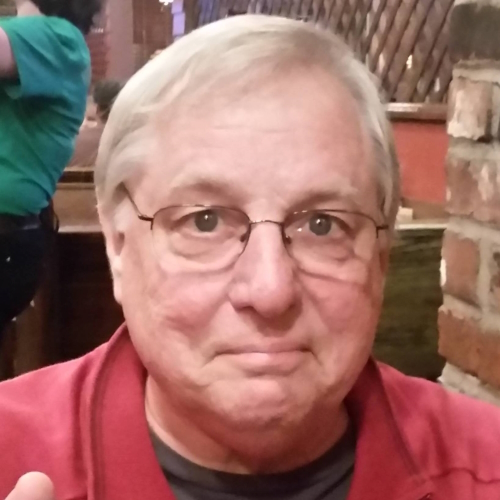
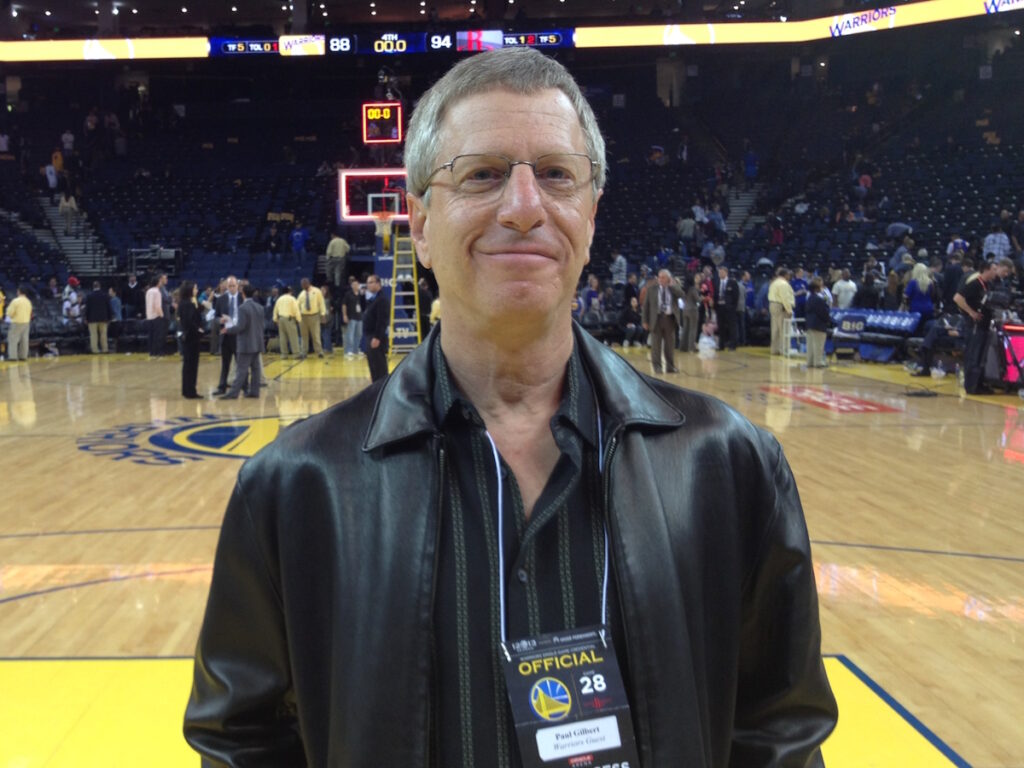
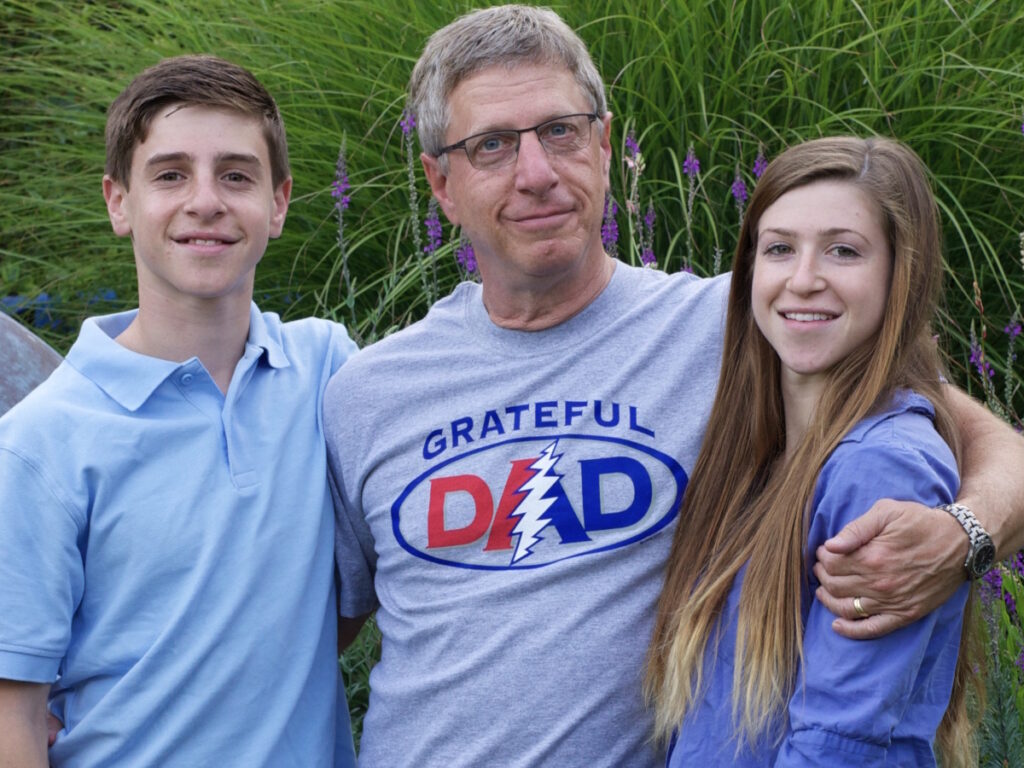
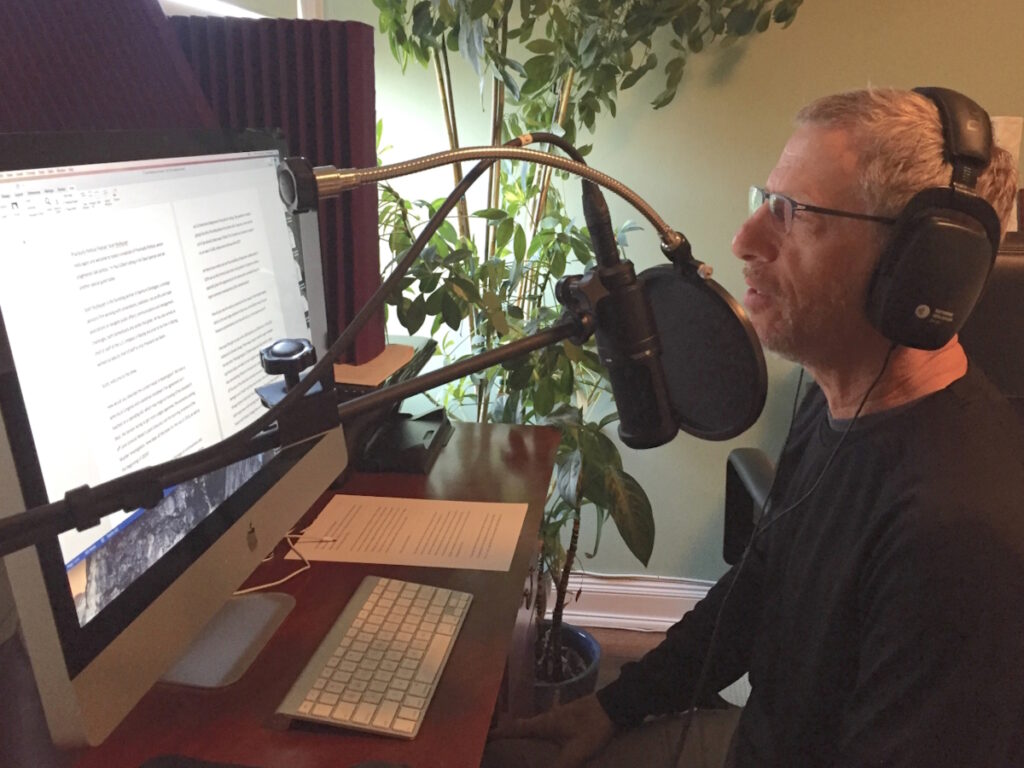
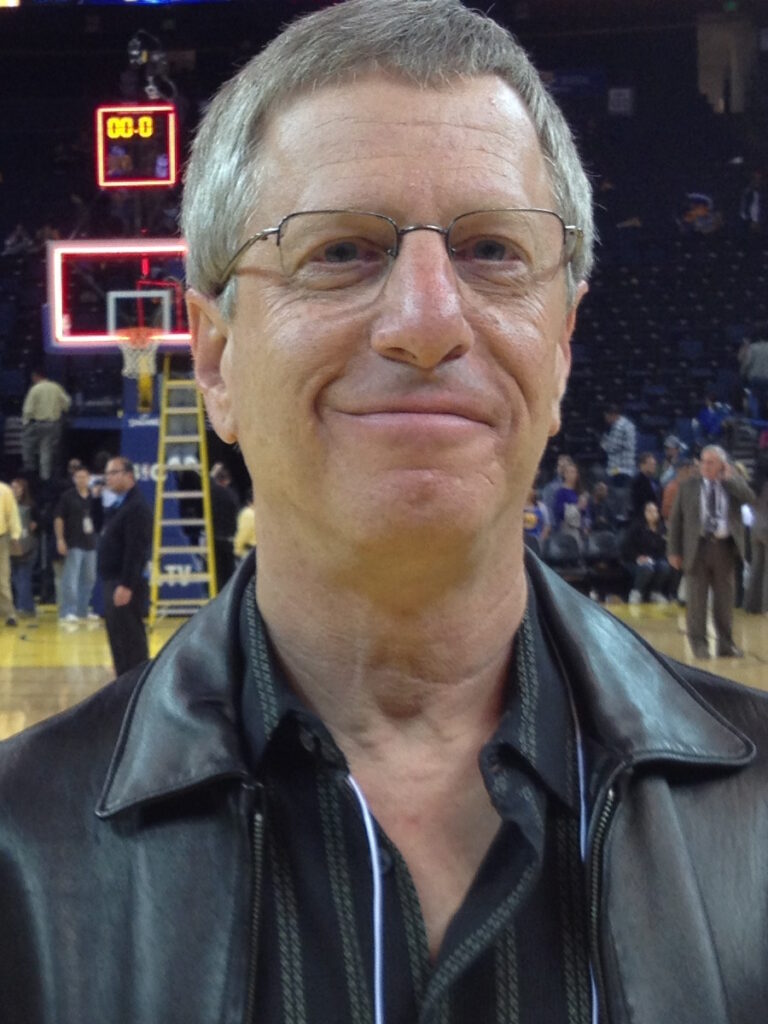
Raajit K. Rampal, MD, PhD
Ruth: Dr. Rampal, give us a little bit of your background, why and how you became interested in MPNs, as well as what your practice looks at.
Dr. Raajit Rampal: I’m a physician-scientist and I lead the MPN program at MSK.
My interest came from the biology side. I’ve been working with Ross Levine for a number of years on the lab side. It became clinically interesting based on what I was learning in the lab so I’ve taken on clinical practice and doing clinical trials for patients in MPN.
This is a field with such an unmet need for effective therapies. Wanting to be at the forefront of that and trying to deliver change where it’s needed have always driven what I want to do. This was the perfect intersection of my scientific and clinical interests.


