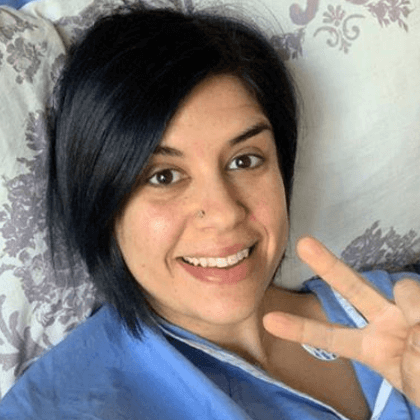
Amanda’s Stage 2A Colon Cancer Story

Amanda G., Colon Cancer, Stage 2A
Symptoms: Gurgly stomach, blood in stool, chronic constipation
Treatment: Surgery (hemicolectomy), chemotherapy (CAPOX), Zarxio
Table of Contents
Amanda was experiencing gastrointestinal symptoms, including bloody stools, which worsened and persisted for almost a year before she finally got a colonoscopy.
She was then diagnosed with stage 2A colon cancer.
She talks about the frustration of not feeling listened to and taken seriously, how important it is to fight for answers and advocate for yourself, and why you should be on top of your health care.
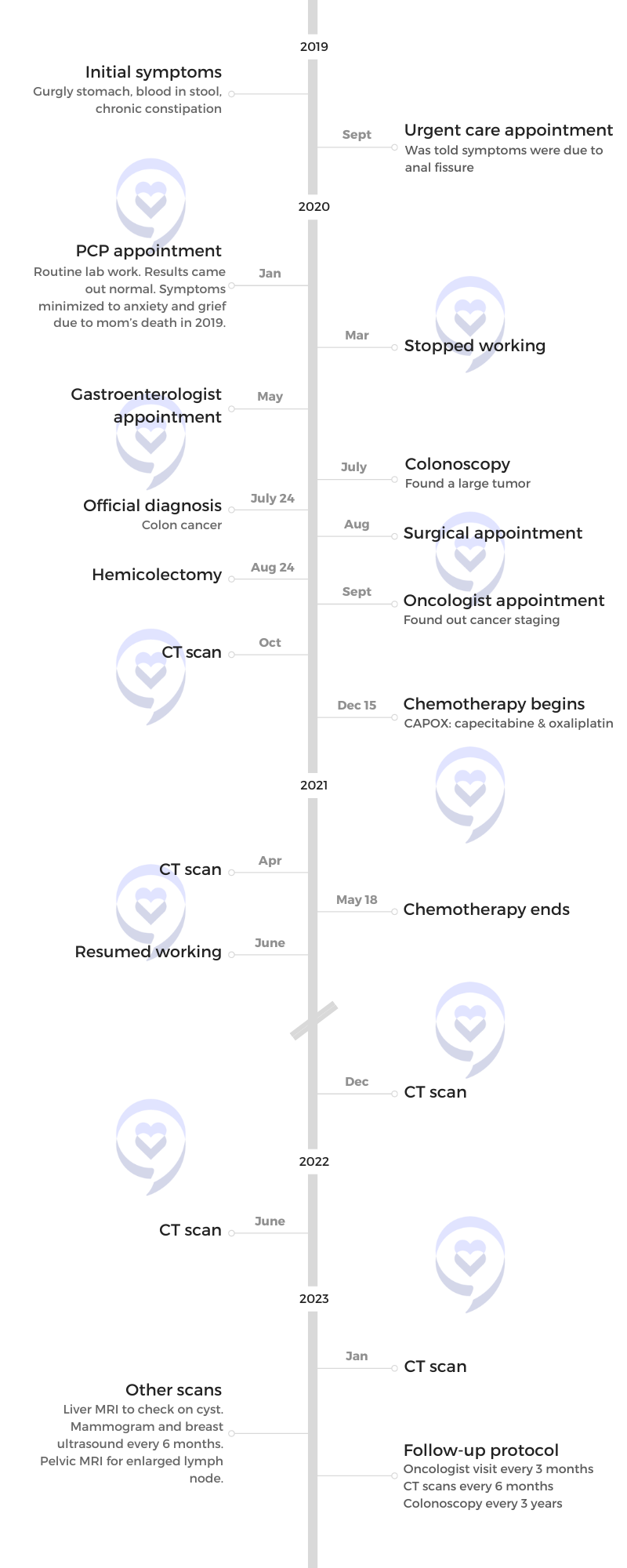
Initial symptoms of colon cancer
In August/September 2019, I started getting weird but very light IBS symptoms, like something as simple as a gurgly stomach when I was hungry. But it would be so consistent. It would be every day, something I had never dealt with before.
I thought, “That’s weird. Is it my diet?” My mind didn’t go to the worst. Those were my early, early symptoms.
Then about a month later, I started seeing blood. That was alarming because, of course, it’s blood. But again, you don’t want to freak out. I gave it a couple of weeks and I thought, “Maybe it’s hemorrhoid. Let’s see if this is consistent and persistent,” and it was.
I didn’t have insurance at the time so I went to my local urgent care where I was told it was probably just hemorrhoids, probably a fissure.
I laughed in the office and said, “I don’t want to have like colon cancer or something,” and the doctor reassured me, “I don’t think you have cancer. I think that’s a little outlandish even to assume that. I think you’re fine.”
I asked how long I could expect to have it. She said, “It depends.” She gave me a really loose-ended answer. “Typically, [in] a couple [of] weeks, it’ll heal up. But if it’s a fissure, like a tear, if you don’t change your diet and eat more fiber, that could be chronic and you could just see blood for months.”
Just keep an eye on it. No solid answer. I wasn’t super thrilled with it. There was no exam done, no blood testing. I took her for her word.
Still dealing with the gurgly stomach but very minor and the bleeding. I just assumed it was a fissure or hemorrhoids. I thought, “Okay, let’s ride this out and see how long this lasts.”



Physical symptoms of grief
In February 2019, I lost my mom suddenly. I wasn’t there. She died of a heart attack 3,000 miles away.
A lot of people who are grieving deal with similar symptoms. Anything you’re going through will manifest itself through your gut. I had a lot of people tell me this was grief.
It wasn’t until I actually saw my first doctor [that] he said, “You’ve been through a lot. I wouldn’t worry about this. I truly think it’s just grief.”
My primary care told me I needed psychological intervention because I was panicked at that point. When I got my health insurance in January, I was excited. I got to see a doctor [and] get blood work and all these tests done. He ran the blood work and it all comes back normal, which was a relief for me. That was all he decided he needed to know that I was probably just grieving.
With these symptoms came anxiety. I was never a hypochondriac. It wasn’t until I had these symptoms that I thought, “Something’s wrong,” which I think is your body telling you something’s wrong. There’s no reason for me to doubt that.
This was January 2020. The doctor told me, “There’s nothing wrong with you. You have no family history of colon cancer. You’re so young. This would be very outlandish.”

Possibility of colon cancer
I mentioned it multiple times. I mentioned it at the urgent care. It’s the first thing I thought of when I saw blood. I’m very smart. I’d like to consider that I am very in touch with my body. I understand these things.
When I was growing up, my mom was very ill and I was in and out of hospitals with her. I was comfortable with it [and] I had a head start on maybe what other people wouldn’t.
I thought, “This is a symptom of colon cancer.” I know I’m 29, but I kept bringing it up to the doctors. Their response was, “Oh, that’s silly. There’s no way that would be colon cancer.”
I, of course, Googled my symptoms. At the height of my anxiety and my symptoms, I was on Google almost every night before bed, just trying to find someone else who maybe had gone through this. I would be on YouTube, searching [for] these symptoms.
Symptoms persisted & intensified
I went on this amazing trip for my 30th birthday in March 2020, weeks before everything shut down. I went to Hawaii and Australia. I booked it because it’s a big birthday. I was going to process my mom’s death on this trip. It was going to be really a beautiful trip for me to say goodbye to this really crazy decade and start my new one.
It was wonderful. I had the best time [and] met a lot of great people, but my symptoms just intensified. It was almost like my body was saying, “Now’s the time. This isn’t going away.”
At this point, I’d been bleeding since September. It’s now March. I was chronically constipated. I couldn’t go to the bathroom and when I could, it was just blood. There was no pain. I was pretty bloated a lot of the time.
I just remember feeling like I couldn’t really enjoy my trip because there was something in the back of my mind saying something was wrong. That was when I thought, “When I get back from Australia, I’m going to insist on getting a gastroenterologist and get this ball rolling because something is seriously wrong.” At this point, I need to fight for it.
Initial appointment with primary care physician
I get back home to L.A. right as everything’s shutting down. Doctors are not seeing patients in person anymore unless it’s considered urgent. Trying to get a hold of any doctor is seemingly impossible. Every appointment is over FaceTime or Zoom.
I got an appointment with my primary care. I said, “These symptoms aren’t going away. In fact, everything seems to be getting worse. I’m really concerned.” He said, “You don’t look sick. If you had cancer, Amanda, you would be losing weight at a rapid pace. Your face would be sunken in.” I just couldn’t believe he said that to me.
I said, “Yeah, if it were bad, if it were end-stage cancer, of course. I’m telling you what I think is happening and you are dismissing everything and not even offering a solution.” Finally, he said, “Your blood work is fine. If it were cancer, you would have anemia.”
My red blood cell count was low and normal. My mind went to, Maybe I’m not anemic now but give it a couple of months, that red blood cell count will go lower if it is a tumor. I’m thinking all this and I thought, “I can’t go to the bathroom without aid from a pill. I’m seeing blood. Clearly, there’s something blocking everything moving.”

