Types of Lymphoma, Symptoms and Diagnosis, and Treatment Options
Lymphomas refer to a broad class of blood cancers that affect blood cells, bone marrow, lymph nodes, and the lymphatic system in general. Leukemia, myeloma and myelodysplastic syndromes (MDS) are other common types of blood cancers, and there are more than 70 different types of lymphoma.
Learn more about the types of lymphoma, signs and symptoms, treatment options, and patient stories.
What is lymphoma?
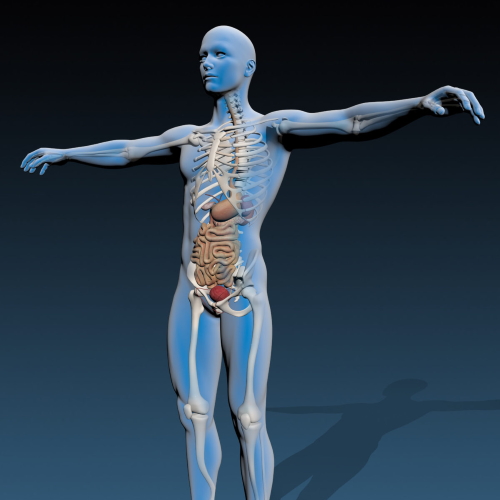
Lymphoma is a type of blood cancer that affects the lymphatic system. The lymphatic system, or lymph system, refers to the circulatory and immune system organs and tissues that help support your body’s immune functions.
There are many different types of lymphomas, some of which are aggressive and others that are very slow growing. The more than 70 types of lymphoma are broadly put into one of two classes: Hodgkin lymphoma or non-Hodgkin lymphoma.
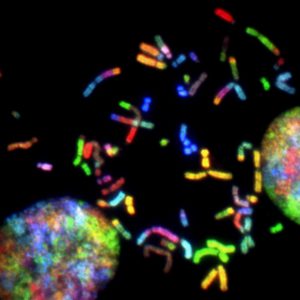
Both Hodgkin and non-Hodgkin lymphomas can occur in children and adults, and they generally develop from white blood cells called lymphocytes. Cancer develops in B lymphocytes and T lymphocytes (B cells and T cells, respectively) and can then travel to other parts of the lymphatic system and beyond.
Cancer cells can eventually form tumors in lymph nodes, bone marrow, the bloodstream, and other organs.
Hodgkin lymphoma
According to the Lymphoma and Leukemia Society, approximately 8,000 – 9,000 people are diagnosed with Hodgkin lymphoma (Hodgkin’s disease) annually.
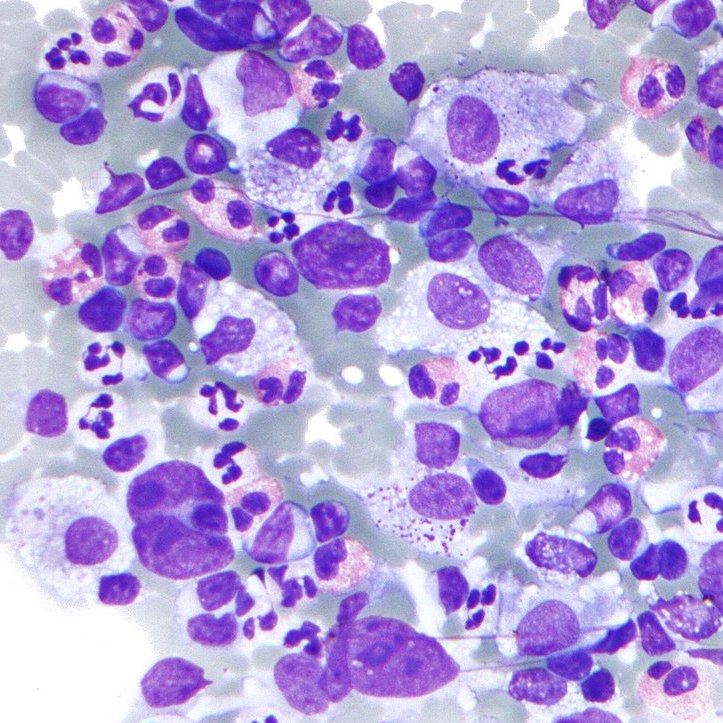
Hodgkin lymphoma’s cellular hallmark is the presence of a particular type of tumor cells called Hodgkin Reed-Sternberg cells, a mutation of B lymphocytes. These abnormally large cells are confirmed through biopsy samples.