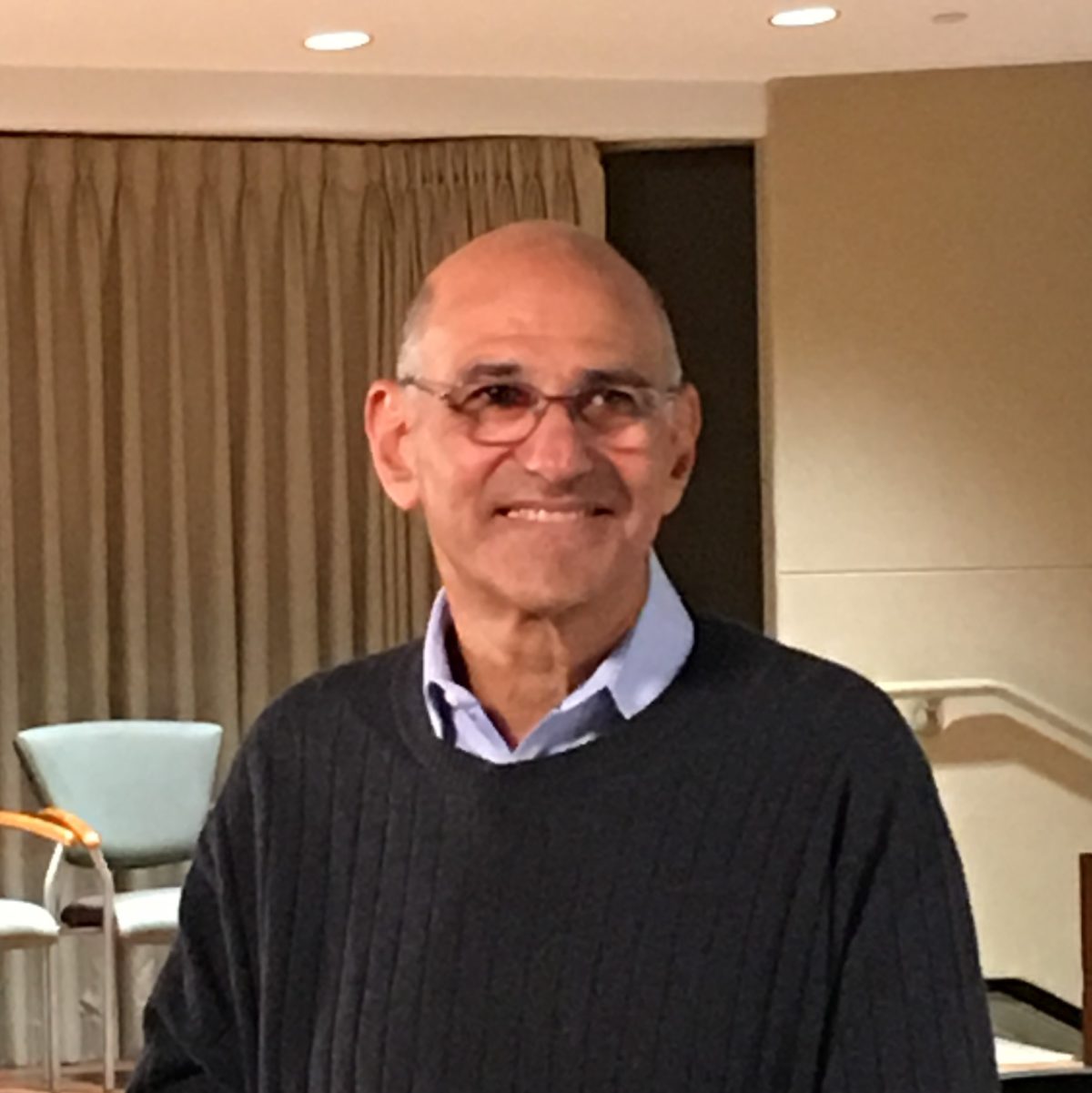
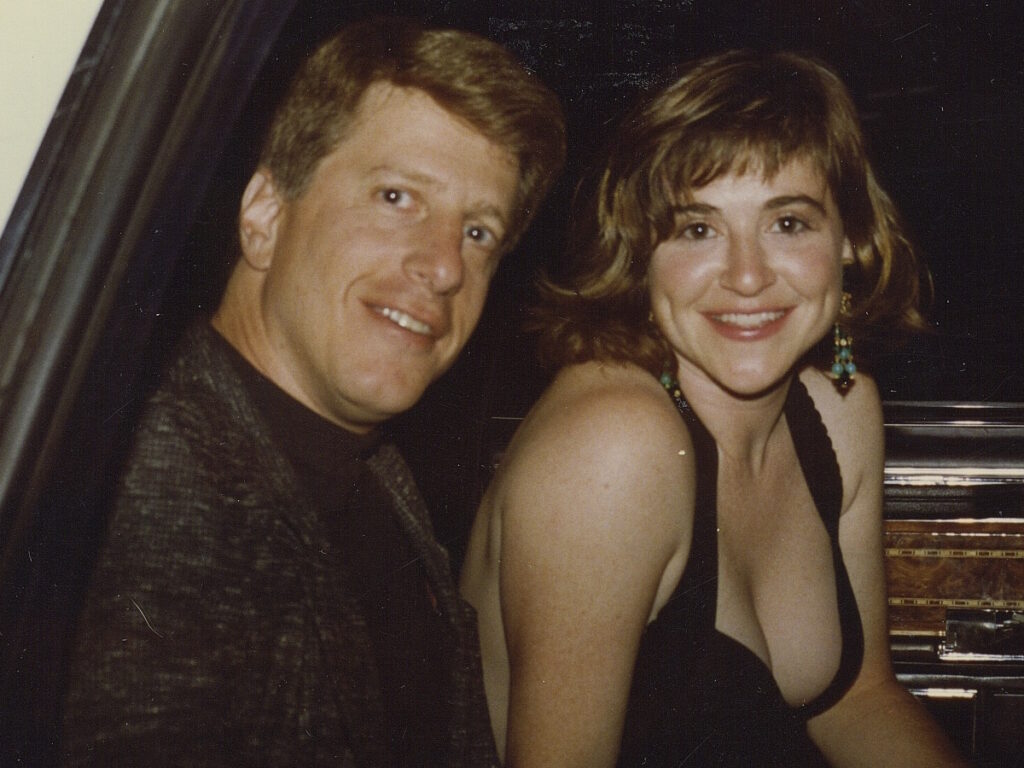
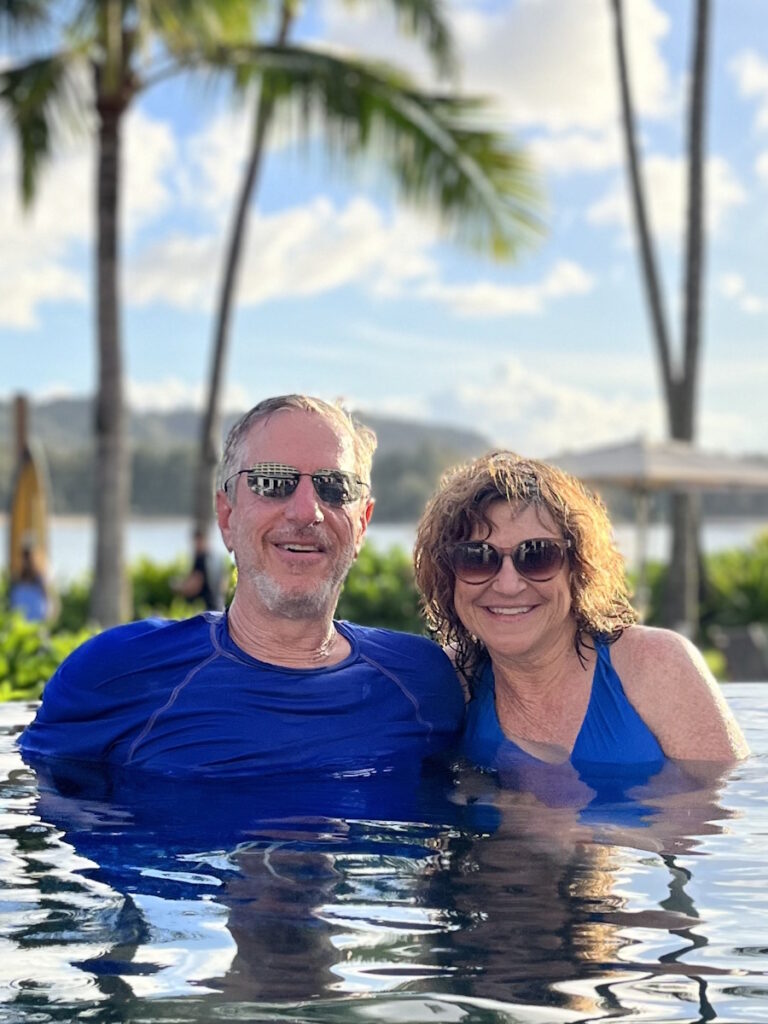
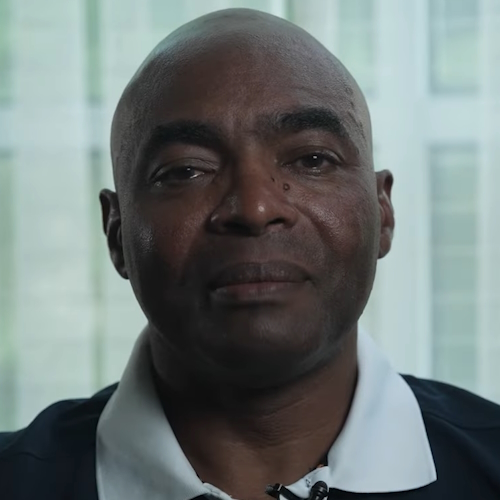
Gabriela S. Hobbs, MD
Ruth: Dr. Hobbs, would you tell us a little bit about yourself and how your interest in MPNs began?