Getting initial testing done
He said, “If you’re really this stressed about it, I will order a stool sample test for you.” This was the, “Aha!” I know this is going to come back abnormal. If anything, this will get things moving. This is how he worded it, “Just to ease your mind, we’ll get you a stool sample test,” and I said, “Perfect. That’s all I want. Let’s just get some proper testing done.”
I get the stool sample test done and that following week, he called me. “We got your results back and it came back positive for blood,” which I knew it would. He goes, “I’m going to refer you to a gastroenterologist,” which is all I wanted in the first place. That should have been done in January.
Because of COVID and everything being slow-moving, I didn’t get a virtual appointment with my gastroenterologist until May. [At] this time, my symptoms are so bad.
In early May 2020, the Black Lives Matter protests and marches were happening and I wanted to go out and support. I had been cooped up for a few months now so we donned our masks, went to Burbank, and protested. It was a hot day and I remember feeling really dizzy and really faint. At one point, we all got down on the ground and I couldn’t get back up. My vision went blank.
I looked at my friends. They know what I was dealing with and what I was going through. I was very vocal with them. They asked, “Are you okay?” I said, “I’m very dizzy and my vision just blacked out. I need to sit for a second.”
My friend’s husband sat with me while they went on. I found the energy to get up and start walking. My friend was giving me snacks. She said, “Do you need food? Are you dehydrated?” If you’re dealing with these other symptoms, I would have thought I was dehydrated. I would have thought it was hot. We’re in masks. We’re walking. Maybe that’s it.
But I just knew. I remember looking at her and I was like, “I think it’s connected to these symptoms here. I know it’s related.” Even more, I was just ready to see the gastro.
I saw my gastroenterologist and he echoed what my primary care said. “You’re young. You’re a healthy girl. You have no history of colon cancer in your family. These symptoms are very common, Amanda.
“We’ll test you for ulcerative colitis. We’ll test you for Crohn’s,” both very serious chronic diseases that you want to be taken seriously. He said, “But the odds of colon cancer are so slim so don’t let your mind go there.”
How can it not? The symptoms are not getting any better. They are consistent and persistent. He said, “We’ll get you in for a colonoscopy.”
I said, “How fast can we get that?” He said, “We have to get your insurance to approve it.” Trying to get a colonoscopy approved for a 29-year-old girl with no pre-existing anything is seemingly impossible.
Waiting for the colonoscopy to get approved
The referral went in and then it’s almost like it got lost in limbo. I didn’t hear back from my insurance. I never got the authorization in the mail.
I called them and I was going back and forth. They said, “Hey, we’re super busy with COVID. Sorry about the delays.” I was on hold for so long.
I remember calling them every single day. “Do you have a referral from this doctor? I need this.” They said, “Oh, well, he didn’t say it was urgent. We’re just taking urgent authorizations. We’re getting through these as fast as we can.”
I’m as patient as I can be and [in] the midst of all of this, anxiety is at an all-time high. I’ve never dealt with anxiety. I’ve never dealt with panic attacks. I sympathize with anyone who deals with it all the time because it is the worst thing that you could deal with.

Feeling like no one was listening & not being taken seriously
It’s hard. You feel all those feelings and associate those thoughts with anxiety. I wanted to turn it off because I thought, “That’s the anxiety talking.” But, at the same time, my body was telling me something completely different.
I would message my friends at 1 a.m. after going to the bathroom and seeing blood. They asked, “Are you in pain?” I said, “I’m not in pain, but I don’t feel right. I just feel like the longer this goes, the worse it’s going to get. I feel like my body, from the inside, is failing and giving up,” especially after that spell in Burbank when we were protesting.
I’m really grateful to have this information to share with people. I have a lot of women, especially in my DMs on Instagram, with concerning symptoms. In one way or another, they found out about my story and reached out to me.
Trying to get a colonoscopy approved for a 29-year-old girl with no pre-existing anything is seemingly impossible.
Amanda G. Tweet
Colonoscopy prep & procedure
The colonoscopy was an interesting experience. I’ve never had one before.
You have to be on an all-liquid diet. You can’t eat any food the day before so you’re hungry. You’re given this prep that you have to drink the day before your procedure. It cleans you out.
It’s not ideal. I wouldn’t say it’s terrible. I don’t want people to fear that. I don’t want people to not get a colonoscopy because they’re afraid of the prep. It’s doable. Have some candies that you can suck on after or even lemonade to chase it.
You’re going to the bathroom all night. You are clearing everything out and you know it’s working. The clearer your bowels, the better the procedure is going to go, and the more accurate it will go. They were said, “You don’t want to come in for your colonoscopy and have it be an incomplete colonoscopy and you have to do this again.”
You go in for your colonoscopy and I was asleep during. I know some people are awake, just groggy. I was completely sedated, but I know that’s not the case for everybody.
The procedure itself was so easy and so quick; in and out in a couple [of] hours. No pain after. You go and can finally eat.
The prep is the worst part and even that I wouldn’t say is bad enough to the point where you shouldn’t go. There are preps that come in pill form. See if your gastroenterologist will prescribe that.
I get one almost every year. [For] the past two years, I’ve gotten them every year and now, they’re going to move me to every three years. Not fun but not the worst thing.



Finding a large tumor during the colonoscopy
The doctor came in. I know doctors are very clinical and to the point, but he said, “We found a large tumor in your sigmoid colon. I biopsied it. Call me tomorrow for the results.”
I’m high as a kite on these drugs. You couldn’t have told me at a better time because [at] that moment, I thought, “Whatever. Tumors can be benign, right? Great. I have my answer.” I’m looking around at the nurses and thought, “Hey, it’s probably benign. At least I have my answer.”
Then you start coming off the drugs. One of my nurses was lovely. He wheeled me out when my friend came to pick me up and I asked, “What happens now with the tumor in my colon?” He goes, “This happened to my friend and they’ll just cut the tumor out and you’re going to be golden. You’re going to be fine.”
On the drive home, I was telling my friends and they were super supportive. “You’ve got this. You’ve got your answer, on to the next.” This whole time, I’m rationalizing in my brain. Tumors can be benign and they often are. Maybe it’s just a benign tumor.
It was a large tumor. We didn’t know how large until my surgery, which is crazy. It had grown in my colon. I remember thinking, “I have to wait for these results,” and luckily it was just the next day.
Finally getting a colonoscopy
I go for my colonoscopy in July and, of course, there [are] hoops and hurdles to get there. It finally gets approved.
We’re [at] the height of COVID. Now come COVID tests and all those preliminary appointments you have to get.
I remember thinking, “Okay, I’ve gotten this far. We’re now almost a year of symptoms and I’m at the homestretch. I’m going to get my answers.” Waiting for my friend to pick me up to take me to the hospital, I thought, “I’m going to get my answer today.” This has been months and months of absolute mental and physical torture.
I go to the hospital and have my colonoscopy. I deal with things with humor. “Hey, am I the youngest patient you’ve ever had?” All the nurses were lovely. They were so kind and super reassuring.
Once they hook up the drugs to you and you’re loopy, you’re golden. I expected the worst but also don’t think I was prepared to hear it because you hope for the best. You know in the back of your mind, but you never expect what you’re going to hear.
When I woke up from the colonoscopy, I remember looking around the room. The nurses were there and they were just quiet. “Good morning, Amanda. You’re all done.” I’m groggy. I didn’t know what questions to ask.
Diagnosis
Getting the results of the colonoscopy
I was in bed, my head just spinning. I’d already called my family back in Massachusetts and told them what was going on. They said, “Keep us posted. Tumors are often benign. We have all the faith you’re going to be okay.” I said, “Yeah, I think I’m going to be okay but at least I know I have a tumor.”
My doctor called and he goes, “Pathology came back and it is cancer. Please come to my office right away for the next steps.”
You are never prepared to hear that, but in the same sense, I knew. This whole time I knew. I had been saying colon cancer since September. It wasn’t new information. Everything checks out.
I was laying down when I got the phone call. I sat up immediately and said, “Okay, do I come now?” He was sad, “Yeah, come now.”
Follow-up appointment with the gastroenterologist
Immediately call my friend and told him it’s cancer. He was like family to me out here. I love him to death. He asked, “What are we doing?” I said, “I need to go to the doctor.”
He picked me up and brought me to the office. That was an interesting car ride and visit. I was just very quiet and shocked.
Things just start going in your mind. How long did I let this go? Did I not fight hard enough for myself? My symptoms have been going on since September of last year. Surely, it’s all over my body by now.
We get into the office and he gives me all my paperwork. He gives me the next steps. He goes, “I’m going to refer you to a surgeon. If the cancer has spread, you will need chemo. If it’s localized, it’ll just be surgery.” It was a lot of information all at once, the same day I heard the diagnosis.
I remember being looked at by everyone in the office as I was leaving. Just diagnosed with cancer and I’m just like, “Okay, bye!” Then you get a lot of, “We’re praying for you.” As nice as that is, I thought, “Oh, this is going to be a whole thing. This is scary”
Treatment
Surgery
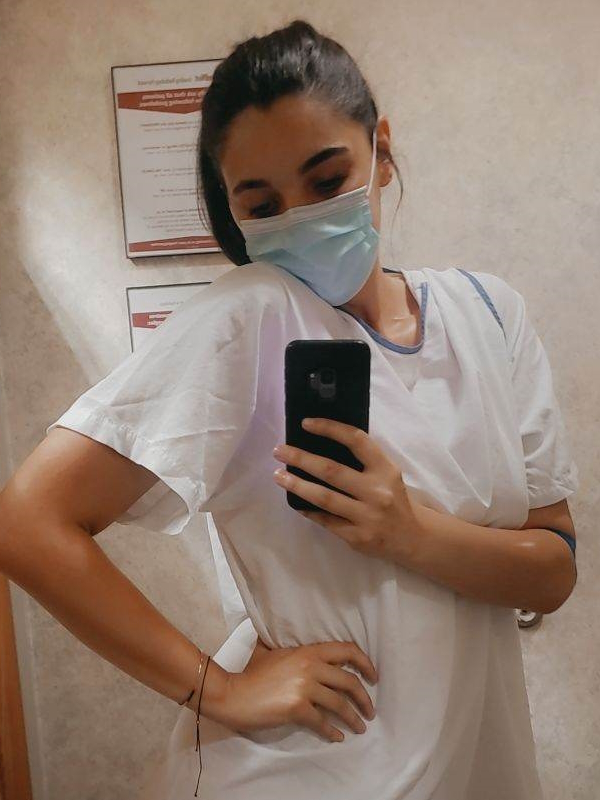
My surgery was another hurdle. I had to keep on my insurance company to approve the surgery. I finally got my surgery a month after my colonoscopy, which in hindsight is about right. It just felt like forever.
They didn’t scan me prior to surgery. I didn’t find out my stage until after surgery when I met with my oncologist.
The surgeon took out the tumor, said it was a large tumor, told me he poked around in there, [and] said there was no visible evidence of metastasis. He said the liver looked good. Everything else looked clear.
He said, “I think you caught this early, but obviously, you have to have a scan and meet with an oncologist to be sure.” He said my lymph nodes were clear, which was a huge relief. He tested 28 lymph nodes. All great news.
Hemicolectomy procedure
I had a hemicolectomy; I just say a colon resection. They removed my sigmoid colon. You have your large intestine, your small intestine, and the sigmoid colon connects to your rectum so it’s right down there.
They went in laparoscopically. It was all done through two little incisions. They went in and took out that part of the colon and resected it.
My surgeon warned me I might need a colostomy bag temporarily. He said, “You might have to have a colostomy bag when you wake up from surgery. If you feel one, don’t freak out. It will be reversed. We’re going to do our best to help make this a clean resection for you.”
All I’m thinking [about] is my pride. I’m 30 years old. I can’t live my life with an ostomy bag. After researching and meeting people, you can have one permanently, live a full life, and be fine. It’s not a big deal. You would much rather have one than not be here from cancer.
It sounded like I’d have to say goodbye to my social life. It’s such a lifestyle change.
He came in and said, “The resection was clean. Everything went well. The tumor was much bigger than anticipated. The colonoscopy picture showed that it was large. It wasn’t until I went in there that it was really large.”
I was really lucky. I had a great surgeon. I had the chief surgeon of the hospital perform my surgery. He was an amazing surgeon. Everything healed up nicely.
This whole experience, I’ve been very, very, very lucky because I know every case is unique, but my case could have been so much worse in so many different areas.
Initial appointment with the oncologist
I was recovering at my friend’s place. A couple of weeks later, I met with my oncologist at Cedars and he was lovely. Dr. Gong was the best doctor that I’d had up to this point. The most caring, the most understanding, and empathetic. He’s amazing. He’s the one who staged me.
He goes over my pathology report. I’m there with my friend and I’m terrified. You just don’t want to hear the worst, like terminal, stage 4, not curable. You don’t want to hear those words, but you have to prepare yourself for those words. You have to brace yourself.
First, he said, “Before I say anything, I’m really sorry this happened to you. This should have never happened to you,” and I just started sobbing. I just felt like this doctor cares and is taking me seriously. It was overwhelming and I really felt it. I thought, “This is the person who should be a doctor. This guy cares.”
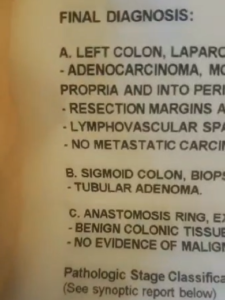
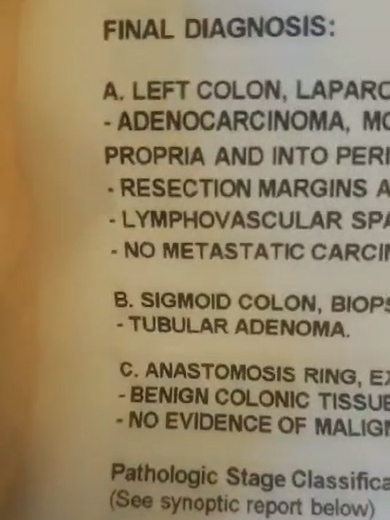
Discussing the pathology report
He said, “I looked at your pathology report and, Amanda, it looks really, really good. You got it in time.” I started crying. He went over everything. He showed me the pathology report. He told me what everything meant.
He said, “We don’t know until you get scanned, but where I would stage you right now is stage 2A.” Staging for colon cancer starts at stage 0, then goes 1, 2, 3, 4, and then substages A, B, [and] C for every stage. I was [in] early stage two.
The staging goes by how much of the colon wall the tumor chewed through. On my pathology report, my tumor had chewed through the first layer, which makes it stage 2A as opposed to stage 1C. It was just starting to chew through and it was very large.
The sizing is the T so on a pathology, it would be T3 and that can go up to 4. The sizing of the tumor and the stage of the tumor is different. It was T3, but stage 2.
I thought, “Great. I caught this in time.” It was very emotional. I was with my friend. I was so happy, so relieved. The surgery was done. It was out of me.