Hodgkin lymphoma is more common in young adulthood, particularly in adults in their early 20s. Hodgkin lymphoma may also present in late adulthood (55+). It affects both males and females.
Hodgkin lymphoma types
There are two main subtypes of Hodgkin lymphoma: classical and nodular lymphocyte predominant. Ninety percent of Hodgkin patients present with classical Hodgkin lymphoma.
Classical Hodgkin lymphoma can be broken into four subtypes:
- Nodular sclerosis
- Mixed cellularity
- Lymphocyte-rich
- Lymphocyte-depleted

In person I was told that it wasn’t cancer, that it was some sort of infection that was causing the lymph nodes to be inflamed, but they sent it in to a different place for a second opinion.
That came back as Hodgkin’s.
Wade W., classical Hodgkin lymphoma
Non-Hodgkin lymphoma
Non-Hodgkin lymphoma, sometimes abbreviated as NHL, is the more common class of lymphoma. It can occur at any age, though it is more common in older adults.
There are two major divisions of NHL: B cell lymphoma and T cell lymphoma.
B cell lymphoma
Approximately 80% of NHL diagnoses are B cell lymphomas. This can include:
- Diffuse large B-cell lymphoma
- Primary mediastinal B cell lymphoma
- Follicular lymphoma
- Small lymphocytic lymphoma
- Chronic lymphocytic leukemia
- Marginal zone lymphoma
- Mantle cell lymphoma
- Waldenström’s macroglobulinemia
- Burkitt lymphoma
T cell lymphoma
Although there are some rare T cell NHL cases, the more common T cell lymphomas account for approximately 15% of non-Hodgkin lymphomas, including:
- Peripheral T cell lymphoma not otherwise specified
- Anaplastic large cell lymphoma
- Angioimmunoblastic lymphoma
- Autaneous T cell lymphoma
Lymphoma signs & symptoms
Lymphoma symptoms will vary based on the individual, but many patients report painless swelling of lymph nodes in the neck, armpits, or groin. Some other common symptoms include:
- Fever
- Rapid weight loss
- Night sweats
- Fatigue
- Body itching
However, these symptoms may not necessarily mean cancer. Swollen lymph nodes are common when fighting infection or when you have a cold. If any symptoms persist without change (or they get worse), you should see a doctor so they can determine the root problem.
I think a lot of the cancer websites really get it right when they describe cancer fatigue as the fatigue that doesn’t go away when you sleep or you rest.
Luis V., diffuse large B cell lymphoma
I had an incredible hard time breathing through my nose (near 90 to 100%) blockage which led me to seek the ear, nose, throat (ENT) doctor to take a look.
As a result, I had the ENT in Santa Barbara diagnose the issue and help by having a simple procedure to remove the tissue. When they removed the tissue, he found some of the tissue suspicious and as a result, sent it in for a biopsy.
It was through this surgery that they first discovered Hodgkin lymphoma cells in the tissue removed from my adenoids. Before that, I had no idea that I had Hodgkin’s lymphoma.
Helicon K., Hodgkin lymphoma

Lymphoma Diagnosis
Because there are so many types of lymphoma and treatment varies based on type, making the correct diagnosis is critical. Your doctor will review your physical symptoms, but diagnosis is determined through a biopsy.
A biopsy is a procedure where a doctor removes a small piece of tissue for examination. A surgical biopsy is an outpatient procedure where the lymph node or diseased tissue is removed partially or in full.
A core needle biopsy involves using a hollow needle to remove a core tissue or fluid sample.
In addition to a biopsy, your medical team will order imaging tests to determine where the lymphoma is located and how far it has spread. Your doctor will also order a bone marrow biopsy to determine if the lymphoma has spread further.
Imaging and bone marrow biopsy will help determine staging, which will help inform and guide treatment.
In the following three weeks I had a needle biopsy, bone marrow biopsy, a port placed, a surgical biopsy because the cells from needle biopsy had dried up by the time they reached the Mayo Clinic, and a PET scan.
I’ll be honest, the bone marrow biopsy hurt, but that was probably because she couldn’t get enough fluid so she had to do it four times. I don’t think that normally happens, but the surgical biopsy was probably the worst. It hurt for weeks after and I’m now left with a decent sized dent on the right side of my chest where the scar is.