Dr. Gabriela Hobbs: I am the clinical director of the leukemia service as well as the MPN program at Massachusetts General Hospital in Boston. I’ve always been interested in hematology as far as I can remember, and I was very fortunate to do fellowship training with Dr. Rampal.
For me, myeloproliferative neoplasms in particular are such a rewarding group of patients to take care of. It merges everything that I love about being a physician. I can have very longitudinal as well as very intimate patient relationships with the patients whom I take care of. From the clinical perspective, I found taking care of patients incredibly rewarding and also very varied.
From the scientific perspective, when I was an undergraduate student, we started seeing some of these oral-targeted agents being approved and I knew that was something I wanted to be involved in for my career.
Being a clinical investigator who’s able to see clinicians like Raajit Rampal doing investigations in the lab, finding new targets and new drugs, and being the person who helps take that to clinical trials to the patients is incredibly rewarding.
The most common symptom of patients with myelofibrosis is fatigue, which is probably one of the reasons why myelofibrosis and the other MPNs sometimes take a while to get diagnosed.
Dr. Gabriela Hobbs
Symptoms of Myelofibrosis
Ruth: Myelofibrosis is rare. Some practitioners don’t see very many MF patients. Some patients who are diagnosed with myelofibrosis don’t have enough information or are misguided at times. What do you each see as the major symptoms of myelofibrosis?
Dr. Hobbs: Myelofibrosis is a disease that can present in many different ways. I certainly see completely asymptomatic patients. Their doctor noticed that they had some abnormalities in their blood counts or maybe the patient themself noted that their abdomen felt a little bit different. Patients are on the spectrum of either not having a lot of symptoms or having lots and lots of symptoms.
I would say the most common symptom of patients with myelofibrosis is fatigue, which is probably one of the reasons why myelofibrosis and the other MPNs sometimes take a while to get diagnosed. Other symptoms that we see a lot of are itching, night sweats, fevers, and unintentional weight loss.
Dr. Rampal: Part of the challenge is whether those symptoms are communicated in visits with physicians. Part of that involves us asking the right questions or, at least, training our colleagues to ask the right questions because not everybody is forthcoming about their symptoms. The alternative is that they get so used to their symptoms that it’s the new normal for them and that is sometimes the tougher part of trying to understand how somebody is doing.
Dr. Hobbs: Occasionally, there may be some patients who feel like there are certain symptoms that they wouldn’t bring up to an oncologist. When I meet a patient for the first time and go down my checklist of MPN symptoms, I’ll ask them about itching and they’d say, “How did you know?” We’re fortunate in the MPN world to have these forms that have been validated to help us ask about symptoms that we know are very common in patients with MPN so that we don’t miss anything.
There’s a whole spectrum of symptoms patients can experience.
Dr. Raajit Rampal
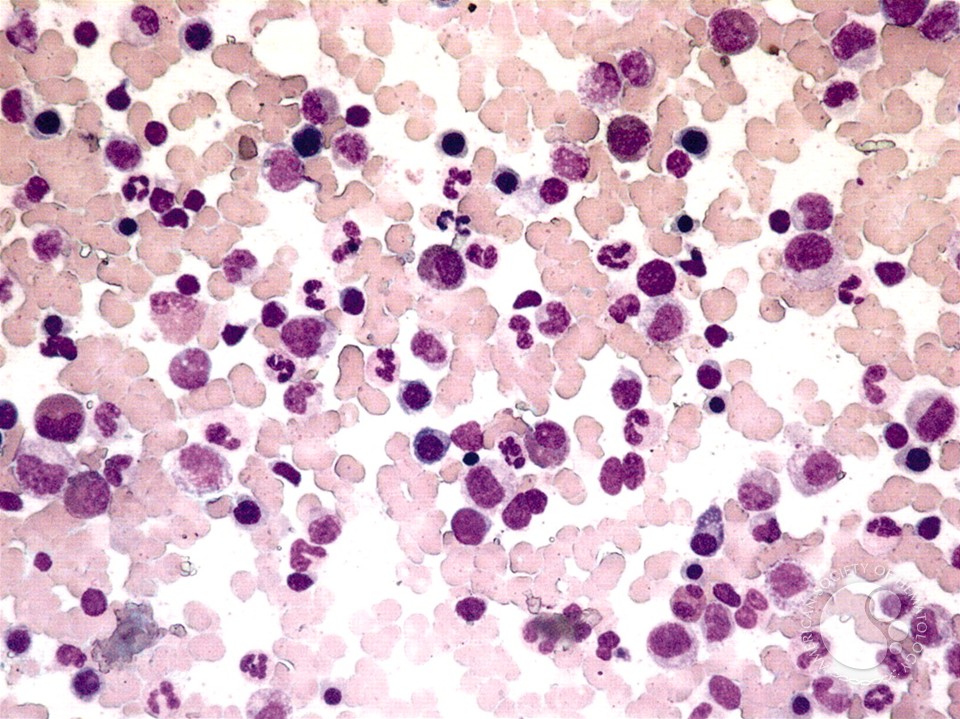
Dr. Rampal: Myelofibrosis is a disease of the bone marrow where you have mutated cells that start to grow and take over the bone marrow. They cause inflammation and we think the inflammation causes scarring in the bone marrow. As that happens, the bone marrow starts to contract and is unable to make blood cells. Blood cells start to go into the liver and the spleen to try to produce blood so those organs get larger and cause symptoms.