Lymphovascular invasion (LVI)
He goes, “You have something called lymphovascular invasion. They didn’t find cancer in your lymph nodes, but they found the DNA of cancer in blood vessels surrounding the tumor and the tissue, which means you’re at higher risk for this returning.”
I asked, “Okay, what do we do?” He said, “There’s no real evidence of your cancer anywhere in your body, but you have the option to proceed with chemo if you want.
“Obviously, it’s your choice. You don’t have to do chemo. But I highly recommend that you do to reduce the odds of this coming back.” That’s all I needed to hear.
I said, “Of course, I’m going to do chemo.” Again, I don’t think I was really ready for what that meant, but I thought, “Whatever lowers my chances. I don’t want to ever deal with this again so if I have to be sick for a little bit…”
Mind you, being sick for a little bit isn’t just being sick. It’s the worst thing you can put your body through, but I was just so ready to go and get that moving.
CAPOX chemotherapy for colon cancer
I told my oncologist I wanted to start chemo and that was in September. I had to jump through hurdles with my insurance company again.
I’m feeling great at this point. I’m recovered from my surgery. I feel back to myself. I’m not bleeding anymore. I feel great. This is now October/November.
I felt crazy because I’m fighting for chemo and I feel like I don’t need it. My scan was clear in October. I need to keep this from returning, but I haven’t felt this good in so long.
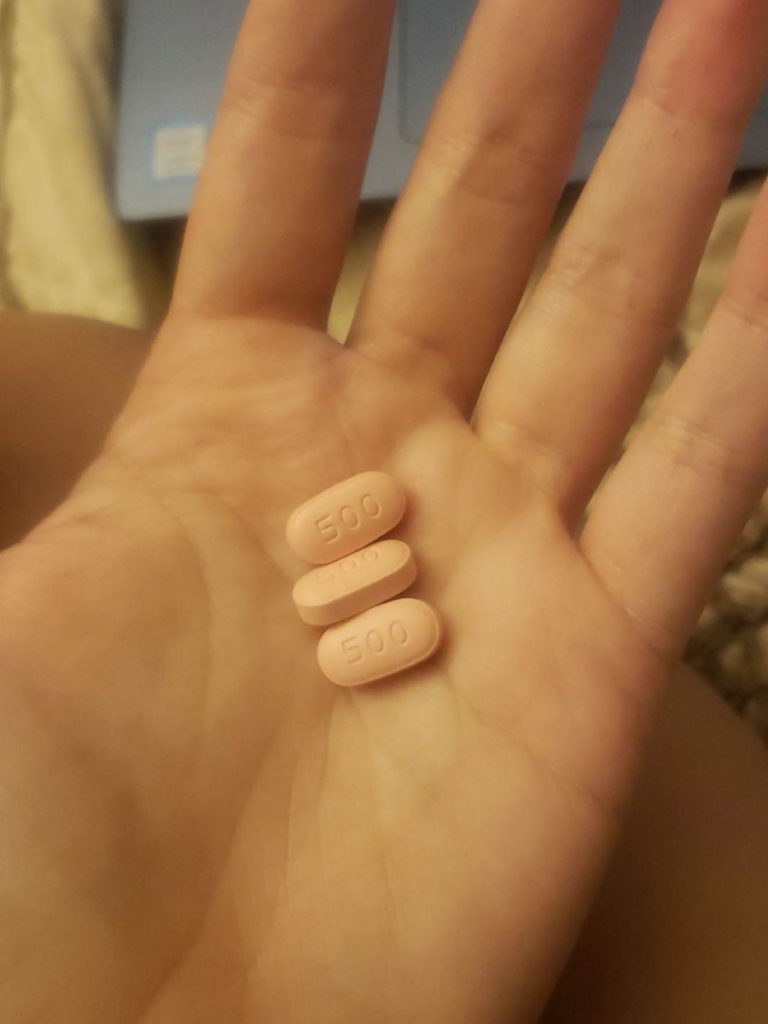
Finally, it got approved. My course of treatment was CAPOX, which is oxaliplatin, the IV chemo, and then Xeloda, which is the pill form of chemo.
My oncologist wanted to do the combo. He’s said, “This is very common. This is one of the most effective routes for colon cancer to keep this from recurring.” He also told me it was one of the most toxic on the body and it’s not fun.
I started in December. I got my port placed the day before chemo, which was the easiest thing. When I got it removed, my doctor let me keep it so I have it as a souvenir. I told him, “I want this. I paid for it. It got me through chemo. That’s mine.”
My anxiety about that was more than chemo. I was freaking out. I joined a colon cancer group on Facebook. I remember putting a post up that said, “I’m so scared to have this port placed because it goes under your skin, on your chest. That seems insane to me.”
Everyone said, “Oh, yeah, it’s an easy procedure. You’re awake for it.” I thought that sounded like a nightmare.
If anyone is in the early stages of their cancer battle and is afraid of getting a port, let me put your mind at ease. You feel nothing. You’re loopy. It’s done in 20 minutes. These doctors do a bunch of them a day. It’s so easy and you’ll be grateful for it. It will save your veins. Trust me.
I was doing chemo every other week for six months. I would go in every other Tuesday. I would do three pills in the morning and three pills at night. I would start my chemo, take my three pills, have my chemo, go home, take my pills at night, [and] go to sleep.
The day after chemo, I would go back to the oncologist’s office and get a shot called Zarxio to boost my white blood cells. Chemo kills your white blood cells so they want to make sure you don’t get sick. They want to make sure that you can come back for chemo the following week and be good.
That shot made me feel so bad, so ill. It would make my body ache. I don’t know what it is about that shot, but my entire body would feel like it got hit by a truck.
I would go in for that shot then they would hook me up to hydration so I’d be at chemo on Wednesday just for the hydration drip through your port. Then after that, you’re good for two weeks.
Side effects CAPOX chemotherapy for colon cancer
The five days following chemo are the worst and it’s cumulative.
The first week I went, I remember thinking, This isn’t so bad. This is 2020-2021. We couldn’t have visitors. We couldn’t have people sit with us, which is fine. I was asleep anyway for the most part, on my phone, or listening to music.
I remember leaving the cancer center that first time thinking, “That wasn’t bad at all. I actually feel fine.” I went home and that’s when it started coming.
I couldn’t even lift up my arms. The nausea was terrible. There’s neuropathy. They warned me beforehand of all the potential side effects of these drugs. They talked about neuropathy and said, “Don’t touch anything cold.” You listen to them, but you don’t really rationalize it.
I went into my fridge, grabbed juice, and it felt a singe. When you touch something cold, it feels like a singe almost. Think of when you get shocked but like a permanent shock and it’s like singeing the tips of your fingers. It would go away when you stop touching something cold. That was the first few cycles.
As the weeks went on and I had more treatments, it became something completely different. My feet and my legs were starting to get numb. I would compare your feet and legs to when your foot falls asleep and you go up to walk — that sensation, that’s what it feels like. Almost like a dead leg.
My fingertips felt completely different. They felt numb and tingly. I didn’t have any pain with it. I know a lot of people have severe neuropathy pain and have to take gabapentin for it.
Again, this is why I say I’m very lucky in all these little aspects of my journey compared to others. I never had pain and I still don’t have pain and I’m really grateful for that because I did 12 rounds. I did it for six months. I got out pretty unscathed.
Neuropathy
I still have some numbness in my feet, but my fingertips are back to normal. My oncologist told me, “We don’t know. Neuropathy can be permanent. It can get worse. It can get better. You can try acupuncture for it,” but my hands are fine and my feet are pretty okay. There’s no pain so I’m fine.
The side effects were cumulative. This is the part of cancer where unless they’ve gone through it themselves or seen someone go through it, people don’t really know how awful it is.
This is the pandemic so no one was really seeing each other. I was talking to my friends through FaceTime. I’d be on my bed, be on the pillow, and would just look terrible. My voice would be so soft.
I’d realize, “I ate a potato today.” It’s all I could manage to get down. Your appetite is gone and you’re so sick, but you can’t actually throw anything up because you’re not eating anything. It’s terrible.
That journey made me understand why people who are on chemo for life [want to] stop because it’s not a quality of life. I get it and I would never judge someone for that decision.
Before, I might have been thought, “Why would you stop fighting? That makes no sense. There’s this treatment out there that can prolong your life.” You get a taste of it and think, “Well, what kind of life is that?” You would rather have a quality of life.
It was quite the journey. A week after chemo, I would start feeling better. I would start feeling like myself. I would always take that week to be outside, have lots of yummy food, and be with my friends to the capacity that I could.
I’m trying not to get COVID because COVID meant I couldn’t have chemo. I would also be putting everyone else in that cancer center at risk so I took it very seriously. I didn’t want to get sick not just for me. I knew I would be okay, but there are a lot of people much older than me, much sicker than me who couldn’t afford to get COVID.
I kept quite a distance from friends, spent a lot of time outside, and would go to the beach a lot with my friends. That felt like a safe place to be — outside, away from people — and that became our little sanctuary. It was just nice to feel normal again. I think that’s what you just want to feel is normal.
I keep my stickers on the wall of every treatment that I had. Every time you go in, you get a new sticker. I would put them around my calendar and count them. Those stickers were a visual for me. When I was in bed feeling my worst, I thought, “Okay, you’ve got six stickers, you just need six more. You’re halfway there.”
My nurse practitioner would check on me in my chemo chair. I was four or five chemos in at that point. I remember asking, “Do I have to do all of this? My scans are good. My blood work’s good. My cancer markers are all good. Do I have to do this? Do I have to go the whole way? Can I just do six?” Because some people just do six.
She put her hand on my leg and said, “Amanda, you are going to be so grateful once this is done. But yes, you have to finish your full treatment. You will be better off for it.” It’s almost like when you’re begging your mom to stay home from school when you’re sick. She was like, “You’re going to be fine. I know this is hard, but you’re going to be fine.
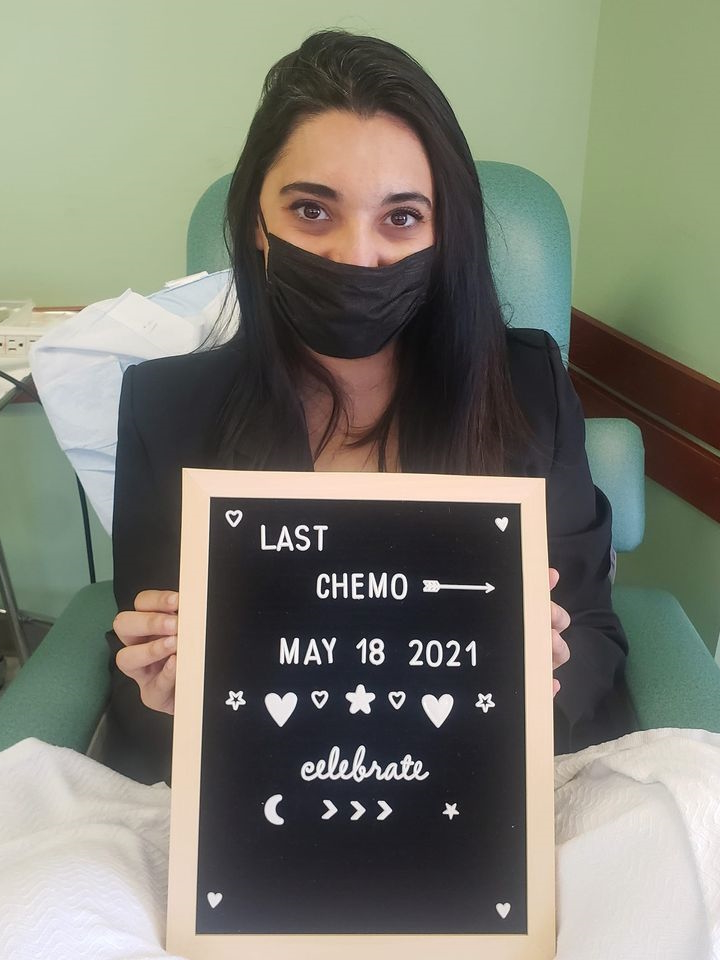
Celebrating the last week of chemotherapy
A week before my last treatment, my friend and I went up to Big Bear. It was this celebratory trip to celebrate my last week of chemo the following Tuesday. It was so much fun.
I wanted to go on this hike and told him, “It has to be a really easy hike. I can’t do much.” He was said, “It’ll be like a chill hike. Don’t even worry about it.”
We go on this hike and it turned into this really strenuous hike. Every five minutes, I would take a 10-minute break just to catch my breath and regain my strength.
When I got to the top of that mountain, I thought, “Wow. Here I am, actively on chemo, I just hiked up, and here I am with these beautiful views. I’m good.”
You can’t believe what you’re capable of. It just felt really good. I went into my last round of chemo with that and said, “Oh, we’re golden. This is good.”
Follow-up protocol
Every six months, I get a CAT scan. I feel like they always find little things in your scan. They found a fibroid in my breast so I have to go in for mammograms and ultrasounds to monitor that. I feel lucky that I’m being watched so carefully and closely because they’ll catch anything.
I go for a colonoscopy every three years. I have one coming up that I requested because they found a polyp in my last one. I want to do one just to make sure I don’t have polyps growing at a rapid rate.
I see my oncologist every three months for blood work and that’s always been good. They’re looking at your cancer biomarkers. Luckily, all my biomarkers have been in the normal range.
They did a lot of genetic testing and they did find out that I do have some mutations that involve colon cancer. There’s a mutation for kidney cancer and skin cancer so they’re keeping an eye on my kidney function, taking a look at my kidneys on scans, making sure I’m going to a dermatologist, [and] getting skin lesions, freckles, and moles checked out.
They’re really keeping a close eye on me. It’s a pain in the butt and not a normal life by any means, but I would rather have that than the alternative. I am monitored very frequently and I’m also on top of it
Dealing with scanxiety
It used to be really bad in the beginning, the first few scans after chemo, because it’s scary. You’re fearing the worst. Is this going to be the day the shoe drops and it comes back? Because it happens.
The fact of the matter is you’ll get a clean scan, but there will likely be something that pops up but doesn’t necessarily mean it’s cancer. I had a spot on my liver show up and I’m thinking, Did it go to my liver? But it was just a cyst. That entails going to get an MRI of your liver done then it resolves itself and it’s no longer there. It was just a cyst.
You remind yourself that our bodies have a bunch of things going on in them at all times and you’re being watched constantly. You’re probably going to see something on a scan.
“There’s a mass in your breast. We’re going to go get an ultrasound of that. Go get a mammogram done. It’s probably nothing,” and it is. It’s just a fibroid. It’s not growing. It’s very common for young women to have them, but because women our age aren’t constantly being scanned, we don’t know that.
I go into scans now with, “Whatever they find, it’s likely nothing. Your biomarkers for every three months are normal.” The biggest thing that I look at [are] my blood work, my labs, and how I’m feeling.
Let’s say something were to come back. Even if they do find something, it’s caught early enough [that] we can do something about it. Nothing will ever be as bad as that first time, in my opinion, because you’re so scared of the unknown.
At this point, scanxiety is real. You don’t ever want to find something, but I’m just like, “Even if they did, it would be caught so early, hopefully, that we could do something about it.”