Keyla S., Non-Hodgkin lymphoma

Lymphoma Staging
The Ann Arbor classification system was originally developed for Hodgkin lymphoma diagnosis but is now used to diagnose disease severity for all types of lymphoma.
- Stage I – Stage I is localized to a single lymph node region or single organ.
- Stage II – Stage II defines disease that has spread to two or more lymph node regions on the same side of the diaphragm.
- Stage III – Stage III involves disease on both sides of the diaphragm and may or may not involve the spleen.
- Stage IV – Disease has spread to multiple organs outside the lymphatic system.
Some hospitals consider Stage III and Stage IV as the same stage because treatment approaches are similar.
Lymphoma treatment
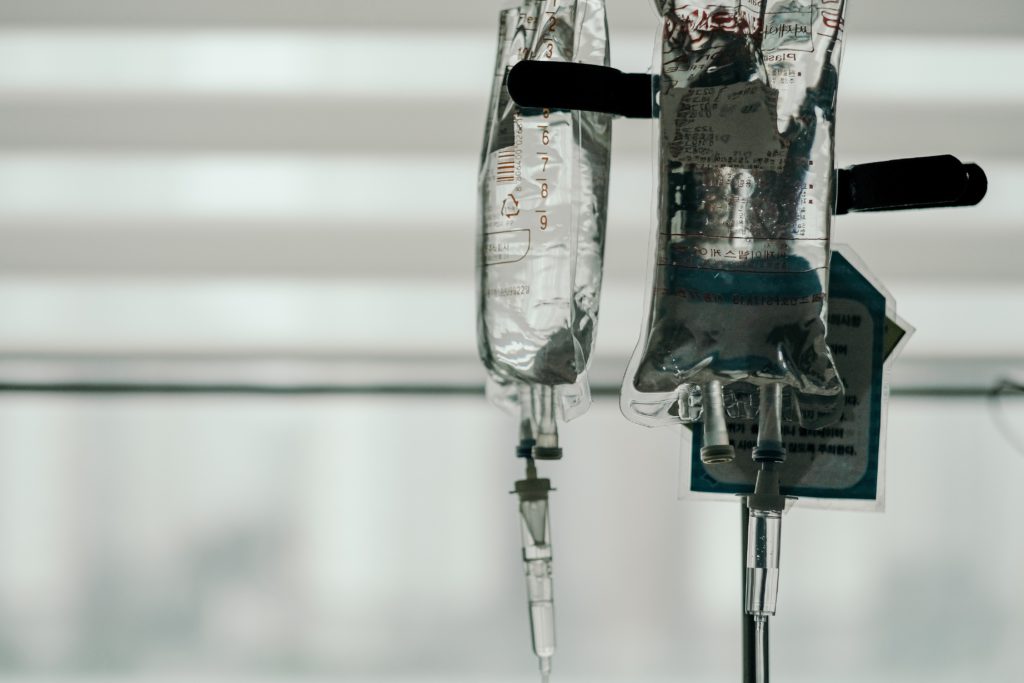
Treatment will vary based on the type of lymphoma, the staging, and how aggressive the disease is. Broadly speaking, these treatments are the most common:
Hodgkin lymphoma treatment
Hodgkin lymphoma is usually treated with chemotherapy and radiation therapy. The most common chemotherapy course is known as ABVD, named after the four drugs used in treatment:
- Doxorubicin (Adriamycin)
- Bleomycin
- Vinblastine
- Dacarbazine
The “red devil” was push chemo. That typically went by pretty fast. That one didn’t do a whole lot to me during the infusions. I only had two infusions of the bleomycin because it was destroying my lung function so bad. They had to cut it out.
Once I got to the vinblastine, I was just so exhausted. I pretty much slept through that and had the dacarbazine. That was light-sensitive, and it was wintertime thankfully, but any time I would go out in the sun, it was so sensitive. I had to wear long sleeves and hats.
Madi J., Hodgkin lymphoma

I got ABVD chemo for the first two cycles, which was four rounds. For the rest of the eight treatments, it was just the AVD.
They took out the B drug (bleomycin) because my PET scan after the first four treatments showed that I had no evidence of disease. They were able to take out the bleomycin since it can be hard on your lungs.
Lia S., Hodgkin lymphoma
Once I got to the vinblastine, I was just so exhausted. I pretty much slept through that and had the dacarbazine. That was light-sensitive, and it was wintertime thankfully, but any time I would go out in the sun, it was so sensitive. I had to wear long sleeves and hats.