The inflammation that causes the scarring and damage in the bone marrow also causes people to have symptoms. Those include getting fatigued, losing weight unexpectedly, and having bone pain and aches. There’s a whole spectrum of symptoms patients can experience, but those are among the most common.
That’s how we think about myelofibrosis and how we think about the disease getting worse. We look at blood counts. If people’s blood counts are getting worse, that’s a sign of disease progression. If their spleens or livers are getting larger or they’re feeling worse, all of those are signs of the disease progressing.
There were two phase 3 studies presented about myelofibrosis, the navitoclax and pelabresib studies.
Dr. Gabriela Hobbs
ASH 2023 Updates on Myelofibrosis Treatments
Ruth: We all know there’s been such an explosion in advances in myelofibrosis in recent years. Dr. Hobbs, what came out of ASH 2023 that you’re most excited about?
Dr. Hobbs: It’s exciting. I can’t remember participating in an ASH conference where there were two phase 3 studies presented about myelofibrosis, the navitoclax and pelabresib studies. That in and of itself was a reflection of how far the field has come. We’re now presenting phase 3 studies on drugs that may get approved.
Dr. Rampal: I totally agree. When have we had two phase 3 studies read out? I can’t remember if that’s ever even been the case simultaneously. Thinking about this in the context of our patient audience, this is a clear sign of progress in the field.
Let’s separate that idea from what happens from a regulatory standpoint. You have to get to this point. This is where the finish line is. It is incredibly encouraging that we’ve got drugs to this point of phase 3 where we may have definitive results that could lead to approvals.
What we can probably say, at least with both drugs, is that they have activity in the disease. There’s no question. What happens from here, of course, is up to the FDA. But I’m encouraged by this. I think these drugs have the potential to make a difference for patients so this is exciting.
The combination (ruxolitinib and navitoclax) led to a very dramatic improvement in spleen volume reduction in patients compared to patients who were treated with ruxolitinib alone.
Dr. Gabriela Hobbs
Dr. Hobbs: Both of these studies were phase 3 studies, as Dr. Rampal mentioned. The navitoclax study was the TRANSFORM study that compared ruxolitinib alone to ruxolitinib and navitoclax. They wanted to see if the combination of the two drugs was more effective at improving spleen volume response as well as improving the symptoms of myelofibrosis patients.
They found that the combination led to a very dramatic improvement in spleen volume reduction in patients compared to patients who were treated with ruxolitinib alone. The symptom endpoint was more difficult, as it seemed like symptom improvement was similar with the combination of navitoclax and ruxolitinib compared to ruxolitinib alone.
My take on that is it’s not entirely surprising that a drug like navitoclax would not improve the symptoms, but it certainly didn’t make patients feel worse. I think that’s important when you think about combination therapy as well. I wouldn’t consider that an entirely negative endpoint.
Why should patients care about how big the spleen is and how much it shrinks? That is one of the few things we know that correlates with survival.
Dr. Raajit Rampal
Dr. Rampal: Let me build off of something that Dr. Hobbs said. Symptoms are important to patients and that has to be part of any of our treatment arsenals. But as you said, we want to get drugs that alter the trajectory of the disease and not simply focus on symptom reduction. That has to be part of the conversation going forward as we think about new drugs in this space.
How much weight do we put on symptom reduction as something that we, as a community or the FDA, should fixate on? As long as the drug is not making people feel worse, if it’s doing other things for patients, then maybe that’s where the win is if you will.
About pelabresib, this is a study of the combination of pelabresib, which is a BET inhibitor, plus ruxolitinib versus ruxolitinib alone. The study looked at whether patients had a greater degree of spleen shrinkage with the combination or ruxolitinib alone.
The answer was unequivocally yes. Patients who got the combination had a much greater spleen response, 65% versus 30%.
Why is that important? Why should patients care about how big the spleen is and how much it shrinks? That is one of the few things we know that correlates with survival. We’ve known from the time of ruxolitinib. Spleen shrinkage correlates with overall survival, which is something we all care about deeply.
There was a trend toward the symptoms getting better with the combination. It wasn’t quite statistically significant, but it was certainly a trend that favored the combination.
Importantly, it didn’t add toxicity. We didn’t see that there were any new major signs of toxicity with the two drugs versus one. In oncology, we worry about that all the time. If you add another drug, you may add toxicity, but that wasn’t the case here. From that standpoint, I’m very encouraged by both data sets.
A big takeaway from having all these drugs is that we shouldn’t wait for people to get that sick. We should treat earlier on.
Dr. Raajit Rampal
Treatment Sequencing
Ruth: Dr. Rampal, as we talk about more options available both today and in the future, one of the things that comes up often, especially for higher-risk MF, is sequencing. What are we learning about optimizing the new drugs and combination drug therapies, including determining when and how to switch therapies?
Dr. Rampal: The answer is we don’t know. The broader context of this is that we have more options so that has two implications.
Historically, there’s been a reluctance to start therapy because you didn’t have anything else. If you were in a world where there was only ruxolitinib and it stopped working, what were you going to do? That’s not true anymore.
A big takeaway from having all these drugs is that we shouldn’t wait for people to get that sick. We should treat earlier on. What is earlier on? There’s some ambiguity there, but I think that is one of the implications of having a lot more drugs.
The reality is we’re going to learn how to use these drugs as we go along. There isn’t a great deal of data. We have data on switching from ruxolitinib to fedratinib. We know what happens and how people do when you do that, but do we have data for the other drugs?
If we start going from momelotinib to ruxolitinib, we don’t have the granular data for that. Those are things we’re going to figure out in practice, probably over the next 1 to 2 years, I’d say.
Now that we have four approved JAK inhibitors, there’s no reason to feel like somebody needs to wait for symptoms from their spleen or their disease.
Dr. Gabriela Hobbs
Dr. Hobbs: The point that Dr. Rampal made is so important, especially when we think about what he said about one of the things that we know in myelofibrosis, which is a smaller spleen equals better outcomes.
An important message for patients is exactly what Dr. Rampal said. Now that we have four approved JAK inhibitors, there’s no reason to feel like somebody needs to wait for symptoms from their spleen or their disease because we do have a lot of options.
Now that we have a lot of options, it became a situation where all of us are calling each other and asking, “How do you switch from this one to the other? Have you had a good experience?”
Sometimes, the clinical trials don’t necessarily translate to what we do in clinical practice. Many clinical trials require that patients be completely off of a JAK inhibitor before they switch to the other, which is something that, in practice, probably neither of us would ever really feel like doing. Over the next year, it’s something that we’re going to have some publications about to help guide the broader community to do that safely.