Importance of advocating for yourself
Doctors went to medical school and so many women and men will take their word to heart and think, “Oh, well, then I’m fine.” Who are they to disagree?
I’m really lucky because my mom’s death — what they said caused my anxiety — lit a fire under my butt even more. This entire time, I just heard her voice in my head like, What are you doing? Go. Get it done. Get it checked out. What would she have wanted me to do?
You’re telling me I’m grieving and that these symptoms are because of grief but in reality, I’m fighting so hard for this because my mom would not want to see me go through anything that she had to go through. I used it as fuel to get it going.
A lot of people don’t even know where to start with self-advocacy. They’re having these symptoms and they don’t even know that a colonoscopy or an endoscopy is what they need. They don’t even know these procedures. They don’t even know a gastroenterologist is a doctor they need to ask for.
Ask for a gastroenterologist. Blood is the main tick-off that something’s wrong. If you’re that concerned, fight for yourself. Tell them you’re having these symptoms because the only way to know is to actually get tested. You can’t go to urgent care and have someone look at your butt and be like, “You’re fine.” You just can’t.
Words of advice
The best thing you can do for yourself is [to] demand answers. Once you get that answer, even if it’s the worst thing, even if it’s cancer, you will feel so much better because the question is gone and they’re going to start taking you seriously.
Demand those answers. Forget about the anxiety of what it is for a second. Forget about the what-ifs. Assume it’s cancer. You’re going to have a plan in place and they’re going to take care of you. Things are going to get moving. You’re going to assimilate to this new life and it’s going to be so much better once you find out. Everything changed after my diagnosis.
It gets better. If you are going through this, there is a light at the end of the tunnel. Everyone’s journey is different, but there is beauty in this awful disease and it opens your eyes to a lot of amazing things.
My patience has grown. My empathy has grown toward people. Be patient with each other. Be patient with yourself.
Listen to your body. Get checked. Stay on top of your health. Don’t think it can’t happen to you because it can. I am a walking example of that. Take care of yourself.
Share This Post
More Colorectal Cancer Patient Stories
Shannon M., Colon Cancer, Stage 1
Cancer Details: Found the cancer as a result of her Lynch Syndrome
1st Symptoms: Routine colonoscopy found polyp
Treatment: Partial colectomy
Hugo T., Colon Cancer, Stage 1
Cancer Details: Diagnosed 2 weeks after 5 years remission from testicular cancer
1st Symptoms: Inflamed bowel
Treatment: Subtotal colectomy, immunotherapy
Rachel B., Sigmoid Colon Cancer, Stage 1
Cancer Details: The sigmoid colon (or pelvic colon) is the part of the large intestine that is closest to the rectum
1st Symptoms: Stomach discomfort, nausea, bloating, blood in stool
Treatment: Colectomy
Chris T., Colon Cancer, Stage 2
Cancer Details: Discovered Lynch Syndrome after genetic testing
1st Symptoms: Found the cancer as a result of family history, early colonoscopy
Treatment: Partial colectomy
Shannon C., Colon Cancer, Stage 2A
Cancer Details: Diagnosed at 29, tested positive for Lynch Syndrome
1st Symptoms: Severe pains after eating
Treatment: Partial colectomy
Barbara M., Colon Cancer, Stage 3
Cancer Details: Family history wasn’t flagged, should have had colonoscopy earlier
1st Symptoms: Stomach discomfort, difficult to process food
Treatment: Colectomy, Chemo (FOLFOX, CAPOX)
Shelley B., Colon Cancer, Stage 3B
Cancer Details: Had no usual first symptoms, found as a result of routine colonoscopy and endoscopy
1st Symptoms: None
Treatment:Partial colectomy, chemotherapy (FOLFOX)
Lindsay D., Colon Cancer, Stage 4
Cancer Details: Diagnosed at 32, cancer spread to ovary and lung
1st Symptoms: Lump in pelvic area, funny-smelling food, weight loss
Treatment: Chemotherapy, colectomy (surgery)
Lee J., Colon Cancer, Stage 4, Recurrence
Cancer Details: Recurrence then remission
1st Symptoms: Discovered stage 4 cancer from unrelated CT scan
Treatment: Neoadjuvant chemo (FOLFOX), hemicolectomy (partial colon surgery), adjuvant chemo (FOLFOX), chemo post-recurrence (FOLFIRI), liver surgery
JJ S., Colorectal Cancer, Stage 4
Age at Diagnosis: 27l
1st Symptoms: Abdominal pain, blood in stool
Treatment: Surgery to remove tumor, chemotherapy, clinical trial of Keytruda (pembrolizumab)
Haley P., Colon Cancer, Stage 3C
Symptoms: Constipation, fatigue, shortness of breath
Treatment: Surgery, chemotherapy
Amanda G., Colon Cancer, Stage 2A
Symptoms: Gurgly stomach, blood in stool, chronic constipation
Treatment: Surgery (hemicolectomy), chemotherapy (CAPOX), Zarxio
Symptoms: Fatigue, anemia, irregular bowel movements, loss of appetite, heavy periods Treatment: Laparoscopy, chemotherapy, partial hysterectomy
Dania M., Colon Cancer, Stage 4, with Liver and Peritoneal Carcinomatosis
Symptoms: Constipation, diarrhea, terrible bloating, swollen belly, as if pregnant
Treatment: Surgery, immunotherapy (KEYTRUDA)
Stephanie K., Colon Cancer, Stage 3
Symptoms: Very bad cramps, bloating, indigestion, burping
Treatment: Surgery, chemotherapy (CAPOX)
Jason A., Colon Cancer, Stage 3B
Symptoms: Abdominal pressure, fatigue, small amounts of blood in stool
Treatment: Surgery (colon resection), chemotherapy (FOLFOX: folinic acid, fluorouracil, and oxaliplatin)
More To Explore
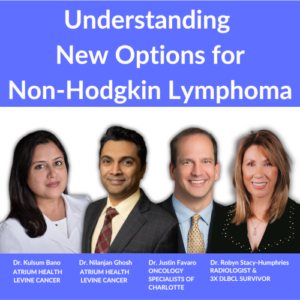
Understanding New Options for Non-Hodgkin Lymphoma
Accessing the Best Care for You or a Loved One: Understanding New Options for Non-Hodgkin Lymphoma
Dr. Kulsum Bano, Dr. Nilanjan Ghosh, and Dr. Justin Favaro discuss the latest advances with 3-time DLBCL survivor and patient advocate Dr. Robyn Stacy-Humphries.