Madi J., Hodgkin lymphoma

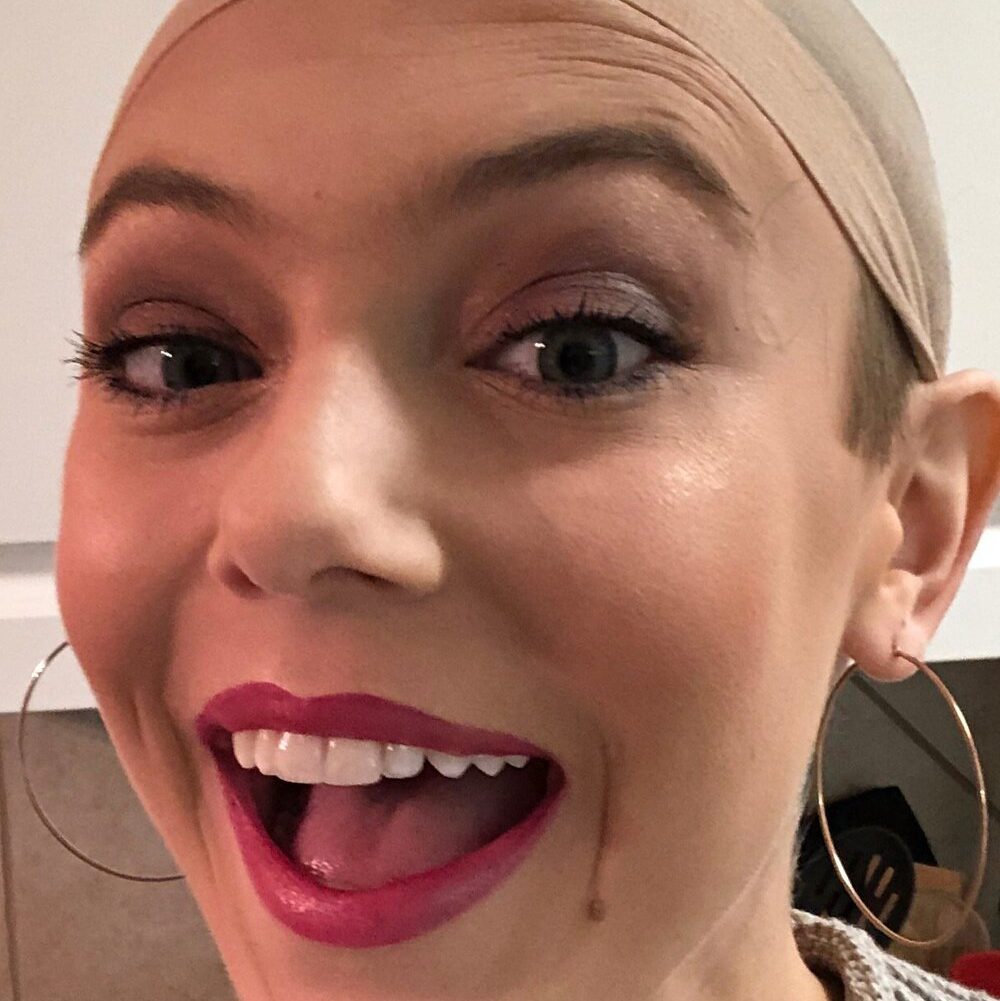
Non-Hodgkin lymphoma treatment
Non-Hodgkin lymphoma is also often treated with chemotherapy, with R-CHOP being the most common chemotherapy course for B cell lymphomas:
- Rituximab
- Cyclophosphamide
- Doxorubicin hydrochloride
- Vincristine sulfate
- Prednisone
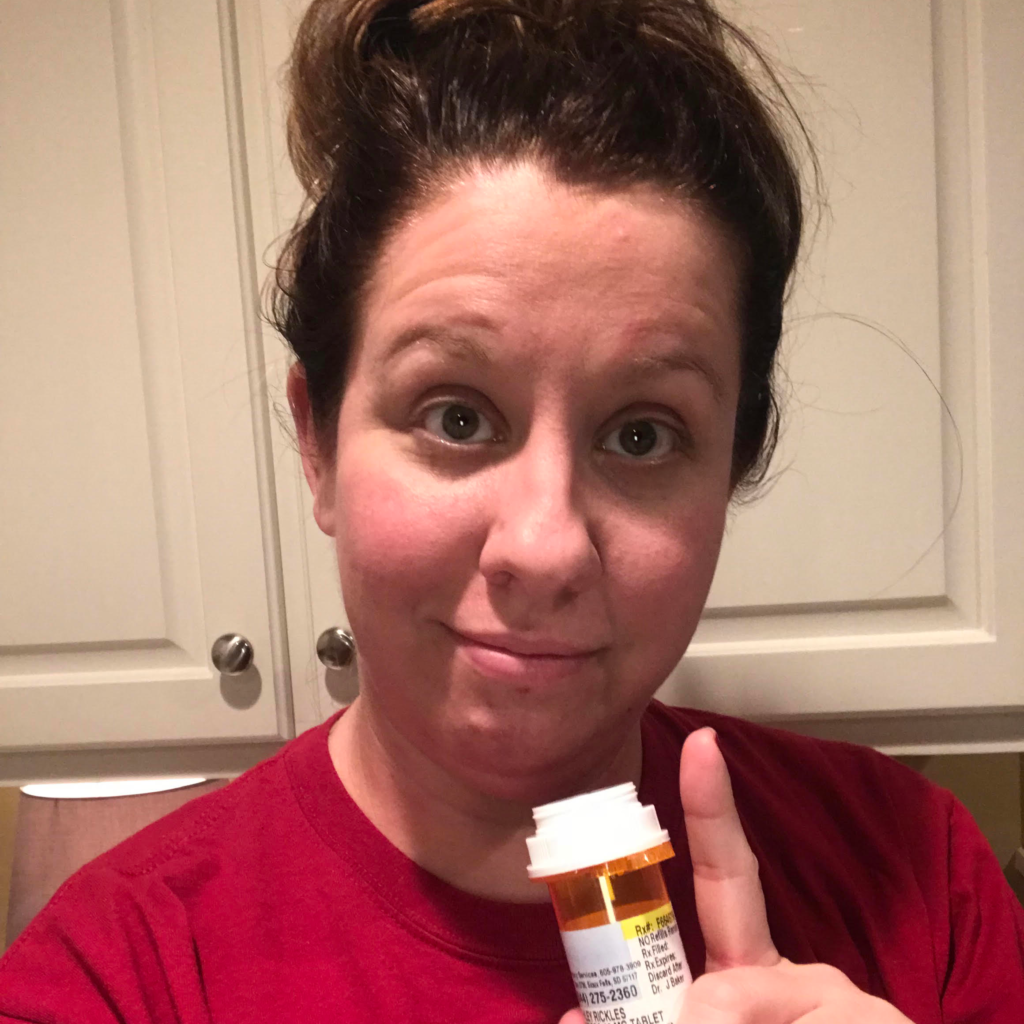
The first round, the first week I just felt headache-y. I wouldn’t say I felt 100-percent but I felt fine, which is really weird. That was good, the first round, until about the third week. My hair started falling out.
I think in my third round, my doctor said rounds three, four, and five are the hardest. She was 100-percent right. Round two was okay, I felt gross the first week but nothing major. I felt nauseous but it was controllable.
Round three I felt really awful. Headache-y, so nauseous, everything tastes awful. I did get really bad mouth sores every round after that. It really hurt to swallow. Brushing my teeth was incredibly painful so that was really hard.
Emily G., Non-Hodgkin lymphoma
Lymphoma survival statistics
Since 1960, when data first became available, 5-year survival rates for Hodgkin lymphoma have doubled from 40% in the 1960s to almost 90% in 2016.
For people age 45 or younger at diagnosis, the 5-year survival rate is around 95%.
For non-Hodgkin lymphoma cases, the 5-year survival rate is around 75% as of 2016. In people with NHL diagnosed younger than 45, the 5-year survival rate is 84.7%.
And it’s not perfect, right? Because here I am. I’ll be six months in remission in a few days. Gee, that’s great, right? What does it mean? Well, it doesn’t really mean anything in and of itself. Doesn’t mean I’m cured, doesn’t mean that I’m going to be alive in 10 years, it doesn’t mean I’m going to be alive 20. What it means is that I’m six months in remission, and I’ve got today.
What am I going to do today? I’m going to help somebody today. How am I going to be seen today? How am I going to see other people today? That’s really important. And I would encourage people, when others say, “Live every day as if it was your last,” to really shut that message down. Because to me, that message works best when you cut it in half, and you just leave it at “Live every day.”
Luis V., Non-Hodgkin lymphoma

Want to share your story?
Share your story with us!