What these data have shown with the FREEDOM trials is that you can better manage gastrointestinal toxicity and that it does get better over time.
Dr. Raajit Rampal
ASH 2023 Updates on Fedratinib
Ruth: Dr. Rampal, what did we learn about fedratinib at ASH 2023?
Dr. Rampal: The most updated data was the FREEDOM2 study, which looked at fedratinib in patients who have been on ruxolitinib. There were earlier trials that looked at the same question, like the JAKARTA2 trial.
When fedratinib was being studied early on, it was seen that there was a lot of gastrointestinal toxicity, like nausea, vomiting, and diarrhea, which was experienced by the majority of patients.
There have been two subsequent trials with fedratinib, the FREEDOM trials, where they aggressively tried to manage the symptoms from the get-go. They didn’t wait for people to get sick or have nausea or diarrhea. When they prescribe the drug, they say, “When you start the drug, if you start to feel nausea, you’re going to take this medication or if any diarrhea starts, you’re going to take this medication.” You don’t let these symptoms get out of control.
What these data have shown with the FREEDOM trials is that you can better manage gastrointestinal toxicity and that it does get better over time. Is that still a side effect that we have to be concerned about? Yes, but it is something that we can manage in most cases if we’re aggressive about doing that upfront and the expectation is that it will get better over time.
The data (on selinexor) is still in earlier stages so I’m waiting to see if this agent is well-tolerated by patients.
Dr. Gabriela Hobbs
ASH 2023 Updates on Selinexor
Ruth: Dr. Hobbs, what about selinexor?
Dr. Hobbs: Selinexor has been interesting as well. This is a newer agent that we’ve started to see some preliminary results on and they presented their data also in combination with ruxolitinib. This agent seems to have very impressive responses in terms of shrinking the spleen and improving symptoms as well.
The data is still in earlier stages so I’m waiting to see if this agent is well-tolerated by patients. We’ll have to see how the later studies will pan out, but it’s still exciting.
Having this fourth agent will be very helpful in the management of patients with MF, especially patients who have anemia and aren’t able to get a bone marrow transplant.
Dr. Gabriela Hobbs
ASH 2023 Updates on Momelotinib
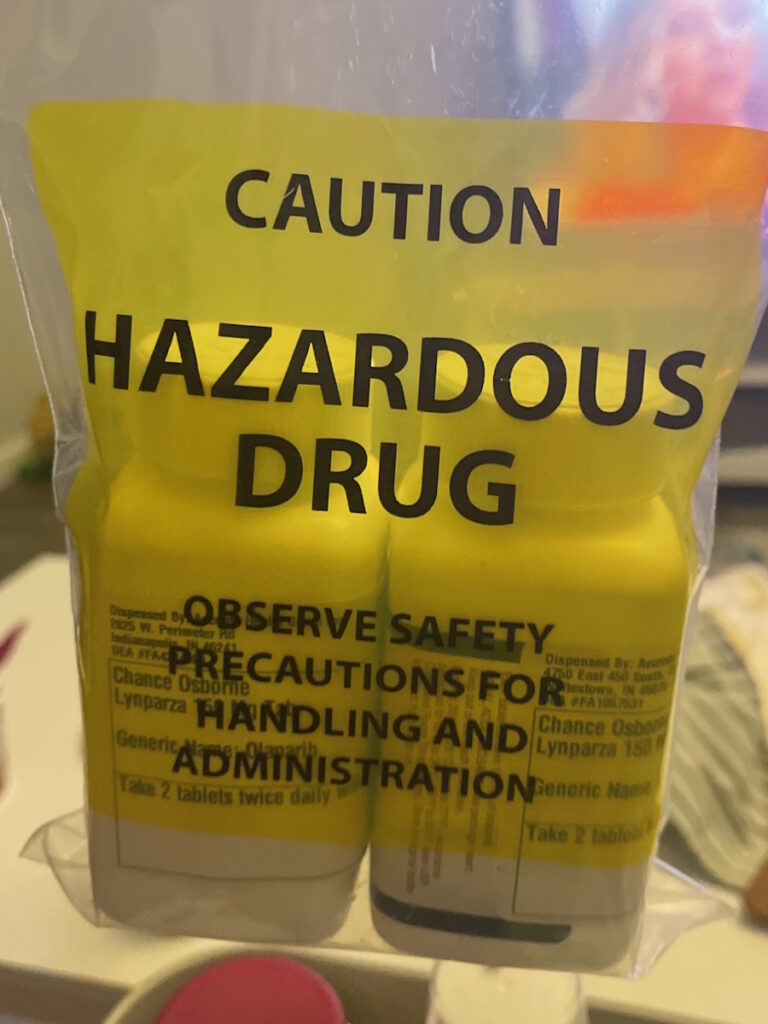
Ruth: There’s an unmet need for the treatment of anemia for patients with MPN, specifically myelofibrosis, which brings us to momelotinib and a few others.
Dr. Hobbs: We’ve mentioned that there are now four JAK inhibitors that are approved for the treatment of myelofibrosis. We have pacritinib, ruxolitinib, fedratinib, and momelotinib, which was approved at the end of September 2023.
Momelotinib is a JAK inhibitor that was approved a little bit differently than the others. Its main indication is for patients who have myelofibrosis and anemia. Anemia has been an unmet need in the management of myelofibrosis so it’s exciting to have a drug like momelotinib that can help anemia and also a drug like pacritinib that can also help anemia in a subset of patients.
In my practice, I’ve noticed that since the approval of this agent, there have been many patients, especially those who are active online, in their communities, and in patient advocacy organizations, who have been excited or eager to switch to this medication.
I do think that having this fourth agent will be very helpful in the management of patients with MF, especially patients who have anemia and aren’t able to get a bone marrow transplant.
When we have patients with myelofibrosis who have anemia, it’s important to consider if a bone marrow transplant is the right therapy. But for those who can’t receive that therapy, momelotinib takes care of a lot of the parts of the disease that we worry about, like the symptoms, the spleen, and the low red blood cell numbers.
In some cases, they take patients who are relying on transfusions and convert them to not needing a transfusion, which is important in terms of survival.
Dr. Raajit Rampal
Dr. Rampal: There is so much going on in anemia in this disease, it’s remarkable. It’s a problem for which we had no good solutions until very recently.
As you mentioned, momelotinib and pacritinib also seem to have an effect in a proportion of patients where they can increase the hemoglobin. In some cases, they take patients who are relying on transfusions and convert them to not needing a transfusion, which is important in terms of survival.
We know that that correlates with survival, but it’s also quality of life. If you have a patient who’s getting stuck in the transfusion chair for 4 to 6 hours a week or more and that is no longer an issue, that is immensely important to their quality of life. It’s an important problem.