FDA Update: Good News for Multiple Myeloma?
Good news for multiple myeloma patients: FDA committee approves new clinical trial requirement to accelerate approvals on April 12, 2024.
Amanda’s Stage 2A Colon Cancer Story

Amanda was experiencing gastrointestinal symptoms, including bloody stools, which worsened and persisted for almost a year before she finally got a colonoscopy.
She was then diagnosed with stage 2A colon cancer.
She talks about the frustration of not feeling listened to and taken seriously, how important it is to fight for answers and advocate for yourself, and why you should be on top of your health care.
- Name: Amanda G.
- Diagnosis:
- Colon cancer
- Lymphovascular invasion (LVI)
- Staging: 2A
- Initial Symptoms:
- Gurgly stomach
- Blood in stool
- Chronic constipation
- Treatment:
- Surgery: hemicolectomy
- Chemotherapy: CAPOX (capecitabine & oxaliplatin)
- Zarxio
Once you get that answer, even if it’s the worst thing, even if it’s cancer, you will feel so much better because the question is gone and they’re going to start taking you seriously…
Everything changed after my diagnosis.
Introduction
I’m 33 years old. I live in L.A.
I love to go to the movies. I love to go to the beach. I’m a huge sports fan.
I work in entertainment. I’m a model. I also work in events and hospitality.
I love having a good time. I love going out and having adventures. I love to travel.
Pre-diagnosis
Initial symptoms of colon cancer
In August/September 2019, I started getting weird but very light IBS symptoms, like something as simple as a gurgly stomach when I was hungry. But it would be so consistent. It would be every day, something I had never dealt with before. I
I thought, “That’s weird. Is it my diet?” My mind didn’t go to the worst. Those were my early, early symptoms.


Then about a month later, I started seeing blood. That was alarming because, of course, it’s blood. But again, you don’t want to freak out. I gave it a couple of weeks and I thought, “Maybe it’s hemorrhoid. Let’s see if this is consistent and persistent,” and it was.
I didn’t have insurance at the time so I went to my local urgent care where I was told it was probably just hemorrhoids, probably a fissure.
I laughed in the office and said, “I don’t want to have like colon cancer or something,” and the doctor reassured me, “I don’t think you have cancer. I think that’s a little outlandish even to assume that. I think you’re fine.”
I asked how long I could expect to have it. She said, “It depends.” She gave me a really loose-ended answer. “Typically, [in] a couple [of] weeks, it’ll heal up. But if it’s a fissure, like a tear, if you don’t change your diet and eat more fiber, that could be chronic and you could just see blood for months.”
Just keep an eye on it. No solid answer. I wasn’t super thrilled with it. There was no exam done, no blood testing. I took her for her word.
Still dealing with the gurgly stomach but very minor and the bleeding. I just assumed it was a fissure or hemorrhoids. I thought, “Okay, let’s ride this out and see how long this lasts.”
Physical symptoms of grief
In February 2019, I lost my mom suddenly. I wasn’t there. She died of a heart attack 3,000 miles away.
A lot of people who are grieving deal with similar symptoms. Anything you’re going through will manifest itself through your gut. I had a lot of people tell me this was grief.
It wasn’t until I actually saw my first doctor [that] he was like, “You’ve been through a lot. I wouldn’t worry about this. I truly think it’s just grief.”
My primary care told me I needed psychological intervention because I was panicked at that point.
When I got my health insurance in January, I was excited. I got to see a doctor [and] get blood work and all these tests done. He ran the blood work and it all comes back normal, which was a relief for me. That was all he decided he needed to know that I was probably just grieving.
With these symptoms came anxiety. I was never a hypochondriac. It wasn’t until I had these symptoms that I thought, “Something’s wrong,” which I think is your body telling you something’s wrong. There’s no reason for me to doubt that.
This was January 2020. The doctor told me, “There’s nothing wrong with you. You have no family history of colon cancer. You’re so young. This would be very outlandish.”


Possibility of colon cancer
I mentioned it multiple times. I mentioned it at the urgent care. It’s the first thing I thought of when I saw blood. I’m very smart. I’d like to consider that I am very in touch with my body. I understand these things.
When I was growing up, my mom was very ill and I was in and out of hospitals with her. I was comfortable with it [and] I had a head start on maybe what other people wouldn’t.
I thought, “This is a symptom of colon cancer.” I know I’m 29, but I kept bringing it up to the doctors. Their response was, “Oh, that’s silly. There’s no way that would be colon cancer.”
I, of course, Googled my symptoms. At the height of my anxiety and my symptoms, I was on Google almost every night before bed, just trying to find someone else who maybe had gone through this. I would be on YouTube, searching [for] these symptoms.
One of the first few things after Crohn’s disease and ulcerative colitis was colon cancer. I thought, “This isn’t crazy to think.”
The doctor told me, “We can run some tests, like an H. pylori breath test, to see if you have bacteria.” In my mind, it doesn’t make sense what they’re doing, but I’m just going to go through the motions. Let’s tick it off.
Symptoms persisted & intensified
I went on this amazing trip for my 30th birthday in March 2020, weeks before everything shut down. I went to Hawaii and Australia. I booked it because it’s a big birthday. I was going to process my mom’s death on this trip. It was going to be really a beautiful trip for me to say goodbye to this really crazy decade and start my new one.
It was wonderful. I had the best time [and] met a lot of great people, but my symptoms just intensified. It was almost like my body was saying, “Now’s the time. This isn’t going away.”
At this point, I’d been bleeding since September. It’s now March. I was chronically constipated. I couldn’t go to the bathroom and when I could, it was just blood. There was no pain. I was pretty bloated a lot of the time.
I just remember feeling like I couldn’t really enjoy my trip because there was something in the back of my mind saying something was wrong. That was when I thought, “When I get back from Australia, I’m going to insist on getting a gastroenterologist and get this ball rolling because something is seriously wrong.” At this point, I need to fight for it.





Initial appointment with primary care physician
I get back home to L.A. right as everything’s shutting down. Doctors are not seeing patients in person anymore unless it’s considered urgent. Trying to get a hold of any doctor is seemingly impossible. Every appointment is over FaceTime or Zoom.
I got an appointment with my primary care. I said, “These symptoms aren’t going away. In fact, everything seems to be getting worse. I’m really concerned.” He said, “You don’t look sick. If you had cancer, Amanda, you would be losing weight at a rapid pace. Your face would be sunken in.” I just couldn’t believe he said that to me.
I said, “Yeah, if it were bad, if it were end-stage cancer, of course. I’m telling you what I think is happening and you are dismissing everything and not even offering a solution.” Finally, he said, “Your blood work is fine. If it were cancer, you would have anemia.”
My red blood cell count was low normal. My mind went to, Maybe I’m not anemic now but give it a couple of months, that red blood cell count will go lower if it is a tumor. I’m thinking all this and I’m just like, “I can’t go to the bathroom without aid from a pill. I’m seeing blood. Clearly, there’s something blocking everything moving.”
Getting initial testing done
He said, “If you’re really this stressed about it, I will order a stool sample test for you.” This was the, “Aha!” I know this is going to come back abnormal. If anything, this will get things moving. This is how he worded it, “Just to ease your mind, we’ll get you a stool sample test,” and I said, “Perfect. That’s all I want. Let’s just get some proper testing done.”
I get the stool sample test done and that following week, he called me. “We got your results back and it came back positive for blood,” which I knew it would. He goes, “I’m going to refer you to a gastroenterologist,” which is all I wanted in the first place. That should have been done in January.
Initial appointment with a gastroenterologist
Because of COVID and everything being slow-moving, I didn’t get a virtual appointment with my gastroenterologist until May. [At] this time, my symptoms are so bad.
In early May 2020, the Black Lives Matter protests and marches were happening and I wanted to go out and support. I had been cooped up for a few months now so we donned our masks, went to Burbank, and protested. It was a hot day and I remember feeling really dizzy and really faint. At one point, we all got down on the ground and I couldn’t get back up. My vision went blank.
I looked at my friends. They know what I was dealing with and what I was going through. I was very vocal with them. They asked, “Are you okay?” I said, “I’m very dizzy and my vision just blacked out. I need to sit for a second.”
My friend’s husband sat with me while they went on. I found the energy to get up and start walking. My friend was giving me snacks. She said, “Do you need food? Are you dehydrated?” If you’re dealing with these other symptoms, I would have thought I was dehydrated. I would have thought it was hot. We’re in masks. We’re walking. Maybe that’s it.
But I just knew. I remember looking at her and I was like, “I think it’s connected to these symptoms here. I know it’s related.” Even more, I was just ready to see the gastro.

I saw my gastroenterologist and he echoed what my primary care said. “You’re young. You’re a healthy girl. You have no history of colon cancer in your family. These symptoms are very common, Amanda.
“We’ll test you for ulcerative colitis. We’ll test you for Crohn’s,” both very serious chronic diseases that you want to be taken seriously. He said, “But the odds of colon cancer are so slim so don’t let your mind go there.”
How can it not? The symptoms are not getting any better. They are consistent and persistent. He said, “We’ll get you in for a colonoscopy.”
I said, “How fast can we get that?” He said, “We have to get your insurance to approve it.” Trying to get a colonoscopy approved for a 29-year-old girl with no pre-existing anything is seemingly impossible.

Waiting for the colonoscopy to get approved
The referral went in and then it’s almost like it got lost in limbo. I didn’t hear back from my insurance. I never got the authorization in the mail.
I called them and I was going back and forth. They’re like, “Hey, we’re super busy with COVID. Sorry about the delays.” I was on hold for so long.
I remember calling them every single day. “Do you have a referral from this doctor? I need this.” They said, “Oh, well, he didn’t say it was urgent. We’re just taking urgent authorizations. We’re getting through these as fast as we can.”
I’m as patient as I can be and [in] the midst of all of this, anxiety is at an all-time high. I’ve never dealt with anxiety. I’ve never dealt with panic attacks. I sympathize with anyone who deals with it all the time because it is the worst thing that you could deal with.
I felt so alone, lost, and confused. I was like, “I feel like I’m going to die and no one’s listening to me.”
I finally got the colonoscopy scheduled in July. This was May so I had to go two more months.



Feeling like no one was listening & not being taken seriously
It’s hard. You feel all those feelings and associate those thoughts with anxiety. I wanted to turn it off because I thought, “That’s the anxiety talking.” But, at the same time, my body was telling me something completely different.
I would message my friends at 1 a.m. after going to the bathroom and seeing blood. They asked, “Are you in pain?” I said, “I’m not in pain, but I don’t feel right. I just feel like the longer this goes, the worse it’s going to get. I feel like my body, from the inside, is failing and giving up,” especially after that spell in Burbank when we were protesting.
I’m really grateful to have this information to share with people. I have a lot of women, especially in my DMs on Instagram, with concerning symptoms. In one way or another, they found out about my story and reached out to me.
Colonoscopy prep & procedure
The colonoscopy was an interesting experience. I’ve never had one before.
You have to be on an all-liquid diet. You can’t eat any food the day before so you’re hungry. You’re given this prep that you have to drink the day before your procedure. It cleans you out.


It’s not ideal. I wouldn’t say it’s terrible. I don’t want people to fear that. I don’t want people to not get a colonoscopy because they’re afraid of the prep. It’s doable. Have some candies that you can suck on after or even lemonade to chase it.
You’re going to the bathroom all night. You are clearing everything out and you know it’s working. The clearer your bowels, the better the procedure is going to go, and the more accurate it will go. They were like, “You don’t want to come in for your colonoscopy and have it be an incomplete colonoscopy and you have to do this again.”
You go in for your colonoscopy and I was asleep during. I know some people are awake, just groggy. I was completely sedated, but I know that’s not the case for everybody.
The procedure itself was so easy and so quick; in and out in a couple [of] hours. No pain after. You go and can finally eat.
The prep is the worst part and even that I wouldn’t say is bad enough to the point where you shouldn’t go. There are preps that come in pill form. See if your gastroenterologist will prescribe that.
I get one almost every year. [For] the past two years, I’ve gotten them every year and now, they’re going to move me to every three years. Not fun but not the worst thing.
Finally getting a colonoscopy
I go for my colonoscopy in July and, of course, there [are] hoops and hurdles to get there. It finally gets approved.
We’re [at] the height of COVID. Now come COVID tests and all those preliminary appointments you have to get.
I remember being like, “Okay, I’ve gotten this far. We’re now almost a year of symptoms and I’m at the homestretch. I’m going to get my answers.” Waiting for my friend to pick me up to take me to the hospital, I was like, “I’m going to get my answer today.” This has been months and months of absolute mental and physical torture.
I go to the hospital and have my colonoscopy. I deal with things with humor. “Hey, am I the youngest patient you’ve ever had?” All the nurses were lovely. They were so kind and super reassuring, like, “Hey, you’re going to be fine. Don’t sweat it.”
Once they hook up the drugs to you and you’re loopy, you’re golden. I’m like, “Let’s just get this going. I’ve been waiting for this.”
I expected the worst but also don’t think I was prepared to hear it because you hope for the best. You know in the back of your mind, but you never expect what you’re going to hear.
When I woke up from the colonoscopy, I remember looking around the room. The nurses were there and they were just quiet. “Good morning, Amanda. You’re all done.” I’m groggy. I don’t even know what questions to ask. I’m just like, “Great. Awesome. Cool.”


Finding a large tumor during the colonoscopy
The doctor comes in. I know doctors are very clinical and to the point, but it was just like, “We found a large tumor in your sigmoid colon. I biopsied it. Call me tomorrow for the results.”
I’m high as a kite on these drugs. You couldn’t have told me at a better time because [at] that moment, I was like, “Whatever. Tumors can be benign, right? Great. I have my answer.” I’m looking around at the nurses and like, “Hey, it’s probably benign. At least I have my answer.”
Then you start coming off the drugs. One of my nurses was lovely. He wheeled me out when my friend came to pick me up and I was like, “What happens now with the tumor in my colon?” He goes, “This happened to my friend and they’ll just cut the tumor out, resect you, and you’re going to be golden. You’re going to be fine.”
On the drive home, I was telling my friends and they were super supportive. “You’ve got this. You’ve got your answer, on to the next.” This whole time, I’m rationalizing in my brain. Tumors can be benign and they often are. Maybe it’s just a benign tumor.
It was a large tumor. We didn’t know how large until my surgery, which is crazy. It had grown in my colon. I remember being like, “I have to wait for these results,” and luckily it was just the next day.
Diagnosis
Getting the results of the colonoscopy
I remember being in bed, my head just spinning. I’d already called my family back in Massachusetts and told them what was going on. They were like, “Keep us posted. Tumors are often benign. We have all the faith you’re going to be okay.” I was like, “Yeah, I think I’m going to be okay but at least I know I have a tumor.”
My doctor called and he goes, “Pathology came back and it is cancer. Please come to my office right away for the next steps.”
You are never prepared to hear that, but in the same sense, I knew. This whole time I knew. I had been saying colon cancer since September. It wasn’t new information. Everything checks out.
I was laying down when I got the phone call. I sat up immediately and was like, “Okay, do I come now?” He was like, “Yeah, come now.”
Follow-up appointment with the gastroenterologist
Immediately call my friend and told him it’s cancer. He was like family to me out here. I love him to death. He was like, “What are we doing?” I said, “I need to go to the doctor.”
He picked me up and brought me to the office. That was an interesting car ride and visit. I was just very quiet and shocked.
Things just start going in your mind. How long did I let this go? Did I not fight hard enough for myself? My symptoms have been going on since September of last year. Surely, it’s all over my body by now.
We get into the office and he gives me all my paperwork. He gives me the next steps. He goes, “I’m going to refer you to a surgeon. If the cancer has spread, you will need chemo. If it’s localized, it’ll just be surgery.” It was a lot of information all at once, the same day I heard the diagnosis.
I remember being looked at by everyone in the office as I was leaving. Just diagnosed with cancer and I’m just like, “Okay, bye!” Then you get a lot of, “We’re praying for you.” As nice as that is, you’re like, “Oh, this is going to be a whole thing. This is scary.”
Treatment
Surgery
My surgery was another hurdle. I had to keep on my insurance company to approve the surgery. I finally got my surgery a month after my colonoscopy, which in hindsight is about right. It just felt like forever.
They didn’t scan me prior to surgery. I didn’t find out my stage until after surgery when I met with my oncologist.
The surgeon took out the tumor, said it was a large tumor, told me he poked around in there, [and] said there was no visible evidence of metastasis. He said the liver looked good. Everything else looked clear.
He was like, “I think you caught this early, but obviously, you have to have a scan and meet with an oncologist to be sure.” He said my lymph nodes were clear, which was a huge relief. He tested 28 lymph nodes. All great news.