There are some other drugs in development and that includes a drug called luspatercept, which is FDA-approved for myelodysplastic syndrome. There are also some other drugs from a few other companies that are anemia-specific and there was some data presented at ASH on them. There are early signs of efficacy. Too early to say anything definitively, but at least it looks like these are drugs that will be studied further.
What’s been practice-changing is having the approval of the last JAK inhibitor, which is momelotinib.
Dr. Gabriela Hobbs
Practice-Changing Updates
Ruth: We talked about what’s happened in the lab, what’s in the drug approval process, what’s recently been approved, and where our needs still are. What came out of ASH that you think is truly practice-changing immediately or in the near future?
Dr. Hobbs: What was very exciting was seeing the two phase 3 studies. Although those two drugs, pelabresib and navitoclax, are still not approved, they are potentially closer to our doorstep and something that we will have to have conversations about how to use.
Do we use them in combination with the JAK inhibitor that they were studied with? Do we use them with other JAK inhibitors? How do we think about sequencing when we’re talking about combination? Although neither of these agents is approved, these are questions that need to be discussed.
What’s been practice-changing is having the approval of the last JAK inhibitor, which is momelotinib. We now have four drugs that we can prescribe to our patients when we see them in the clinic, especially those who have anemia.
There are so many drugs coming down the pipeline and showing interesting activity, especially some of those showing activity by themselves.
Dr. Gabriela Hobbs
Personalizing Myelofibrosis Treatment
Ruth: The drugs and the studies we’ve talked about are all very exciting, but what other treatments are you excited to share with patients to help you personalize treatment?
Dr. Hobbs: We’ve discussed the MANIFEST and TRANSFORM studies looking at combination studies in phase 3. There are so many drugs that are being evaluated and it’s been very exciting to be at an ASH where we hear about so many different mechanisms of action being explored. Many of those are by themselves and some of them are now getting to the point where they’re used in combination.
To mention a few, there was a compound called a PIM1 kinase inhibitor, another one that inhibits lysyl oxidase, which is a group of enzymes that have to do with making fibrosis or scarring happen in the bone marrow, and an LSD1 inhibitor called bomedemstat.
There are so many drugs coming down the pipeline and showing interesting activity, especially some of those showing activity by themselves. Generally speaking, when we have new drugs that are not JAK inhibitors used by themselves, we rarely see a lot of clinical activity so I thought that that was exciting.
Individualized medicine is the holy grail and there’s a lot of different ways to think about it. There’s how we use the drugs we have now and what some of the newer drugs may be able to do for us.
Dr. Raajit Rampal
Dr. Rampal: There is this whole pipeline of things coming forward, which is amazing for this field. We spent some time talking about the top-line phase 3. But as Dr. Hobbs mentioned, there are all of these drugs that are in early development that are showing us that they may be able to do something. Even beyond what we have, some things are part of the big picture here.
Individualized medicine is the holy grail and there’s a lot of different ways to think about it. There’s how we use the drugs we have now and what some of the newer drugs may be able to do for us.
A key example of this is calreticulin. There’s been a focus on this. There are drugs in investigation that are specific antibodies that target calreticulin. That could be a game-changer if those things work. Pre-clinically, there’s good rationale. Imagine a future where if those drugs are effective, then for calreticulin-mutant patients, this is what we use. We have a drug that targets your mutation. That is where we want to be.
Of course, other mutations occur in the disease and we’ve already started trying to do personalized medicine for patients. Some patients have an IDH mutation that occurs typically in people with more advanced diseases.
We’ve completed a trial where we used a JAK inhibitor plus an IDH inhibitor. IDH inhibitors are FDA-approved for people with leukemia and we’ve combined those drugs and seen very good results. That’s an example of genetically-informed personalized medicine, but there’s also how you use the drugs we have in practice.
Dr. Hobbs: We’ve mentioned a few times that we have four different JAK inhibitors and it’s important to know which patients those are going to help. Are there certain situations where we should use one JAK inhibitor versus another?
At ASH 2023, we saw an update on a similar study that was published recently by the folks who looked at pacritinib. They found that patients who have a symptom improvement of greater than 10% had an improvement in survival, which is similar to what they showed recently with patients on pacritinib having a survival benefit if they also had a spleen volume reduction.
Again, that goes to the theme that we were saying. It’s important to use these drugs and make sure that those drugs are doing what they’re supposed to be doing for the patient. We have endpoints that help patients not only to live better but hopefully to live longer. That can also help the practicing doctor to say this drug is not meeting those endpoints. It’s not helping my patient have an improvement in their spleen or their symptoms. We have other drugs that we should we should think about switching to.
One of the areas where there’s a lot of interest is looking at pre-fibrotic myelofibrosis or early myelofibrosis to see if we can get to the disease earlier before a lot of scarring develops.
Dr. Gabriela Hobbs
ASH 2023 Updates on Interferon
Ruth: There was an interesting study presented at ASH about interferon-α versus hydroxyurea, which is the oldest of the drugs still used for myelofibrosis or MPNs. This study was in untreated MPN patients who were unable to take ruxolitinib. What did we learn?
Dr. Hobbs: Several abstracts were presented with interferon. One was the updated results of the DALIAH study comparing pegylated interferon to hydroxyurea for patients with earlier disease essential thrombocythemia and polycythemia vera. There was also another study looking at earlier myelofibrosis, like pre-fibrotic myelofibrosis.
There’s been a lot of interest in looking at interferons in general across the spectrum of the disease. One of the areas where there’s a lot of interest is looking at pre-fibrotic myelofibrosis or early myelofibrosis to see if we can get to the disease earlier before a lot of scarring develops.
If we look at all the characteristics of the patients who had stable disease for years versus those who progressed, is there a difference that AI can say if you look at these particular parameters, this is a warning sign?
Dr. Raajit Rampal
Artificial Intelligence in Hematology
Ruth: There was a fascinating presentation on the use of artificial intelligence, specifically to differentiate between essential thrombocythemia and pre-fibrotic primary myelofibrosis. Is that something that you see coming into practice or are we way off on that?
Dr. Rampal: We’ll level set by talking about what we mean by AI, which neither of us are experts in. One of the powers of AI is to take broad sets of data and identify patterns. That is a very simplistic way of thinking about the many things that AI can do and is built to do. It can take thousands of variables and find patterns that humans aren’t going to be able to find in real time.
This is an example of what you’re talking about. If you took thousands of bone marrow samples and you said that clinically, these people look like ET, but based on the other parameters that we have, these people look like myelofibrosis. Is AI going to be able to better discriminate versus a human and say this pattern better fits the ET pattern and that pattern better fits the MF pattern?
It will help us refine some of the key characteristics of the disease. The hope is that it may also give us some clues for things like progression if you look at the pattern of a lot of patients. We’re talking about thousands of patients and if we look at all the characteristics of the patients who had stable disease for years versus those who progressed, is there a difference that AI can say if you look at these particular parameters, this is a warning sign? That I think is part of where we think this is going to go.
There are lots of great resources online where, as a patient, you can advocate for yourself to recommend different treatments to your provider to make sure that you’re getting the most updated care.
Dr. Gabriela Hobbs
How Patients Can Be More Proactive in Their Treatment
Ruth: Now that we’ve heard updates out of ASH 2023, what can a patient bring to their community hematology-oncologist as opposed to waiting for it to trickle down? What are some of the ways that a patient can be more proactive with knowing what we now know?
Dr. Hobbs: If you’re a patient or a family member of a patient, you’re already taking those steps that are so important. It’s important to remember that myeloproliferative neoplasms are rare diseases so not everybody has access to subspecialized care.
What’s incredible about the MPN community is that the group of clinicians who treat MPN and are doing research in MPN are extremely committed and passionate about treating these diseases. We’re excited to work with industry partners who are similarly very passionate about finding new therapies for these diseases.
There are lots of great resources online where, as a patient, you can advocate for yourself to recommend different treatments to your provider to make sure that you’re getting the most updated care.
It’s worth asking your physician: when is it time for me to get started on treatment? If you are at the point of needing treatment, it may be worth getting a consultation in a center where there’s a lot of experience.
Dr. Raajit Rampal
Dr. Rampal: If you’re a patient who’s being cared for in the community, it’s worth asking your physician: when is it time for me to get started on treatment? This is an evolving space. We’re more and more convinced that earlier may be more beneficial, but there is a danger in waiting too long.
If you are at the point of needing treatment, it may be worth getting a consultation in a center where there’s a lot of experience. We, who are focused on this, have the forefront of the developments at our fingertips. Doctors in the community setting are busy seeing a lot of different types of cancers. They have to keep up on all of this and they may not have immediate access to that information.
If it is time to get treated, it may be worth a consultation at least to say, “Is this the right thing? Or is there a compelling clinical trial that maybe may make more sense right in the current era?”
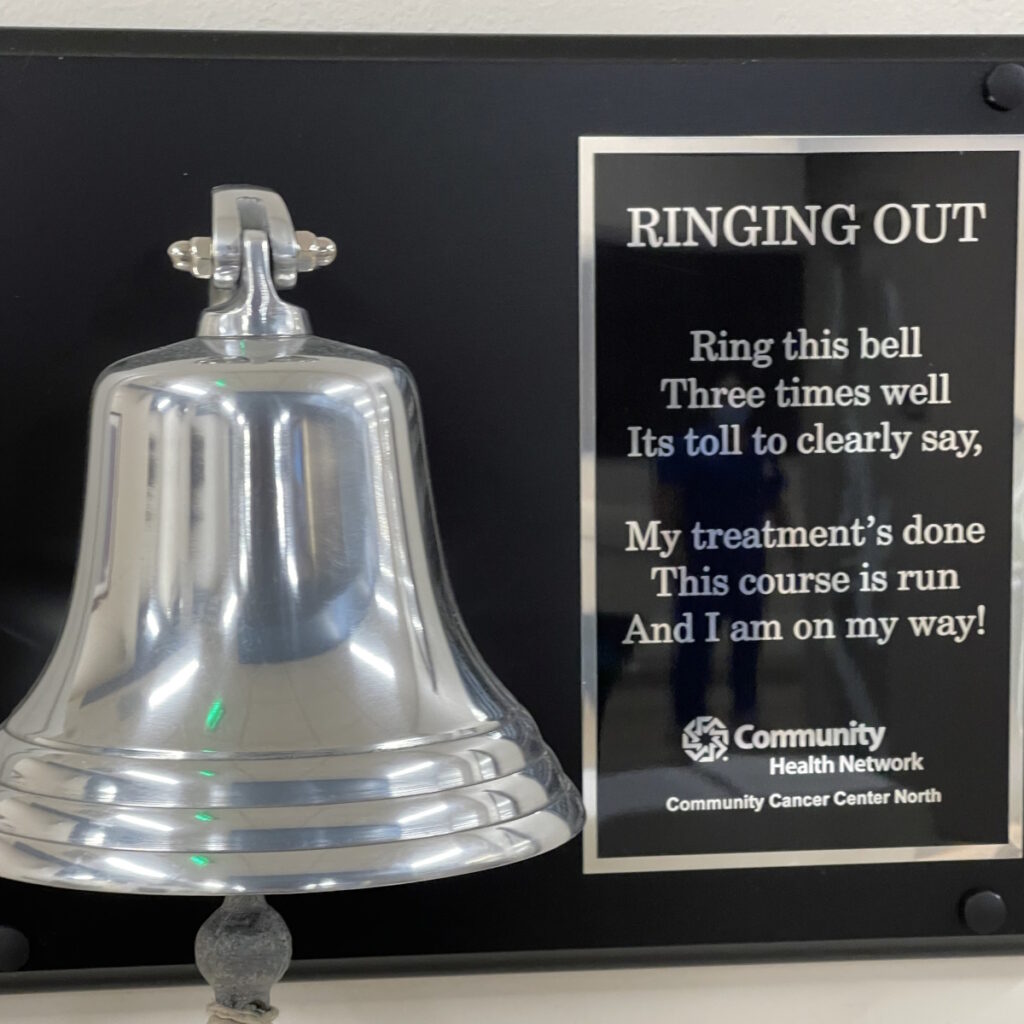
We’re bringing back hope. We’ve seen more developments at ASH 2023 than in maybe any prior in the last ten years that I can think of. That’s not unimportant.
Ruth: That’s a very hopeful message. We seem to say that every year but maybe now even more than ever.
Conclusion
Ruth: From a patient perspective, one of the themes that came out of ASH 2023 is all these new approaches to old diseases. It’s not that we’ve discovered new diseases. It’s that these are diseases and patients who have not had solutions for so long or our options have been so limited and now there are more and more options.
Thank you both so much for your time, Dr. Hobbs and Dr. Rampal. Always my pleasure.
Stephanie: Thank you so much, Ruth, for being our incredible patient advocate and moderator. Also to Drs. Hobbs and Rampal for the work and research you do to help move the landscape of myelofibrosis options.
We hope that you walk away with a better understanding of the latest treatments and clinical trials in myelofibrosis. They may or may not be right for you, but it is our goal to make sure you feel empowered to make a decision for yourself.
Thank you and we hope to see you again at a future program at The Patient Story.


Special thanks again to GSK and Karyopharm for their support of our independent patient education content. The Patient Story retains full editorial control.