Hemicolectomy procedure
I had a hemicolectomy; I just say a colon resection. They removed my sigmoid colon. You have your large intestine, your small intestine, and the sigmoid colon connects to your rectum so it’s right down there.
They went in laparoscopically. It was all done through two little incisions. They went in and took out that part of the colon and resected it.
My surgeon warned me I might need a colostomy bag temporarily. He was like, “You might have to have a colostomy bag when you wake up from surgery. If you feel one, don’t freak out. It will be reversed. We’re going to do our best to help make this a clean resection for you.”
All I’m thinking [about] is my pride. I’m 30 years old. I can’t live my life with an ostomy bag. After researching and meeting people, you can have one permanently, live a full life, and be fine. It’s not a big deal. You would much rather have one than not be here from cancer.
But in my head, it just sounded like, Oh my gosh, say goodbye to my social life. It’s such a lifestyle change. It’s the first thing I felt for when I woke up, but I didn’t have one.
He came in and was like, “The resection was clean. Everything went well. The tumor was much bigger than anticipated. The colonoscopy picture showed that it was large. It wasn’t until I went in there that it was really large.”
I was really lucky. I had a great surgeon. I had the chief surgeon of the hospital perform my surgery. He was an amazing surgeon. Everything healed up nicely.
This whole experience, I’ve been very, very, very lucky because I know every case is unique, but my case could have been so much worse in so many different areas.
Initial appointment with the oncologist
I was recovering at my friend’s place. A couple of weeks later, I met with my oncologist at Cedars and he was lovely. Dr. Gong was the best doctor that I’d had up to this point. The most caring, the most understanding, and empathetic. He’s amazing. He’s the one who staged me.
He goes over my pathology report. I’m there with my friend and I’m terrified. You just don’t want to hear the worst, like terminal, stage 4, not curable. You don’t want to hear those words, but you have to prepare yourself for those words. You have to brace yourself.
First, he said, “Before I say anything, I’m really sorry this happened to you. This should have never happened to you,” and I just started sobbing. I just felt like this doctor cares and is taking me seriously. It was overwhelming and I really felt it. I’m like, “This is the person who should be a doctor. This guy cares.”

Discussing the pathology report
He was like, “I looked at your pathology report and, Amanda, it looks really, really good. You got it in time.” I started crying. He went over everything. He showed me the pathology report. He told me what everything meant.
He was like, “We don’t know until you get scanned, but where I would stage you right now is stage 2A.” Staging for colon cancer starts at stage 0, then goes 1, 2, 3, 4, and then substages A, B, [and] C for every stage. I was [in] early stage two.
The staging goes by how much of the colon wall the tumor chewed through. On my pathology report, my tumor had chewed through the first layer, which makes it stage 2A as opposed to stage 1C. It was just starting to chew through and it was very large.
The sizing is the T so on a pathology, it would be T3 and that can go up to 4. The sizing of the tumor and the stage of the tumor is different. It was T3, but stage 2.
I remember being like, “Great. I caught this in time.” It was very emotional. I was with my friend. I was so happy, so relieved. The surgery was done. It was out of me.
Lymphovascular invasion (LVI)
He goes, “You have something called lymphovascular invasion. They didn’t find cancer in your lymph nodes, but they found the DNA of cancer in blood vessels surrounding the tumor and the tissue, which means you’re at higher risk for this returning.”
I was like, “Okay, what do we do?” He was like, “There’s no real evidence of your cancer anywhere in your body, but you have the option to proceed with chemo if you want.
“Obviously, it’s your choice. You don’t have to do chemo. But I highly recommend that you do to reduce the odds of this coming back.” That’s all I needed to hear.
I was like, “Of course, I’m going to do chemo.” Again, I don’t think I was really ready for what that meant, but I was just like, “Sure, whatever lowers my chances. I don’t want to ever deal with this again so if I have to be sick for a little bit…”
Mind you, being sick for a little bit isn’t just being sick. It’s the worst thing you can put your body through, but I was just so ready to go and get that moving.


Chemotherapy
CAPOX chemotherapy for colon cancer
I told my oncologist I wanted to start chemo and that was in September. I’m jumping through hurdles with my insurance company again.
I’m feeling great at this point. I’m recovered from my surgery. I feel back to myself. I’m not bleeding anymore. I feel great. This is now October/November.
I felt crazy because I’m fighting for chemo and I feel like I don’t need it. My scan was clear in October. I need to keep this from returning, but I haven’t felt this good in so long.
Finally, it got approved. My course of treatment was CAPOX, which is oxaliplatin, the IV chemo, and then Xeloda, which is the pill form of chemo.
My oncologist wanted to do the combo. He’s like, “This is very common. This is one of the most effective routes for colon cancer to keep this from recurring.” He also told me it was one of the most toxic on the body and it’s not fun.
I started in December. I got my port placed the day before chemo, which was the easiest thing. When I got it removed, my doctor let me keep it so I have it as a souvenir. I’m like, “I want this. I paid for it. It got me through chemo. That’s mine.”
My anxiety about that was more than chemo. I was freaking out. I joined a colon cancer group on Facebook. I remember putting a post up and was like, “I’m so scared to have this port placed because it goes under your skin, on your chest. That seems insane to me.”
Everyone was like, “Oh, yeah, it’s an easy procedure. You’re awake for it.” I was like, “Oh, that sounds like a nightmare. I don’t know that I can do that.” They’re like, “Think of all you’ve dealt with up to this point. This is nothing,” and it really was.
If anyone is in the early stages of their cancer battle and is afraid of getting a port, let me put your mind at ease. You feel nothing. You’re loopy. It’s done in 20 minutes. These doctors do a bunch of them a day. It’s so easy and you’ll be grateful for it. It will save your veins. Trust me.
I was doing chemo every other week for six months. I would go in every other Tuesday. I would do three pills in the morning and three pills at night. I would start my chemo, take my three pills, have my chemo, go home, take my pills at night, [and] go to sleep.
The day after chemo, I would go back to the oncologist’s office and get a shot called Zarxio to boost my white blood cells. Chemo kills your white blood cells so they want to make sure you don’t get sick. They want to make sure that you can come back for chemo the following week and be good.

That shot made me feel so bad, so ill. It would make my body ache. I don’t know what it is about that shot, but my entire body would feel like it got hit by a truck.
I would go in for that shot then they would hook me up to hydration so I’d be at chemo on Wednesday just for the hydration drip through your port. Then after that, you’re good for two weeks.

Side effects from CAPOX chemotherapy
The five days following chemo are the worst and it’s cumulative.
The first week I went, I remember thinking, This isn’t so bad. This is 2020-2021. We couldn’t have visitors. We couldn’t have people sit with us, which is fine. I was asleep anyway for the most part, on my phone, or listening to music.
I remember leaving the cancer center that first time being like, “That wasn’t bad at all. I actually feel fine.” They’re like, “Just go home and rest.” I went home and that’s when it starts coming.
You can’t even lift up your arms. The nausea is terrible. There’s neuropathy. They warned me beforehand of all the potential side effects of these drugs. They talked about neuropathy and were like, “Don’t touch anything cold.” You listen to them, but you don’t really rationalize it.
I went into my fridge, grabbed juice, and it felt like a singe. When you touch something cold, it feels like a singe almost. Think of when you get shocked but like a permanent shock and it’s like singeing the tips of your fingers. It would go away when you stop touching something cold. That was the first few cycles.
As the weeks went on and I had more treatments, it became something completely different. My feet and my legs are starting to get numb. I would compare your feet and legs to when your foot falls asleep and you go up to walk — that sensation, that’s what it feels like. Almost like a dead leg.
My fingertips felt completely different. They felt numb and tingly. I didn’t have any pain with it. I know a lot of people have severe neuropathy pain and have to take gabapentin for it.
Again, this is why I say I’m very lucky in all these little aspects of my journey compared to others. I never had pain and I still don’t have pain and I’m really grateful for that because I did 12 rounds. I did it for six months. I got out pretty unscathed.
I still have some numbness in my feet, but my fingertips are back to normal. My oncologist told me, “We don’t know. Neuropathy can be permanent. It can get worse. It can get better. You can try acupuncture for it,” but my hands are fine and my feet are pretty okay. There’s no pain so I’m fine.
The side effects were cumulative. This is the part of cancer where unless they’ve gone through it themselves or seen someone go through it, people don’t really know how awful it is.
This is the pandemic so no one was really seeing each other. I was talking to my friends through FaceTime. I’d be on my bed, be on the pillow, and would just look terrible. My voice would be so soft.

I’d be like, “I ate a potato today.” It’s all I could manage to get down. Your appetite is gone and you’re so sick, but you can’t actually throw anything up because you’re not eating anything. It’s terrible.
That journey made me understand why people who are on chemo for life [want to] stop because it’s not a quality of life. I get it and I would never judge someone for that decision.
Before, I might have been like, “Why would you stop fighting? That makes no sense. There’s this treatment out there that can prolong your life.” You get a taste of it and it’s like, “Oh, well, what kind of life is that?” You would rather have a quality of life.
It was quite the journey. A week after chemo, I would start feeling better. I would start feeling like myself. I would always take that week to be outside, have lots of yummy food, and be with my friends to the capacity that I could.
I’m trying not to get COVID because COVID meant I couldn’t have chemo. I would also be putting everyone else in that cancer center at risk so I took it very seriously. I didn’t want to get sick not just for me. I knew I would likely be okay, but there are a lot of people much older than me, much sicker than me who couldn’t afford to get COVID.
I kept quite a distance from friends, spent a lot of time outside, and would go to the beach a lot with my friends. That felt like a safe place to be — outside, away from people — and that became our little sanctuary. It was just nice to feel normal again. I think that’s what you just want to feel is normal.
I keep my stickers on the wall of every treatment that I had. Every time you go in, you get a new sticker. I would put them around my calendar and count them. Those stickers were a visual for me. When I was in bed feeling my worst, I was like, “Okay, you’ve got six stickers, you just need six more. You’re halfway there.”
My nurse practitioner would check on me in my chemo chair. I was four or five chemos in at that point. I remember asking, “Do I have to do all of this? My scans are good. My blood work’s good. My cancer markers are all good. Do I have to do this? Do I have to go the whole way? Can I just do six?” Because some people just do six.
She put her hand on my leg and was like, “Amanda, you are going to be so grateful once this is done. But yes, you have to finish your full treatment. You will be better off for it.” It’s almost like when you’re begging your mom to stay home from school when you’re sick. She was like, “You’re going to be fine. I know this is hard, but you’re going to be fine.”


Celebrating the last week of chemotherapy
A week before my last treatment, my friend and I went up to Big Bear. It was this celebratory trip to celebrate my last week of chemo the following Tuesday. It was so much fun.
I wanted to go on this hike and I was like, “It has to be a really easy hike. I can’t do much.” He was like, “It’ll be like a chill hike. Don’t even worry about it.”
We go on this hike and it turned into this really strenuous hike. Every five minutes, I would take a 10-minute break just to catch my breath and regain my strength.
When I got to the top of that mountain, I was just like, “Wow. Here I am, actively on chemo, I just hiked up, and here I am with these beautiful views. I’m good.”
You can’t believe what you’re capable of. It just felt really good. I went into my last round of chemo with that and I was like, “Oh, we’re golden. This is good.”



Follow-up protocol
Every six months, I get a CAT scan. I feel like they always find little things in your scan. They found a fibroid in my breast so I have to go in for mammograms and ultrasounds to monitor that. I feel lucky that I’m being watched so carefully and closely because they’ll catch anything.
I go for a colonoscopy every three years. I have one coming up that I requested because they found a polyp in my last one. I want to do one just to make sure I don’t have polyps growing at a rapid rate.
I see my oncologist every three months for blood work and that’s always been good. They’re looking at your cancer biomarkers. Luckily, all my biomarkers have been in the normal range.
They did a lot of genetic testing and they did find out that I do have some mutations that involve colon cancer. There’s a mutation for kidney cancer and skin cancer so they’re keeping an eye on my kidney function, taking a look at my kidneys on scans, making sure I’m going to a dermatologist, [and] getting skin lesions, freckles, and moles checked out.
They’re really keeping a close eye on me. It’s a pain in the butt and not a normal life by any means, but I would rather have that than the alternative. I am monitored very frequently and I’m also on top of it.

Dealing with scanxiety
It used to be really bad in the beginning, the first few scans after chemo, because it’s scary. You’re fearing the worst. Is this going to be the day the shoe drops and it comes back? Because it happens.
The fact of the matter is you’ll get a clean scan, but there will likely be something that pops up but doesn’t necessarily mean it’s cancer. I had a spot on my liver show up and I’m thinking, Did it go to my liver? But it was just a cyst. That entails going to get an MRI of your liver done then it resolves itself and it’s no longer there. It was just a cyst.
You remind yourself that our bodies have a bunch of things going on in them at all times and you’re being watched constantly. You’re probably going to see something on a scan.
“There’s a mass in your breast. We’re going to go get an ultrasound of that. Go get a mammogram done. It’s probably nothing,” and it is. It’s just a fibroid. It’s not growing. It’s very common for young women to have them, but because women our age aren’t constantly being scanned, we don’t know that.
I go into scans now with, “Whatever they find, it’s likely nothing. Your biomarkers for every three months are normal.” The biggest thing that I look at [are] my blood work, my labs, and how I’m feeling.
I’m like, “You’re feeling fine. You have no symptoms of anything. You were just scanned six months ago. You just had blood work three months ago. Everything was fine. Everything was normal. There’s nothing out of whack here so there’s no reason for you to go into this scan thinking anything.
“Let’s say something were to come back. Even if they do find something, it’s caught early enough [that] we can do something about it. You’ve done this before.” Nothing will ever be as bad as that first time, in my opinion, because you’re so scared of the unknown.
At this point, scanxiety is real. You don’t ever want to find something, but I’m just like, “Even if they did, it would be caught so early, hopefully, that we could do something about it.”


Importance of advocating for yourself
Doctors went to medical school and so many women and men will take their word to heart and be like, “Oh, well, then I’m fine.” Who are they to disagree?
I’m really lucky because my mom’s death — what they said caused my anxiety — lit a fire under my butt even more. This entire time, I just heard her voice in my head like, What are you doing? Go. Get it done. Get it checked out. What would she have wanted me to do?
You’re telling me I’m grieving and that these symptoms are because of grief but in reality, I’m fighting so hard for this because my mom would not want to see me go through anything that she had to go through. I used it as fuel to get it going.
A lot of people don’t even know where to start with self-advocacy. They’re having these symptoms and they don’t even know that a colonoscopy or an endoscopy is what they need. They don’t even know these procedures. They don’t even know a gastroenterologist is a doctor they need to ask for.
Ask for a gastroenterologist. Blood is the main tick-off that something’s wrong. If you’re that concerned, fight for yourself. Tell them you’re having these symptoms because the only way to know is to actually get tested. You can’t go to urgent care and have someone look at your butt and be like, “You’re fine.” You just can’t.
Words of advice
The best thing you can do for yourself is [to] demand answers. Once you get that answer, even if it’s the worst thing, even if it’s cancer, you will feel so much better because the question is gone and they’re going to start taking you seriously.
Demand those answers. Forget about the anxiety of what it is for a second. Forget about the what-ifs. Assume it’s cancer. You’re going to have a plan in place and they’re going to take care of you. Things are going to get moving. You’re going to assimilate to this new life and it’s going to be so much better once you find out. Everything changed after my diagnosis.
It gets better. If you are going through this, there is a light at the end of the tunnel. Everyone’s journey is different, but there is beauty in this awful disease and it opens your eyes to a lot of amazing things.
My patience has grown. My empathy has grown toward people. Be patient with each other. Be patient with yourself.
Listen to your body. Get checked. Stay on top of your health. Don’t think it can’t happen to you because it can. I am a walking example of that. Take care of yourself.



Inspired by Amanda’s story?
Share your story, too!
Colon Cancer Patient Stories
Shannon M., Colon Cancer, Stage 1
Cancer Details: Found the cancer as a result of her Lynch Syndrome
1st Symptoms: Routine colonoscopy found polyp
Treatment: Partial colectomy
Hugo T., Colon Cancer, Stage 1
Cancer Details: Diagnosed 2 weeks after 5 years remission from testicular cancer
1st Symptoms: Inflamed bowel
Treatment: Subtotal colectomy, immunotherapy
Rachel B., Sigmoid Colon Cancer, Stage 1
Cancer Details: The sigmoid colon (or pelvic colon) is the part of the large intestine that is closest to the rectum
1st Symptoms: Stomach discomfort, nausea, bloating, blood in stool
Treatment: Colectomy
Chris T., Colon Cancer, Stage 2
Cancer Details: Discovered Lynch Syndrome after genetic testing
1st Symptoms: Found the cancer as a result of family history, early colonoscopy
Treatment: Partial colectomy
Shannon C., Colon Cancer, Stage 2A
Cancer Details: Diagnosed at 29, tested positive for Lynch Syndrome
1st Symptoms: Severe pains after eating
Treatment: Partial colectomy
Barbara M., Colon Cancer, Stage 3
Cancer Details: Family history wasn’t flagged, should have had colonoscopy earlier
1st Symptoms: Stomach discomfort, difficult to process food
Treatment: Colectomy, Chemo (FOLFOX, CAPOX)
Shelley B., Colon Cancer, Stage 3B
Cancer Details: Had no usual first symptoms, found as a result of routine colonoscopy and endoscopy
1st Symptoms: None
Treatment:Partial colectomy, chemotherapy (FOLFOX)
Lindsay D., Colon Cancer, Stage 4
Cancer Details: Diagnosed at 32, cancer spread to ovary and lung
1st Symptoms: Lump in pelvic area, funny-smelling food, weight loss
Treatment: Chemotherapy, colectomy (surgery)
Lee J., Colon Cancer, Stage 4, Recurrence
Cancer Details: Recurrence then remission
1st Symptoms: Discovered stage 4 cancer from unrelated CT scan
Treatment: Neoadjuvant chemo (FOLFOX), hemicolectomy (partial colon surgery), adjuvant chemo (FOLFOX), chemo post-recurrence (FOLFIRI), liver surgery
JJ S., Colorectal Cancer, Stage 4
Age at Diagnosis: 27l
1st Symptoms: Abdominal pain, blood in stool
Treatment: Surgery to remove tumor, chemotherapy, clinical trial of Keytruda (pembrolizumab)
Haley P., Colon Cancer, Stage 3C
Symptoms: Constipation, fatigue, shortness of breath
Treatment: Surgery, chemotherapy
Amanda G., Colon Cancer, Stage 2A
Symptoms: Gurgly stomach, blood in stool, chronic constipation
Treatment: Surgery (hemicolectomy), chemotherapy (CAPOX), Zarxio
Symptoms: Fatigue, anemia, irregular bowel movements, loss of appetite, heavy periods Treatment: Laparoscopy, chemotherapy, partial hysterectomy
Dania M., Colon Cancer, Stage 4, with Liver and Peritoneal Carcinomatosis
Symptoms: Constipation, diarrhea, terrible bloating, swollen belly, as if pregnant
Treatment: Surgery, immunotherapy (KEYTRUDA)
Stephanie K., Colon Cancer, Stage 3
Symptoms: Very bad cramps, bloating, indigestion, burping
Treatment: Surgery, chemotherapy (CAPOX)
Jason A., Colon Cancer, Stage 3B
Symptoms: Abdominal pressure, fatigue, small amounts of blood in stool
Treatment: Surgery (colon resection), chemotherapy (FOLFOX: folinic acid, fluorouracil, and oxaliplatin)